Back to Journals » Journal of Inflammation Research » Volume 17
Relationship Between the Systemic Immune-Inflammation Index and Deep Venous Thrombosis After Spinal Cord Injury: A Cross-Sectional Study
Authors Tian F , Lu Y, Liu X , Zhao C, Xi X, Hu X, Xue Y, Sun X, Yuan H
Received 6 September 2024
Accepted for publication 29 October 2024
Published 6 November 2024 Volume 2024:17 Pages 8325—8334
DOI https://doi.org/10.2147/JIR.S491055
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tara Strutt
Fei Tian,1,* Yuheng Lu,1,* Xinyu Liu,1,* Chenguang Zhao,1 Xiao Xi,1 Xu Hu,1 Yike Xue,2 Xiaolong Sun,1 Hua Yuan1
1Department of Rehabilitation Medicine, Xijing Hospital, The Fourth Military Medical University, Xi’an, People’s Republic of China; 2Department of Diagnostic Radiology, Xijing Hospital, The Fourth Military Medical University, Xi’an, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaolong Sun; Hua Yuan, Department of Rehabilitation Medicine, Xijing Hospital, The Fourth Military Medical University, Xi’an, People’s Republic of China, Email [email protected]
Purpose: To explore the relationship between the systemic immune-inflammation index (SII) and deep venous thrombosis (DVT) in patients with spinal cord injury (SCI).
Methods: This cross-sectional study included data from 382 participants with SCI. The SII was calculated for all participants. Logistic regression, smooth curve fitting, interaction effects were used to substantiate the research objectives.
Results: The overall prevalence of DVT was 23.1% (22.4% among males, 25.6% among females). A positive association between SII and the risk for DVT was observed (odds ratio 1.39 [95% CI 1.03– 1.87]; P=0.032), independent of confounders. Similar patterns of association were observed in the subgroup analysis (P values for interaction, all > 0.05). Further sensitivity analyses provided confidence that the results were reliable and unlikely to be substantially altered by unmeasured confounding factors.
Conclusion: Results of the present suggest that higher SII may be associated with DVT in patients with SCI, highlighting a potential link between SII and DVT. These findings underscore the potential of SII as a valuable predictive biomarker for DVT, thus offering a promising avenue for early detection and intervention strategies in patients with SCI.
Plain Language Summary: The aim of this study was to investigate the relationship between the systemic immune-inflammation index (SII) and deep vein thrombosis (DVT) in patients with spinal cord injury (SCI). We analyzed data from 382 SCI patients and found that 23.1% of them had DVT. The risk of DVT was significantly increased by 39% with each 1-point increase in SII (OR = 1.39, 95% CI: 1.03– 1.87, p = 0.031). Our results showed that higher SII values were associated with an increased risk of DVT, independent of other factors. This suggests that SII may be used as a potential biomarker to predict DVT in SCI patients, highlighting the importance of early detection and intervention. This finding could greatly contribute to the early detection and management of DVT in SCI patients using SII.
Keywords: systemic immune-inflammation index, deep venous thrombosis, spinal cord injury
Introduction
The most common complication of spinal cord injury (SCI) is deep vein thrombosis (DVT). It has been reported that the incidence of DVT in patients with SCI is 5% to 26%.1 DVT is a prevalent global disease characterized by primary symptoms including leg swelling, pain, and rubor.2 It is primarily caused by stasis, vascular wall damage or dysfunction, and hypercoagulability.3 DVT continues to be a global burden, affecting approximately 88 to 112 individuals/1,000,000 person-years.4,5 The onset of DVT can significantly reduce life expectancy, underscoring the importance of a comprehensive understanding of this condition and its contributing factors.6,7 Such knowledge is crucial for effective prevention, management and, ultimately, enhancing the prognosis and quality of life of those affected by DVT.
Recently, the systemic immune-inflammation index (SII), a critical blood parameter, has been developed as a prognostic predictor of various cancers and inflammatory diseases.8–11 Involving 3 inflammatory biomarkers, including platelets, neutrophils and lymphocytes, the SII is calculated as platelets × neutrophils/lymphocytes, and may provide a comprehensive reflection of local immune status and systemic inflammation in the entire body simultaneously.12,13 DVT is related to inflammation, and the SII is an indicator of the severity of whole-body inflammation.12,14 A recent study demonstrated an association between SII and pulmonary embolism.15,16 Therefore, the SII may be associated with DVT.
