Back to Journals » Clinical Ophthalmology » Volume 18
Redefined Formula for Anterior Chamber Volume Calculation: Quantitative Analysis of Biometric Parameters Across Ocular Pathologies
Authors Zemitis A , Rizzuto V, Lavrinovica D, Vanags J, Laganovska G
Received 6 September 2024
Accepted for publication 11 December 2024
Published 27 December 2024 Volume 2024:18 Pages 3989—3998
DOI https://doi.org/10.2147/OPTH.S495068
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Arturs Zemitis,1,2 Vincenzo Rizzuto,1– 4 Diana Lavrinovica,1,2 Juris Vanags,1,2 Guna Laganovska1,2
1Riga Stradins University, Department of Ophthalmology, Riga, Latvia; 2Pauls Stradins Clinical University Hospital, Clinic of Ophthalmology, Riga, Latvia; 3School of Advanced Studies, Centre for Neuroscience, University of Camerino, Camerina, Italy; 4Latvian American Eye Centre, Riga, Latvia
Correspondence: Arturs Zemitis, Department of Ophthalmology, Riga Stradins University, Dzirciema 16, LV-1007, Riga, Vidzeme, Latvia, Email [email protected]
Purpose: This study evaluates the discrepancies between ACV measurements obtained from the Heidelberg Anterion and Zeiss IOLMaster 700 and investigates the significance of ACV and other ocular biometry parameters.
Patients and Methods: To investigate intraocular fluid circulation, a robust formula was developed for ACV measurement using the Zeiss IOLMaster 700. A pilot study was conducted to validate this formula, which relied on WTW, CCT, and ACD. The formula used was ACV = (RAC)^2 × (CCD) × 1.51. ACV measurements showed a median of 155.38 (IQR = 131.15– 180.06) for the Heidelberg Anterion and 144.11 mm³ (IQR = 125.62– 159.81) for the Zeiss IOLMaster 700. The intraclass correlation coefficient (ICC) for ACV was 0.908, indicating excellent agreement between devices.
Results: Intraocular fluid volume was significantly lower in eyes with PEXS compared to those without. Eyes with PEX had an ACV of 133 ± 28.3 mm³ versus 142 ± 30.7 mm³ in non-PEX eyes, a statistically significant difference (t (196) = − 2.09, p = 0.038, d = − 0.301). Significant differences were also observed in ACD and AL between PEX and non-PEX eyes, with PEX eyes showing reduced measurements.
Conclusion: Our findings reveal that age-related changes in ACD and ACV are significant, with the redefined formula showing excellent agreement with AS-OCT methods. Eyes with PEX exhibit reduced ACD, ACV, and AL measurements. Additionally, an accessible method for ACV measurement, not relying on Pentacam or AS-OCT, would be valuable, particularly in developing countries, to facilitate broader clinical research.
Plain Language Summary: Our study examines the differences in measuring aqueous humor volume in the eye using two devices, the Heidelberg Anterion and the Zeiss IOLMaster 700. Aqueous humor is the clear fluid in the front part of the eye, which circulates at a rate of 1.0% to 1.5% per minute. We refined a formula to calculate the volume of this fluid using the Zeiss IOLMaster 700, based on specific eye measurements. We found that the volume measurements from both devices were very similar, showing a strong agreement. The study also discovered that eyes with pseudoexfoliation syndrome (PEXS), a condition affecting the eye, had significantly lower fluid volume compared to eyes without the condition. This was also true for other eye measurements like anterior chamber depth (ACD) and axial length (AL). These findings are important because they show that simpler and more accessible methods for measuring fluid volume in the eye can be used effectively, especially in developing countries where advanced equipment may not be available. The study highlights the changes in eye measurements with age and how the new formula aligns well with existing methods. Overall, eyes with PEX show reduced measurements in various eye parameters.
Keywords: anterior chamber volume, pseudoexfoliation, IOL power calculation, Heidelberg Anterion, performance measures
Introduction
Aqueous humor is a transparent, watery fluid that occupies the anterior and posterior chambers of the eye.1 It serves to nourish the avascular structures, such as the lens and cornea, and is critical in maintaining intraocular pressure.2 This fluid is produced by the ciliary body’s pigmented and non-pigmented epithelium, circulates through the pupil into the anterior chamber, and is predominantly drained via the trabecular meshwork and Schlemm’s canal, with a smaller fraction exiting through the uveoscleral outflow pathway.3 Aqueous humor formation involves three primary mechanisms: diffusion, ultrafiltration, and active secretion.4
Several pathologies relate to aqueous humor dynamics, including glaucoma,5 ocular hypertension,6 hypotony,7 uveitis,8 angle-closure glaucoma,9 pseudoexfoliation syndrome,10 and neovascular glaucoma.11 Aqueous humor dynamics are measured through techniques such as tonometry, gonioscopy, pachymetry, aqueous humor outflow facility measurement, aqueous humor production rate estimation, and imaging modalities like optical coherence tomography (OCT) and ultrasound biomicroscopy.12
The turnover rate of aqueous humor within the anterior chamber is estimated to range from 1.0% to 1.5% per minute, corresponding to a measured flow rate of 2.4 ± 0.6 mm³/min, thereby inferring an anterior chamber volume (ACV) of approximately 160 to 240 mm³.13 The production and drainage rates of aqueous humor are not routinely measured in clinical practice due to their limited diagnostic utility.14 Significant nocturnal changes in aqueous humor dynamics in healthy mature humans include reductions in aqueous flow, outflow facility, and possibly uveoscleral outflow.15
Numerous methodologies have been proposed for calculating the ACV based on the dimensions obtained from photographically recorded optical sections of the eye.16–21 Although most of these methods were developed approximately 50 years ago, the advent of modern ophthalmological equipment necessitates a more straightforward approach to calculating the ACV.