Currently, however, there is insufficient evidence supporting the association between SII and DVT. To address this knowledge gap, our primary objective was to investigate the relationship between SII and DVT and explore the implications of this association. We conducted a retrospective cross-sectional study involving 382 participants from the Department of Rehabilitation Medicine at the First Affiliated Hospital of the Air Force Medical University (Shaanxi, China).
Material and Methods
Study Population
This single-center, retrospective, observational study was performed at a tertiary teaching hospital in China. The study protocol was reviewed and approved by the Institutional Ethics Committee of Xijing Hospital of the Fourth Military Medical University (KY20222096-C-1) and conducted in accordance with the tenets of the Declaration of Helsinki. Given the retrospective design of the study and the use of anonymized data, requirements for informed consent were waived. In this study, all patients hospitalized between January 1, 2018 and January 1, 2024 were screened by searching the HIS database. The inclusion criteria were as follows:17,18 diagnosed with SCI; underwent vascular color Doppler ultrasound examination on admission; and collected blood sampling for SII on admission. At the initial screening, 407 patients with SCI were considered. Subsequently, patients were excluded if they fulfilled any of the following criteria: history of previous DVT; superficial venous thrombosis; active infection or chronic inflammation; and use of immunosuppressive therapy. Ultimately, data from 382 consecutive hospitalized patients were included in this study (Figure 1).
 |
Figure 1 Flowchart of patient inclusion and exclusion. Abbreviations: DVT, deep venous thrombosis; SII, systemic immune-inflammation index. |
Covariates
The following variables were included based on the published literature and clinical experience:2,17,19,20 general information (sex, age, blood type smoking, cause, spinal injury plane, American Spinal Injury Association [ASIA] scale score, operation, and onset to admission); and comorbidities (fracture, hypertension, and diabetes); and biological indicators (SII, calculated as: platelet count × neutrophil count / lymphocytes). The units for SII are expressed as 109/L. The time of onset corresponds to the time of SCI, and admission is defined as the first admission to our departmental, and time is measured in days.
Outcome
The primary outcome was the incidence of DVT events at admission, which was confirmed by ultrasound reports.
Statistical Analysis
Histogram distribution, or Q-Q plot, or Kolmogorov–Smirnov test were used for determining whether variables were normally distributed. All normally distributed continuous variables are expressed as mean ± standard deviation (SD), whereas skewed continuous variables are expressed as median (interquartile range [IQR]). Categorical variables are expressed as frequency (percentage [%]). Comparisons of categorical variables were performed using the chi-squared or Fisher’s exact tests, one-way analysis of variance (normal distribution), or Kruskal–Wallis H-test (skewed distribution) to test for differences among different SII groups.
Univariate and multivariate binary logistic regression models were used to test the association between SII and DVT. SII was entered as a continuous variable. These confounders were selected on the basis of clinical interest, the previous scientific literature, all significant covariates in the univariate analysis, or their associations with the outcomes of interest or a change in effect estimate of > 10%. Potential multi-collinearity was tested using the variance inflation factor (VIF), with VIF ≥ 5 indicating the presence of multi-collinearity. Three models were constructed: model 1, adjusted for age and sex; model 2, additionally adjusted for diabetes, hypertension, smoking, and operation; and model 3, additionally adjusted for cause.
Restricted cubic spline models were constructed to develop smooth curves to examine the possible nonlinear dose-response associations between SII and DVT. In this model, SII was used as a continuous variable with 4 knots (5th, 35th, 65th and 95th percentiles) suggested by Harrell. Nonlinearity was tested using a likelihood ratio test comparing the model with only a linear term against the model with linear and cubic spline terms. Interaction and stratified analyses were performed according to subgroup variables. Interaction(s) across subgroups was tested using the likelihood ratio test. Missing data accounted for < 5% of the dataset and were handled by list wise deletion on an analysis basis. To replace missing covariate data with statistical estimates of the missing values, mean, median or mode was used as imputation value for continuous variables, and make NA, 9 or mode as a level for categorical variables. This enabled the researchers to use the collected data in an incomplete dataset. All analyses with complete cohort data for comparison were repeated. The initial model included all available variables (eg, age, sex, diabetes, hypertension, smoking, operation, cause, blood type). The caliper width on the propensity score scale was 0.25 and 1:1 sampling without replacement. All patient characteristics included in generating and distributing the propensity scores were compared before and after propensity score-matching using the standardized mean difference. A threshold < 0.1 was considered to be acceptable Finally, NNN matched pairs were generated and applied to further analyses. All analyses were performed using R version 4.2.2 (http://www.R-project.org R Foundation for Statistical Computing, Vienna, Austria) and FreeStatistics analysis platform version 1.9 (Beijing, China http://www.clinicalscientists.cn/freestatistics). FreeStatistics is a software package that provides intuitive interfaces for most common analyses and data visualization. It uses R as the underlying statistical engine, and the graphical user interface is written in “Python”. Most analyses can be completed with merely a few clicks. It is designed for reproducible analysis and interactive computing. Differences with a two-sided P < 0.05 were considered to be statistically significant.