Aqueous humor circulates from the posterior to the anterior segment of the eye, with its production and drainage extensively studied, though its volume has not been as thoroughly examined. While the ACV has not been directly linked to other ocular pathologies, the study of its metabolomics and composition can provide valuable insights into the various mechanisms operating within the eye.22
In our study, we evaluated the discrepancies between measurements obtained from the Heidelberg Anterion (Heidelberg Engineering, Germany) and the Zeiss IOLMaster 700 (Carl Zeiss AG, Germany). We also refined a formula for calculating intraocular fluid volume and conducted a pilot study to validate this formula. Additionally, we compared measurement differences between a control group and a cataract group. Subsequently, we investigated the significance of ACV and various ocular biometry parameters in relation to a spectrum of ocular comorbidities.
Materials and Methods
To thoroughly investigate intraocular fluid circulation in the eye, it was essential to develop a robust formula to aid our research. Although our hospital is equipped with a Heidelberg Anterion23 anterior segment OCT imaging device, utilizing this machine for ACV calculations would be time-consuming and ultimately impractical. Therefore, we opted to use the Zeiss IOLMaster 70024 for this analysis.
All data for our study were collected using the Zeiss IOLMaster 700, as it was already integrated into the routine examination process for patients undergoing cataract surgery who consented to participate in the study. Consequently, we first needed to establish a reliable method for obtaining ACV measurements using this machine, ensuring accurate and efficient data collection for our research.
During our endeavors, we conducted a pilot study to assess the sufficiency of our formula for analyzing ACV in the eye. This preliminary study included 30 participants, comprising both cataract patients and a younger control group. The study comprised 18 patients in the cataract group and 12 in the control group. The mean age of the cataract group was 73.3 years (± 8.22), ranging from 57 to 88 years. In contrast, the control group had a mean age of 32.2 years (± 7.73), with ages ranging from 26 to 48 years. The objective was to determine if we could develop a reliable formula for ACV measurement using only white-to-white corneal diameter (WTW), central corneal thickness (CCT), and anterior chamber depth (ACD). The ACD, measured using the Heidelberg Anterion AS-OCT device, was defined as the distance from the central anterior corneal epithelium to the anterior surface of the crystalline lens capsule.25
To estimate the ACV using Zeiss IOLMaster 700 ocular biometry parameters, we conducted an extensive literature review to identify an appropriate formula. Our investigation included articles from the 1970s and 1980s that described various optical methods for measuring ACV. We employed the empirical formula initially developed by Max Heim in 194126 and later utilized by Tomlinson et al in 197427 and Johnson et al28 to address our research needs.
Central to our study, the ACV was computed using the following parameters:
- The radius of the anterior chamber (RAC) was established based on the WTW distance.
- The central chamber depth (CCD) was derived from the disparity between the ACD and the CCT.
The WTW distance represents the horizontal measurement across the cornea from one limbus to the other, effectively measuring the diameter of the anterior chamber. This measurement is typically acquired using devices such as the Zeiss IOLMaster 700. Given that the WTW distance corresponds to the diameter, dividing it by two yields the RAC. The radius, being half of the diameter, is crucial for subsequent calculations involving volume. The CCD is determined by subtracting the CCT from the ACD.
This relationship was formalized in the formula:
This formula is derived from the correlation between ACV and ACD, which has been demonstrated to explain approximately 85% of the variation in ACV across multiple studies employing OCT for volume estimation.29,30 ACV can be effectively quantified using both Pentacam (Oculus Optikgeräte GmbH, Germany) and anterior segment optical coherence tomography (AS-OCT), as demonstrated by their reliability. Nonetheless, the lack of substantial agreement between these measurements precludes their interchangeability.31
The intraclass correlation coefficient (ICC) was calculated using a two-way mixed effects model to evaluate the consistency and reliability of the measurements obtained from the two devices. This approach is widely recognized for assessing agreement between different raters or instruments.32,33 The specific model employed for the ICC calculation was “inter-rater reliability, two-way mixed effects, single rater, absolute agreement.” This methodologically aligns with the guidelines provided by Koo and Li,32 which recommend appropriate methods for ICC calculation in inter-rater reliability studies.
We conducted a comparative analysis of the measurements obtained using the Heidelberg Anterion device against the volumes calculated from the Zeiss IOLMaster 700 data, employing the specified formula as outlined earlier. Descriptive statistics, including the median and interquartile range (IQR), were computed for each parameter as assessed by both raters. These statistics provide a detailed summary of the central tendency and dispersion, ensuring a comprehensive depiction of the measurement data.34
To compare the distributions of the measurements from the Heidelberg Anterion and the Zeiss IOLMaster 700, we employed the Mann–Whitney U-test. This non-parametric test is appropriate for comparing two independent groups, especially when the data do not follow a normal distribution.35 The threshold for statistical significance was set at a p-value of < 0.05. This threshold was used to determine whether the results were statistically significant in our analysis.36 Additionally, Levene’s test was performed to assess the homogeneity of variances between the measurements from both devices, ensuring the assumption of equal variances was met. Evaluating the homogeneity of variances is critical for validating many statistical analyses, as it enhances the reliability of subsequent comparative analyses.37 This assessment was crucial in validating our methodology and ensuring the accuracy and reliability of ACV measurements in our research. The measurements are shown in Table 1.
 |
Table 1 Comparison of Ocular Biometry Parameters Between Heidelberg Anterion and Zeiss IOLMaster 700 |
For the WTW measurements, the Heidelberg Anterion device reported a median of 11.60 mm (IQR = 11.33–11.88), whereas the Zeiss IOL Master reported a median of 11.80 mm (IQR = 11.53–12.08). The ICC for WTW was 0.808, with a 95% confidence interval ranging from 0.63 to 0.90, indicating moderate agreement between the two devices. The Mann–Whitney U-test indicated a significant difference between the devices (p = 0.0056), while Levene’s test confirmed the homogeneity of variances (p = 0.103).
For CCT measurements, the Heidelberg Anterion device reported a median of 0.53 mm (IQR = 0.52–0.55) and the Zeiss IOLMaster 700 reported a median of 0.54 mm (IQR = 0.52–0.55). The ICC for CCT was notably high at 0.961, with a 95% confidence interval from 0.92 to 0.98, indicating excellent agreement. Neither the Mann–Whitney U-test (p = 0.267) nor Levene’s test (p = 0.588) revealed significant differences between the measurements.
For ACD measurements, the Heidelberg Anterion device reported a median of 3.25 mm (IQR = 3.00–3.50), while the Zeiss IOLMaster 700 reported a median of 3.21 mm (IQR = 2.97–3.43). The ICC for ACD was 0.991, with a 95% confidence interval from 0.98 to 1.00, indicating excellent agreement between the devices. Neither the Mann–Whitney U-test (p = 0.355) nor Levene’s test (p = 0.939) indicated significant differences between the measurements.
ACV measurements showed a median of 155.38 mm³ (IQR = 131.15–180.06) for the Heidelberg Anterion and 144.11 mm³ (IQR = 125.62–159.81) for the Zeiss IOLMaster 700, with the latter calculated using the formula. The ICC for ACV was 0.908, with a 95% confidence interval from 0.82 to 0.96, suggesting excellent agreement between the devices. The Mann–Whitney U-test revealed a statistically significant difference between the measurements (p = 0.0519), indicating divergent assessments between the two devices. However, Levene’s test did not detect significant variance (p = 0.216), indicating consistency in the spread of measurements across the two groups.
In our analysis, we examined the cohorts and identified distinctions between the younger cohort and the cataract cohort. Statistically significant differences in measurements between groups were found for the ACV Formula, WTW Anterion, ACD Anterion, and ACD IOLMaster. These results indicate a clear trend of decreasing ACD with advancing age, corroborating findings reported in existing literature.38
The differences in ACV should also be observed in the ACV Anterion and ACV Formula groups. These differences can be attributed to the WTW measurement’s ability to differentiate between various diagnostic machines.39 The observed variations are shown in Table 2.
 |
Table 2 The Measurements Were Compared Between the Heidelberg Anterion and the Zeiss IOLMaster 700, as Well as Between the Cataract and Control Groups |
The main investigation involved examining ACV, WTW, ACD, and AL in patients undergoing cataract surgery at Pauls Stradins Clinical University Hospital. Among the chosen participants, 72 were men, while 126 were women. Furthermore, the SPONCS40 system was utilized to classify the hardness of cataracts. Demographics and ocular pathologies are shown in Table 3.
 |
Table 3 Summary of Demographics and Ophthalmic Co-Morbidities Among Patients Included in the Study |
Results
A comprehensive analysis displaying patient concurrent pathologies and their statistical relevance to ACV, WTW, ACD, and AL is shown in Table 4.