Results
Study Population Characteristics
A cohort of 382 patients with a mean (± SD) age of 42.6 ± 12.9 years was enrolled. The demographic was exclusively Han Chinese and the majority of subjects (79.6%) was male. Of these, the overall prevalence of DVT was 23.1%. General characteristics of the participants according to SII are summarized in Table 1. The 4 groups differed in smoking, hypertension, and onset to admission (all P < 0.05). Otherwise, the distribution of patient characteristics (age, blood type, operation, cause, fracture, spinal injury plane, ASIA Scale score, diabetes, and DVT) between the SII groups demonstrated no significant differences (all P > 0.05).
 |
Table 1 Baseline Characteristics of Participants |
Association Between SII and the Risk for DVT
In the univariable analysis, we found that SII was a risk factor for DVT (Supplementary Table 1). Findings from the multivariable logistic regression analysis investigating the correlation between SII and DVT are summarized in Table 2. A higher SII was found to be linked to a heightened risk for DVT (per 1 unit increase, OR 1.39 [95% CI 1.03–1.87]; P=0.032), even after controlling for potential confounding variables (model 3) (Table 2).
 |
Table 2 Multivariate Regression Analysis of Association Between SII and DVT |
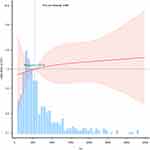
The adjusted smoothed plots in Figure 2 indicate a clear linear relationship between SII and DVT, with a P-value for non-linearity of 0.959. To ensure robustness, the highest and lowest 0.5% of SII values were excluded for each measurement. The trend observed in the plots demonstrate that as SII increases, the risk for DVT increases.
Sensitivity and Subgroup Analyses
Stratified analyses according to sex, operation, hypertension, and diabetes were also performed (Supplementary Table 2). The risk estimates were generally similar for incident DVT across subgroups (all P for interaction >0.05) (Figure 3). For incident DVT, statistically significant results were found for males (OR 1.49 [95% CI 1.05–2.11]), no hypertension (OR 1.39 [95% CI 1.00–1.91]), and no diabetes (OR 1.37 [95% CI 1.02–1.85]). Effect estimates were overlapping in the operation group but were less precise due to the limited number of operative cases. Sensitivity analysis revealed no significant differences in characteristics between the excluded and included participants. Multivariable regression analysis including only patients with complete data yielded similar results.
Discussion
In this study, we revealed a significant positive correlation between SII and the risk for DVT, with an OR of 1.39 (95% CI 1.03–1.87). This association held true across subgroup analyses, with no significant interaction effects observed. Sensitivity analyses further reinforced the robustness of our findings, suggesting that the results were reliable and not likely to be significantly influenced by unmeasured confounding factors.
Current studies have pointed out that systemic inflammation and SII may represent a risk factor for DVT on many occasions. For example, in a Mendelian randomization study, Lv et al reported a strong association between immune-mediated inflammatory diseases and DVT,21 indicating a potential genetic correlation between these two diseases. Chen et al found that the SII was a robust predictor of DVT in elderly patients after hip fracture.22 Similarly, Melinte et al reported higher pre-operative SII strongly predicted acute DVT following total knee arthroplasty.23 To make matters worse, once diagnosed with DVT, high baseline SII values means increased risk for mortality.24 As for patients with SCI, they often remain bedridden for a prolonged period, predisposing them to the development of DVT, thus identifying factors that predict the occurrence of thrombosis is crucial. However, no previous studies have explored whether the SII can serve as a strong correlated factor for DVT.
We identified a positive association between SII and DVT in SCI patients from the Department of Rehabilitation Medicine at the First Affiliated Hospital of Air Force Medical University, which is in accordance with former research in other diseases. Moreover, this association turned to be linear after adjusting for potential confounders and remained statistically significant across different patient subgroups, suggesting a robust and generalizable association. While partially different from our findings, Chen et al did confirm elevated SII was significantly associated with an increased risk of DVT in hospitalized patients, yet it was a non-linear relationship with a threshold effect.25 Thus, we speculate that SII could potentially serve as a valuable predictor of DVT, but different SII predictive models may exist under different diseases and conditions, which are worth further exploration.
In terms of potential mechanisms by which SII can reflect the risk for DVT, emerging studies have highlighted the multifaceted role of systemic inflammation in the pathogenesis of thrombotic events. First, SII, which incorporates neutrophil and platelet counts, reflects the body’s systemic inflammatory state. This inflammation is known to activate the coagulation system by increasing the expression of adhesion molecules on endothelial cells, promoting leukocyte recruitment and platelet aggregation.13,26,27 Second, the inflammatory environment can cause endothelial dysfunction, leading to a prothrombotic state by reducing the production of natural anticoagulants such as nitric oxide and prostacyclin.28 Third, components of the SII, particularly neutrophils, are implicated in the release of procoagulant microparticles that directly contribute to thrombus formation.29,30 These insights underscore the importance of considering systemic inflammation in the assessment and management of DVT risk.31,32
This study represents the first attempt to determine the relationship between the SII and the risk of developing DVT in SCI patients using cohort data from our hospital. Strengths of this study lie in the use of a territorially expansive and rigorously validated electronic healthcare database that encompasses all diagnostic records, hospitalizations, and details of medication dispensation. This enabled the meticulous collection of pertinent information necessary to mitigate common biases inherent in traditional observational studies, such as selection and recall biases. A comprehensive set of sensitivity analyses was performed to enhance the interpretation of the results and validate the primary findings.
However, there were several limitations to the present study that warrant acknowledgment. First, it is essential to recognize that an observational study does not replicate the conditions of a randomized controlled trial (RCT). Consequently, the findings obtained may deviate from the expected outcomes of an RCT and should be interpreted within the context of the activities of daily living. The relatively modest sample size in this study restricted its statistical power and the exploration of potential interactions, necessitating caution in the interpretation of the results. Despite efforts to account for all relevant potential confounders in the multivariate model, the presence of unmeasured or unknown residual confounders (eg, time between the surgery and onset of DVT, Surgical hospital, dietary factors, family income) could potentially lead to an overestimation of the observed associations.
Conclusions
Results of this study underscore the impact of aberrant SII levels on DVT in patients with SCI, independent of confounding variables. This association holds significance for clinicians involved in managing DVT. Further validation and confirmation of these findings are imperative for widespread clinical application.
Data Sharing Statement
We have decided to share the de-identified personal data of the participants, which includes all the data used in the article. This data is stored in a CSV file and can be obtained by contacting the corresponding author ([email protected]). The data will be available to others long after the article is officially published.
Ethics Approval
This study protocol was reviewed and approved by the Institutional Ethics Committee of Xijing Hospital of the Fourth Military Medical University (KY20222096-C-1) and conducted in accordance with the tenets of the Declaration of Helsinki.
Acknowledgments
We would like to express our gratitude to all the staff and study investigators for their valuable contributions. Special thanks to Dr. Jie Liu from the Department of Vascular and Endovascular Surgery at the Chinese PLA General Hospital for his consultation on the study design, language polishing, proofreading, statistical support, and insightful comments on the manuscript. We also extend our appreciation to the Free Statistics team in Beijing, China, for their technical assistance and provision of data analysis and visualization tools.
Author Contributions
All authors have contributed substantially to the work reported with respect to conception, design, conduct, acquisition of data, analysis and interpretation; have been involved in drafting, revising, or critically reviewing the article; have given final approval of the manuscript; have agreed to the journal to which the article will be submitted; and agree to accept responsibility for all aspects of the work.
Funding
This study was supported by grants from the National Natural Science Foundation of China (No. 82272591 and 82072534), and the Medical Staff Training & Boost Project of Xijing Hospital (No. XJZT24JC19, XJZT24LY11, and XJZT24QN20).