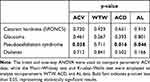 |
Table 4 The ACV, WTW, ACD, and AL, Along with Their Statistical Significance in Relation to Ocular Comorbidities |
The volume of intraocular fluid differed significantly between groups with and without pseudoexfoliation (PEX). Eyes with PEX had a significantly lower ACV (133 ± 28.3 mm³) compared to eyes without PEX (142 ± 30.7 mm³), with a statistically significant difference of −8.94 mm³, 95% CI [−17.4, −0.518], t (196) = −2.09, p = 0.038, d = −0.301. There was also a significant difference in ACD between eyes with PEX (median = 3.00 mm, IQR = 2.71–3.32 mm) and without PEX (median = 3.17 mm, IQR = 2.90–3.45 mm), U = 3824, p = 0.016, r = 0.201. There was also a significant difference in AL between eyes with PEX (median = 23.4 mm, IQR = 22.8–24.0 mm) and without PEX (median = 23.6 mm, IQR = 22.9–24.6 mm), U = 3784, p = 0.046, r = 0.169.
Discussion
Although the measurement of ACV has not yet become standard clinical practice, it holds significant potential for addressing various ocular issues. It can aid in glaucoma diagnosis and management, cataract surgery planning, refractive surgery, assessment of ocular health, and research and development.
A considerable body of research has explored the ACV across various ocular pathologies. Eyes with an ACV of 100 mm³ or less may be classified as having a high risk for the development of acute angle-closure glaucoma.41 The ACV increased significantly at 1 day, 1 week, and 1 month following cataract surgery.42 While there was no observed change in ACV, a notable reduction in ACD was found following myopic LASIK in young patients.42 Corneas with increased thickness might correlate with reduced aqueous production and diminished uveoscleral outflow.43 Biometric differences between Caucasian and Chinese adults include larger ACVs.44 Reduced anterior chamber area and ACV were found to be independently associated with narrow angles, even following adjustment for established ocular biometric parameters such as ACD and AL.45 Greater ACV was found to be associated with decreased deformation altitude values and increasing age while exhibiting higher stiffness parameters and intraocular pressure values.30
In our study, the most pronounced differences were observed within the groups affected by PEX. The literature reveals a lack of consensus concerning the biometric characteristics of the anterior segment in eyes affected by PEXS. A population-based cross-sectional cohort study has shown that PEXS is correlated with advanced age, reduced AL, and a diminished ACD.46 A study demonstrated that the anterior chamber of the eye is significantly shallower in patients with PEX syndrome compared to the control group.47 Research has indicated that eyes with PEX syndrome and cataracts exhibit significantly reduced ACD and increased lens thickness compared to eyes with cataracts alone.47 The reduced ACD observed in patients with PEX syndrome is believed to result from the forward displacement of the lens, which is attributed to lens thickening and the weakening of the lens zonules.48 The fragility of the zonular apparatus significantly contributes to the elevated incidence of phacodonesis, lens dislocation, and vitreous complications encountered during extracapsular cataract surgery in eyes with PEXS.49
However, according to the findings from the Reykjavik Eye Study, PEX did not exhibit a correlation with CCT, ACD, lens thickness, nuclear lens opacifications, or optic disc morphology when analyzed within a multivariate model.50 Duran et al observed no significant differences in ACD when comparing eyes with PEX to their fellow eyes or to control eyes.51
There are only a few studies that have investigated the association between PEX and the axial length of the eye. Topouzis et al found that individuals with incident PEX had a statistically significantly shorter axial length compared to those who had not developed PEX.52 Topouzis’s findings propose that shorter axial length might contribute to the onset of PEX, which may explain the association observed with a shallow anterior chamber in the Beijing Eye Study 2011 by You Q. et al.46
The evidence concerning differences in ACV between eyes with PEX and those without is inconclusive. Mohamed-Noriega et al reported that the ACV, measured using the Pentacam, exhibited negligible differences between the control group (mean ± SD: 109.6 ± 25.6 mm³) and the group affected by PEXS (mean ± SD: 113.363 ± 24.79 mm³).53 Doganay et al employed the Pentacam-Scheimpflug imaging system to assess anterior segment parameters in patients with PEXS, pseudoexfoliative glaucoma (PEXG), and a control group. Their findings revealed no significant differences in mean values of ACV, anterior chamber angle width, CCT, pupil diameter, or corneal volume at 3.0 mm, 5.0 mm, and 7.0 mm among the three groups.54 According to Gharagozloo et al, ACV was markedly decreased in both affected and unaffected eyes of individuals with unilateral PEXS compared to control eyes.55 The Duran et al study revealed no significant differences in ACD, ACV, iridocorneal angle, or keratometry values when comparing eyes with PEX to either fellow eyes or control eyes.51 Omura et al observed that eyes positive for PEXS exhibited a diminished ACV in comparison to PEX-negative eyes.56 Studies have demonstrated that patients with PEXG experience a more pronounced reduction in intraocular pressure following cataract surgery compared to control groups.57
During this study, we hypothesized that glaucoma would be the ocular comorbidity most strongly associated with ACV. However, this hypothesis was not supported by our findings. Lens thickness is an important parameter that can influence ACV and may have implications for conditions such as glaucoma. Increased lens thickness was significantly associated with advancing age, male sex, greater body height, elevated body mass index, hyperopic refractive error, thicker central corneal measurements, reduced anterior chamber depth, and the presence of nuclear cataracts.58 However, in our study, lens thickness was not measured due to the exclusion of patients with severe lens opacities, which cannot be accurately assessed using optical interferometry. While this limitation restricts our ability to explore the relationship between lens thickness and ACV, future studies that include lens thickness measurements would provide valuable insights into how lens thickness may correlate with ACV and its role in ocular health. However, in both POAG patients and individuals without the condition, no meaningful relationship was observed between IOP and ACD, nor between IOP and lens thickness.59 Eyes with angle-closure glaucoma or occludable angles exhibit noticeably shorter AL, shallower ACD, and thicker lenses when compared to those in the normal group.60 Glaucoma is defined as a group of disorders characterized by the degeneration of ganglion cells resulting from axonal damage at the lamina cribrosa of the optic nerve. In essence, glaucoma is a diagnosis of exclusion when the etiology of the optic nerve damage remains unidentified.61 Lowering IOP does not fully address the underlying mechanisms of neurodegeneration. Therefore, there is a significant need for pharmacologic approaches that can protect against glaucomatous neurodegeneration independently of IOP.62
There have been studies linking glaucoma to ACV. The IOP/ACV ratio may serve as a novel diagnostic parameter for predicting the likelihood of success in prostaglandin analogue treatment.63 ACV is a robust and precise predictor of the outcomes of primary angle closure disease.64
Emerging research on the intraocular fluid metabolome shows promise in elucidating integrated biological mechanisms within the anterior segment of the eye and advancing treatment strategies for ocular diseases. Variations in intraocular fluid composition among cataract patients65,66 and individuals with PEX67 have been documented in existing literature. Future investigations could harness data from liquid chromatography-mass spectrometry machines and consider ACV as a potential alternative for concentration calculations in these studies. The product of a substance’s concentration within a fluid and the volume of that fluid determines the total mass or amount of the substance, a critical factor in assessing its overall presence within the fluid.
An accessible and cost-effective method for measuring ACV that does not rely on advanced equipment such as the Pentacam or AS-OCT would be highly beneficial, particularly in developing countries where access to such technology may be limited. With the availability of ocular biometry, it could significantly enhance clinical research on ACV by enabling broader and more comprehensive studies.
Conclusion
Our study evaluated the discrepancies between ACV measurements obtained from the Heidelberg Anterion and Zeiss IOLMaster 700. ACV measurements showed a median of 155.38 mm³ (IQR = 131.15–180.06) for the Heidelberg Anterion and 144.11 mm³ (IQR = 125.62–159.81) for the Zeiss IOLMaster 700, with the latter calculated using the formula. The ICC for ACV was 0.908 (95% CI: 0.82–0.96), indicating excellent agreement between the devices. While the Mann–Whitney U-test revealed a statistically significant difference (p = 0.0519), Levene’s test showed no significant variance (p = 0.216), suggesting consistency in the spread of measurements across both devices. We also refined a formula for calculating intraocular fluid volume, which demonstrated excellent agreement with AS-OCT methods. Additionally, our investigation highlighted the significance of ACV and other ocular biometry parameters in relation to ocular comorbidities, revealing that both ACD and ACV exhibit age-related changes. Notably, eyes affected by PEXS showed reduced ACD, ACV, and AL measurements. This is the first study to validate our redefined formula, which could enable broader clinical research, particularly in settings with limited access to advanced imaging technologies. While ACV remains underexplored, its potential applications in ophthalmology merit further investigation.
Abbreviations
OCT, optical coherence tomography; ACV, anterior chamber volume; WTW, white-to-white corneal diameter; CCT, central corneal thickness; ACD, anterior chamber depth; RAC, radius of the anterior chamber; CCD, central chamber depth; AS-OCT, anterior segment optical coherence tomography; ICC, intraclass correlation coefficient; IQR, interquartile range; PEX, pseudoexfoliation; PEXS, pseudoexfoliation syndrome; PEXG, pseudoexfoliative glaucoma; IOP, intraocular pressure.
Data Sharing Statement
All data generated or analyzed during this study are presented within this article. Additional information is available upon request by contacting the corresponding author.
Ethics Approval and Informed Consent
The research adhered to the ethical principles delineated in the Declaration of Helsinki. Stringent ethical scrutiny was applied to the study’s considerations, resulting in approval from the Medical Ethics Committee of Rigas Stradins University, denoted by decision number 2-PEK-4/307/2023. Furthermore, the requisite approval was obtained from the Pauls Stradins Clinical University Hospital. Patients provided written informed consent to participate in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
All authors hereby declare that they have no conflicts of interest or proprietary interests associated with this work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dvoriashyna M, Repetto R, Romano MR, et al. Aqueous humour flow in the posterior chamber of the eye and its modifications due to pupillary block and iridotomy. Math Med Biol. 2018;35(4):447–467. doi:10.1093/imammb/dqx012
2. Kiel JW. Integrated Systems Physiology: From Molecule to Function to Disease. The Ocular Circulation. San Rafael (CA): Morgan & Claypool Life Sciences Copyright © 2010 by Morgan & Claypool Life Sciences; 2010.