Disclosure
The author(s) report no conflicts of interest in this work.
References
1. Geerts WH, Bergqvist D, Pineo GF. et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):381S–453S. doi:10.1378/chest.08-0656
2. Khan F, Tritschler T, Kahn S, Rodger M. Venous thromboembolism. Lancet. 2021;398(10294):64–77. doi:10.1016/S0140-6736(20)32658-1
3. Di Nisio M, Van Es N, Büller HR. Deep vein thrombosis and pulmonary embolism. Lancet. 2016;388(10063):3060–3073. doi:10.1016/S0140-6736(16)30514-1
4. Raskob G, Angchaisuksiri P, Blanco A, et al. Thrombosis: a major contributor to global disease burden. Arteriosclerosis, Thrombosis, and Vascular Biology. 2014;34(11):2363–2371. doi:10.1161/ATVBAHA.114.304488
5. Arshad N, Isaksen T, Hansen J, Brækkan S. Time trends in incidence rates of venous thromboembolism in a large cohort recruited from the general population. Eur J Epidemiol. 2017;32(4):299–305. doi:10.1007/s10654-017-0238-y
6. Green D, Hull RD, Mammen EF, Merli GJ, Weingarden SI, Yao JS. Deep vein thrombosis in spinal cord injury. Summary and recommendations. Chest. 1992;102(6 Suppl):633S–635S.
7. Zhang L, He M, Jia W, et al. Analysis of high-risk factors for preoperative DVT in elderly patients with simple Hip fractures and construction of a nomogram prediction model. BMC Musculoskelet Disord. 2022;23(1):441. doi:10.1186/s12891-022-05377-8
8. Nøst T, Alcala K, Urbarova I, et al. Systemic inflammation markers and cancer incidence in the UK Biobank. Eur J Epidemiol. 2021;36(8):841–848. doi:10.1007/s10654-021-00752-6
9. Olmez O, Bilici A, Gursoy P, et al. Impact of systemic inflammatory markers in patients with ALK-positive non-small cell lung cancer treated with crizotinib. Pulmonology. 2023;29(6):478–485. doi:10.1016/j.pulmoe.2022.11.006
10. Liu B, Wang J, Li Y, Li K, Zhang Q. The association between systemic immune-inflammation index and rheumatoid arthritis: evidence from NHANES 1999–2018. Arthritis Res Ther. 2023;25(1):34. doi:10.1186/s13075-023-03018-6
11. Wang R, Wen W, Jiang Z, et al. The clinical value of neutrophil-to-lymphocyte ratio (NLR), systemic immune-inflammation index (SII), platelet-to-lymphocyte ratio (PLR) and systemic inflammation response index (SIRI) for predicting the occurrence and severity of pneumonia in patients with intracerebral hemorrhage. Front Immunol. 2023;14:1115031. doi:10.3389/fimmu.2023.1115031
12. Wu Y, Zhao J, Wang Z, et al. Association of systemic inflammatory markers and tertiary lymphoid structure with pathological complete response in gastric cancer patients receiving preoperative treatment: a retrospective cohort study. Int J Surg. 2023;109(12):4151–4161. doi:10.1097/JS9.0000000000000741
13. Xue J, Ma D, Jiang J, Liu Y. Diagnostic and Prognostic Value of Immune/Inflammation Biomarkers for Venous Thromboembolism: is It Reliable for Clinical Practice? J Inflamm Res. 2021;14:5059–5077. doi:10.2147/JIR.S327014
14. Chopard R, Albertsen I, Piazza G. Diagnosis and Treatment of Lower Extremity Venous Thromboembolism: a Review. JAMA. 2020;324(17):1765–1776. doi:10.1001/jama.2020.17272
15. Gok M, Kurtul A. A novel marker for predicting severity of acute pulmonary embolism: systemic immune-inflammation index. Scand Cardiovasc J. 2021;55(2):91–96. doi:10.1080/14017431.2020.1846774
16. Uslu M, Yilmaz M, Ateşçelik M, FA A. The utility of the systemic immune inflammation and systemic inflammation response indices in suspected intermediate-risk pulmonary embolism. Croat Med J. 2024;65(1):13–19. doi:10.3325/cmj.2024.65.13