3. Tamm E. The trabecular meshwork outflow pathways: structural and functional aspects. Exp. Eye Res. 2009;88(4):648–655. doi:10.1016/j.exer.2009.02.007
4. Pizzirani S, Gong H. Functional anatomy of the outflow facilities. Vet Clin North Am Small Anim Pract. 2015;45(6):1101–1126,v.20150831. doi:10.1016/j.cvsm.2015.06.005
5. Gabelt BA, Kaufman P. Changes in aqueous humor dynamics with age and glaucoma. Prog Retinal Eye Res. 2005;24(5):612–637. doi:10.1016/j.preteyeres.2004.10.003
6. Toris CB, Koepsell SA, Yablonski ME, et al. Aqueous humor dynamics in ocular hypertensive patients. J Glaucoma. 2002;11(3):253–258. doi:10.1097/00061198-200206000-00015
7. Pederson JE. Ocular hypotony. Trans Ophthalmol Soc U K (1962). 1986;105(Pt 2):220–226.
8. Alaghband P, Baneke AJ, Galvis E, et al. Aqueous humor dynamics in uveitic eyes. Am J Ophthalmol. 2019;208:347–355.20190830. doi:10.1016/j.ajo.2019.08.018
9. Krzyzanowska I, Töteberg-Harms M. Angle-closure glaucoma. Ophthalmologie. 2022;119(11):1167–1179.20221027. doi:10.1007/s00347-022-01745-w
10. Botling Taube A, Konzer A, Alm A, et al. Proteomic analysis of the aqueous humour in eyes with pseudoexfoliation syndrome. Br J Ophthalmol. 2019;103(8):1190–1194.20190306. doi:10.1136/bjophthalmol-2017-310416
11. Wang X, Ma X, Song J, et al. Analysis aqueous humor lipid profile of neovascular glaucoma secondary to diabetic retinopathy and lipidomic alteration response to anti-VEGF treatment. Exp Eye Res. 2024;242:
12. Toris C, Gagrani M, Ghate D. Current methods and new approaches to assess aqueous humor dynamics. Expert Rev Ophthalmol. 2021;16(3):139–160. doi:10.1080/17469899.2021.1902308
13. Goel M, Picciani RG, Lee RK, et al. Aqueous humor dynamics: a review. Open Ophthalmol J. 2010;4(1):52–59.20100903. doi:10.2174/1874364101004010052
14. Sunderland DK, Sapra A. Physiology, Aqueous Humor Circulation. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2024; 2024.
15. Liu H, Fan S, Gulati V, et al. Aqueous humor dynamics during the day and night in healthy mature volunteers. Archives of Ophthalmology. 2011;129(3):269–275. doi:10.1001/archophthalmol.2011.4
16. Kondo T, Miura M, Imamichi M. Measurement method of the anterior chamber volume by image analysis. Br J Ophthalmol. 1986;70(9):668–672. doi:10.1136/bjo.70.9.668
17. Nagataki S, Lee DA, Iri M. A simple geometrical method of measuring anterior chamber dimensions. Invest Ophthalmol Vis Sci. 1984;25(10):1192–1197.
18. Jones RF, Maurice DM. A SIMPLE PHOTOGRAPHIC METHOD OF MEASURING THE VOLUME OF THE ANTERIOR CHAMBER. Exp Eye Res. 1963;2(3):233–236. doi:10.1016/s0014-4835(63)80041-x
19. Brown N. Quantitative Slit-Image Photography of the Anterior Chamber. Vol. 93. Trans Ophthalmol Soc U K (1962); 1973:277–286.
20. Johnson SB, Passmore JA, Brubaker RF. The fluorescein distribution volume of the anterior chamber. Invest Ophthalmol Vis Sci. 1977;16(7):633–636.
21. Jones RF, Maurice DM. New methods of measuring the rate of aqueous flow in man with fluorescein. Exp Eye Res. 1966;5(3):208–220. doi:10.1016/s0014-4835(66)80009-x
22. Luo Y, Cui HP, Liu Y, et al. Metabolomics and biomarkers in ocular matrix: beyond ocular diseases. Int J Ophthalmol. 2020;13(6):991–1003.20200618. doi:10.18240/ijo.2020.06.21
23. Asam JS, Polzer M, Tafreshi A, et al. Anterior Segment OCT. In: Bille JF, editor. High Resolution Imaging in Microscopy and Ophthalmology: New Frontiers in Biomedical Optics. Cham (CH): Springer Copyright 2019, The Author(s); 2019:285–299.
24. Bullimore MA, Slade S, Yoo P, et al. An evaluation of the IOLMaster 700. Eye Contact Lens. 2019;45(2):117–123. doi:10.1097/icl.0000000000000552
25. Hoffer KJ. Definition of ACD. Ophthalmology. 2011;118(7):1484. doi:10.1016/j.ophtha.2011.03.009
26. Heim M. Photographische Bestimmung der Tiefe und des Volumens der menschlichen Vorderkammer (Part 1 of 2). Ophthalmologica. 2010;102(4):193–206. doi:10.1159/000299988
27. Tomlinson A, Leighton DA. Ocular dimensions and the heredity of open-angle glaucoma. Br J Ophthalmol. 1974;58(1):68–74. doi:10.1136/bjo.58.1.68
28. Johnson SB, Coakes RL, Brubaker RF. A simple photogrammetric method of measuring anterior chamber volume. Am J Ophthalmol. 1978;85(4):469–474. doi:10.1016/s0002-9394(14)75243-2
29. He W, Zhu X, Wolff D, et al. Evaluation of anterior chamber volume in cataract patients with swept-source optical coherence tomography. J Ophthalmol. 2016;2016:
30. Cui X, Yang Y, Li Y, et al. Correlation between anterior chamber volume and corneal biomechanical properties in human eyes. Front Bioeng Biotechnol. 2019;7:
31. Anandan V, Srinivasan R, Asokan R, et al. Evaluation of anterior chamber volume using Pentacam and anterior segment optical coherence tomography among normal subjects. Asian J Ophthalmol. 2018;16(2):86–94. doi:10.35119/asjoo.v16i2.367
32. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163.20160331. doi:10.1016/j.jcm.2016.02.012
33. Alavi M, Biros E, Cleary M. A primer of inter-rater reliability in clinical measurement studies: pros and pitfalls. J Clin Nurs. 2022;31(23–24):e39–e42.20220906. doi:10.1111/jocn.16514
34. Mishra P, Pandey CM, Singh U, et al. Descriptive statistics and normality tests for statistical data. Ann Card Anaesth. 2019;22(1):67–72. doi:10.4103/aca.ACA_157_18
35. Kerby D. The simple difference formula: an approach to teaching nonparametric correlation. Comprehensive Psychol. 2014;3:
36. Andrade C. The P value and statistical significance: misunderstandings, explanations, challenges, and alternatives. Indian J Psychol Med. 2019;41(3):210–215. doi:10.4103/ijpsym.Ijpsym_193_19
37. Joseph LG, Yulia RG, Weiwen M. The impact of Levene’s test of equality of variances on statistical theory and practice. Stat Sci. 2009;24:343–360. doi:10.1214/09-STS301
38. Kamo J, Saso M, Tsuruta M, et al. Aging effect on peripheral anterior chamber depth in male and female subjects investigated by scanning peripheral anterior chamber depth analyzer. Nippon Ganka Gakkai Zasshi. 2007;111(7):518–525.
39. Bao T, Wang L, Liu C, et al. Analysis of biometric parameters of cataract eyes measured with optical biometer Lenstar LS900, IOL Master 700, and OPD-SCAN III. Photodiagnosis Photodyn Ther. 2023;43:
40. Mandelblum J, Fischer N, Achiron A, et al. A Simple Pre-Operative Nuclear Classification Score (SPONCS) for grading cataract hardness in clinical studies. J Clin Med. 2020;9(11):20201029. doi:10.3390/jcm9113503
41. Pakravan M, Sharifipour F, Yazdani S, et al. Scheimpflug imaging criteria for identifying eyes at high risk of acute angle closure. J Ophthalmic Vis Res. 2012;7(2):111–117.
42. Chen M, Hu H, He W, et al. Observation of anterior chamber volume after cataract surgery with swept-source optical coherence tomography. Int Ophthalmol. 2019;39(8):1837–1844.20180904. doi:10.1007/s10792-018-1012-1
43. Gulati V, Ghate DA, Camras CB, et al. Correlations between parameters of aqueous humor dynamics and the influence of central corneal thickness. Invest Ophthalmol Visual Sci. 2011;52(2):920–926. doi:10.1167/iovs.10-5494
44. Fan S, Guo T, Chen B, et al. Differences in ocular biometrics and aqueous humour dynamics between Chinese and Caucasian adults. Br J Ophthalmol. 2019;103(12):1845–1849.20190320. doi:10.1136/bjophthalmol-2018-313132
45. Wu RY, Nongpiur ME, He MG, et al. Association of narrow angles with anterior chamber area and volume measured with anterior-segment optical coherence tomography. Arch Ophthalmol. 2011;129(5):569–574. doi:10.1001/archophthalmol.2011.68
46. You QS, Xu L, Wang YX, et al. Pseudoexfoliation: normative data and associations: the Beijing eye study 2011. Ophthalmology. 2013;120(8):1551–1558.20130425. doi:10.1016/j.ophtha.2013.01.020
47. Dembski M, Nowińska A, Ulfik-Dembska K, et al. Swept source optical coherence tomography analysis of a selected eye’s anterior segment parameters in patients with pseudoexfoliation syndrome. J Clin Med. 2022:1120220105. doi:10.3390/jcm11010268.