17. Zhang J, Fang Y, Pang H, et al. Association of age-adjusted D-dimer with deep vein thrombosis risk in patients with spinal cord injury: a cross-sectional study. Spinal Cord. 2022;60(1):90–98. doi:10.1038/s41393-021-00647-z
18. Zhang J, Chen Y, Wang Z, Chen X, Liu Y, Liu M. Anatomic distribution of lower extremity deep venous thrombosis is associated with an increased risk of pulmonary embolism: a 10-year retrospective analysis. Front Cardiovasc Med. 2023;10:1154875. doi:10.3389/fcvm.2023.1154875
19. Shang Z, Wanyan P, Zhang B, Wang M, Wang X. Incidence and risk factors of deep vein thrombosis in patients with spinal cord injury: a systematic review with meta-analysis. Front Cardiovasc Med. 2023;10:1153432. doi:10.3389/fcvm.2023.1153432
20. Zeng G, Li X, Li W, et al. A nomogram model based on the combination of the systemic immune-inflammation index, body mass index, and neutrophil/lymphocyte ratio to predict the risk of preoperative deep venous thrombosis in elderly patients with intertrochanteric femoral fracture: a retrospective cohort study. J Orthop Surg Res. 2023;18(1):561. doi:10.1186/s13018-023-03966-4
21. Lv X, Gao X, Liu J, et al. Immune-mediated inflammatory diseases and risk of venous thromboembolism: a Mendelian randomization study. Front Immunol. 2022;13(1):1042751. doi:10.3389/fimmu.2022.1042751
22. Chen X, Fan Y, Tu H, Chen J, Li R. A nomogram model based on the systemic immune-inflammation index to predict the risk of venous thromboembolism in elderly patients after Hip fracture: a retrospective cohort study. Heliyon. 2024;10(6):e28389. doi:10.1016/j.heliyon.2024.e28389
23. Melinte RM, Arbănași EM, Blesneac A, et al. Inflammatory Biomarkers as prognostic factors of acute deep vein thrombosis following the total knee arthroplasty. Medicina. 2022;58(10):1502. doi:10.3390/medicina58101502
24. Siddiqui F, García-Ortega A, Kantarcioglu B, et al. Cellular Indices and outcome in patients with acute venous thromboembolism. Clin Appl Thromb Hemost. 2022;28:1309672446. doi:10.1177/10760296221113346
25. Chen X, Ou Y, Wang Z, Liu H, Liu Y, Liu M. Association between systemic immune-inflammation index and risk of lower extremity deep venous thrombosis in hospitalized patients: a 10-year retrospective analysis. Front Cardiovasc Med. 2023;10:1211294. doi:10.3389/fcvm.2023.1211294
26. Koupenova M, Clancy L, Corkrey H, Freedman J. Circulating Platelets as Mediators of Immunity, Inflammation, and Thrombosis. Circ Res. 2018;122(2):337–351. doi:10.1161/CIRCRESAHA.117.310795
27. Ince L, Weber J, Scheiermann C. Control of Leukocyte Trafficking by Stress-Associated Hormones. Front Immunol. 2018;9(1):3143. doi:10.3389/fimmu.2018.03143
28. Huang SL, Xin HY, Wang XY, et al. Recent Advances on the Molecular Mechanism and Clinical Trials of Venous Thromboembolism. J Inflamm Res. 2023;16:6167–6178. doi:10.2147/JIR.S439205
29. Yao M, Ma J, Wu D, et al. Neutrophil extracellular traps mediate deep vein thrombosis: from mechanism to therapy. Front Immunol. 2023;14:1198952. doi:10.3389/fimmu.2023.1198952
30. Zhou Y, Xu Z, Liu Z. Impact of Neutrophil Extracellular Traps on Thrombosis Formation: new Findings and Future Perspective. Front Cell Infect Microbiol. 2022;12:910908. doi:10.3389/fcimb.2022.910908
31. Engelmann B, Massberg S. Thrombosis as an intravascular effector of innate immunity. Nat Rev Immunol. 2013;13(1):34–45. doi:10.1038/nri3345
32. Thålin C, Hisada Y, Lundström S, Mackman N, Wallén H. Neutrophil Extracellular Traps: villains and Targets in Arterial, Venous, and Cancer-Associated Thrombosis. Arterioscler Thromb Vasc Biol. 2019;39(9):1724–1738. doi:10.1161/ATVBAHA.119.312463
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.