48. Janjetović Ž, Bušić M, Bosnar D, et al. Specific characteristics of ocular biometric factors in glaucomatous patients with pseudoexfoliative syndrome as measured by optical low-coherence reflectometry. Acta Clin Croat. 2019;58(1):87–94. doi:10.20471/acc.2019.58.01.11
49. Schlötzer-Schrehardt U, Naumann GO. A histopathologic study of zonular instability in pseudoexfoliation syndrome. Am J Ophthalmol. 1994;118(6):730–743. doi:10.1016/s0002-9394(14)72552-8
50. Arnarsson A, Damji KF, Sverrisson T, et al. Pseudoexfoliation in the Reykjavik Eye Study: prevalence and related ophthalmological variables. Acta Ophthalmol Scand. 2007;85(8):822–827. doi:10.1111/j.1600-0420.2007.01051.x
51. Duran M, Şahin T, Cevher S. Evaluation of anterior segment parameters of clinically unilateral pseudoexfoliation syndrome using scheimpflug imaging technique. Hitit Medical Journal. 2023;5(3):126–130. doi:10.52827/hititmedj.1276468
52. Topouzis F, Founti P, Yu F, et al. Twelve-year incidence and baseline risk factors for pseudoexfoliation: the thessaloniki eye study (an American ophthalmological society thesis). Am J Ophthalmol. 2019;206:192–214.20190513. doi:10.1016/j.ajo.2019.05.005
53. Mohamed-Noriega J, Mohamed-Noriega K, Ruiz-Gonzalez JA, et al. Evaluation of anterior chamber imaging parameters in pseudoexfoliation patients. Invest Ophthalmol Visual Sci. 2016;57:5138.
54. Doganay S, Tasar A, Cankaya C, et al. Evaluation of Pentacam-Scheimpflug imaging of anterior segment parameters in patients with pseudoexfoliation syndrome and pseudoexfoliative glaucoma. Clin Exp Optom. 2012;95(2):218–222.20120209. doi:10.1111/j.1444-0938.2011.00691.x
55. Gharagozloo NZ, Baker RH, Brubaker RF. Aqueous dynamics in exfoliation syndrome. Am J Ophthalmol. 1992;114(4):473–478. doi:10.1016/s0002-9394(14)71860-4
56. Omura T, Tanito M, Doi R, et al. Correlations among various ocular parameters in clinically unilateral pseudoexfoliation syndrome. Acta Ophthalmol. 2014;92(5):e412–413.20140125. doi:10.1111/aos.12348
57. Ramezani F, Nazarian M, Rezaei L. Intraocular pressure changes after phacoemulsification in pseudoexfoliation versus healthy eyes. BMC Ophthalmol. 2021;21(1):
58. Jonas JB, Nangia V, Gupta R, et al. Lens thickness and associated factors. Clin Exp Ophthalmol. 2012;40(6):583–590.20120321. doi:10.1111/j.1442-9071.2012.02760.x
59. Adewara BA, Adegbehingbe BO, Onakpoya OH, et al. Relationship between intraocular pressure, anterior chamber depth and lens thickness in primary open-angle glaucoma patients. Int Ophthalmol. 2018;38(2):541–547.20170313. doi:10.1007/s10792-017-0488-4
60. George R, Paul PG, Baskaran M, et al. Ocular biometry in occludable angles and angle closure glaucoma: a population based survey. Br J Ophthalmol. 2003;87(4):399–402. doi:10.1136/bjo.87.4.399
61. Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311(18):1901–1911. doi:10.1001/jama.2014.3192
62. Cursiefen C, Cordeiro F, Cunha-Vaz J, et al. Unmet needs in ophthalmology: a European vision institute-consensus roadmap 2019–2025. Ophthal Res. 2019;62(3):123–133. doi:10.1159/000501374
63. Scott JA, Roberts CJ, Mahmoud AM, et al. Evaluating the relationship of intraocular pressure and anterior chamber volume with use of prostaglandin analogues. J Glaucoma. 2021;30(5):421–427. doi:10.1097/ijg.0000000000001736
64. Zhou R, Li F, Gao K, et al. Smaller anterior chamber volume is associated with higher risk of intraocular pressure elevation after laser peripheral iridotomy: a 1-year follow-up study. Asia-Pac J Ophthalmol. 2021;10:188–191.
65. Yanshole VV, Yanshole LV, Snytnikova OA, et al. Quantitative metabolomic analysis of changes in the lens and aqueous humor under development of age-related nuclear cataract. Metabolomics. 2019;15(3):
66. Zemitis A, Vanags J, Fan J, et al. Metabolomic disparities in intraocular fluid across varied stages of cataract progression: implications for the analysis of cataract development. J Ocul Pharmacol Ther. 2024;40(8):477–485. doi:10.1089/jop.2024.0067
67. Dmuchowska DA, Pietrowska K, Krasnicki P, et al. Metabolomics reveals differences in aqueous humor composition in patients with and without pseudoexfoliation syndrome. Front Mol Biosci. 2021;8:
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


