Back to Journals » Clinical Ophthalmology » Volume 18
Relationship of Corneal Biomechanics Measured by Corvis ST and Optic Nerve Head Parameters in Healthy Saudi Females
Authors Elagamy A , Alnasser HK, Alghamdi WS, Berika M , Aldisi D
Received 14 May 2024
Accepted for publication 2 September 2024
Published 9 October 2024 Volume 2024:18 Pages 2851—2863
DOI https://doi.org/10.2147/OPTH.S469150
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Amira Elagamy,1,2 Hessa Khaled Alnasser,3 Wafa Saeed Alghamdi,3 Mohamed Berika,4,5 Dara Aldisi6
1Department of Optometry and Vision Sciences, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia; 2Mansoura Ophthalmic Center, Faculty of Medicine, Mansoura University, Mansoura, Egypt; 3College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia; 4Rehabilitation Science Department, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia; 5Anatomy Department, Faculty of Medicine, Mansoura University, Mansoura, Egypt; 6Community Health Sciences Department, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia
Correspondence: Amira Elagamy, Department of Optometry and Vision Sciences, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia, Email [email protected]
Aim: This study assessed the correlation between corneal biomechanical properties measured with Corvis ST (CST) and retinal nerve fiber layer thickness profile, anterior lamina cribrosa surface depth, and other optic nerve head parameters in healthy Saudi females.
Methods: This study included 62 eyes (only right eyes) of 62 healthy Saudi females aged from 20 to 39 yrs. A complete ophthalmologic assessment was performed for all participants. In addition, corneal biomechanical parameters were measured using CST, and optic nerve head parameters were evaluated using spectral domain optical coherence tomography.
Results: This study demonstrated a significant weak positive correlation between circumpapillary retinal nerve fiber layer (cpRNFL) peak angle and only second applanation (A2) length (mm) (r = 0.293, P = 0.021). Also, this study reported a significant moderate negative association between the C/D ratio and radius (r = − .513, P = 0.015). However, there was no significant correlation between corneal biomechanics and ALCSD in this study.
Conclusion: This study reported a significant positive correlation between cpRNFL peak angle and A2-length. In addition, the current study documented a significant moderate negative association between C/D ratio and radius. However, there was no significant correlation between ALCSD and the corneal biomechanical properties in this study. Further research is needed to verify the impact of corneal biomechanics on optic nerve head parameters and further investigate its role in the pathophysiology of glaucoma.
Keywords: corneal biomechanics, circumpapillary retinal nerve fiber layer peak angle, anterior lamina cribrosa surface depth
Introduction
The evaluation of corneal biomechanical properties has important implications for the diagnosis and management of glaucoma.1 It is essential to determine the risk factors for glaucoma progression to monitor patients with greater risk and to reserve visual acuity.2 The role of corneal biomechanics in glaucoma is yet to be fully understood and needs to be further investigated, although many studies3,4 evaluated the importance of corneal biomechanics in glaucoma patients and their significant contribution to the disease progression. Evaluation of optic nerve head (ONH) parameters is mandatory for an early diagnosis of glaucoma. In addition, their relationship to the corneal biomechanics needs to be investigated.5
Mansouri et al3 demonstrated a weak positive association between corneal hysteresis (CH), corneal resistance factor (CRF), and retinal nerve fiber layer thickness evaluated by scanning laser polarimetry (GDx enhanced corneal compensation (GDxECC)). However, no significant relationship was detected after adjusting the axial length (AL) and central corneal thickness (CCT) by age. Matsuura et al6 assessed the association between corneal biomechanics measured by Corneal Visualization Scheimpflug Technology (Corvis ST) (CST) and circumpapillary retinal nerve fiber layer (cpRNFL) peak angle between the supratemporal and infratemporal peaks measured by optical coherence tomography (OCT). They found a significant association between cpRNFL peak angle and only three CST variables. Their study was the only one that investigated this correlation which necessitates further evaluation for better understanding and validation. Bartolomé et al7 investigated the relationship between CH, CRF, Goldman-correlated intraocular pressure (IOPg), and corneal-compensated IOP (IOPcc) using the Ocular Response Analyzer (ORA) and anterior lamina cribrosa surface depth (ALCSD) and other biometric variables in healthy subjects. They reported no significant correlation between IOPcc, IOPg, CH, and ALCSD. No previous study examined the correlation between corneal biomechanics measured by CST and ALCSD and other ONH parameters in healthy Saudi subjects.
This study assessed the correlation between corneal biomechanical properties measured with CST and cpRNFL peak angle, ALCSD measured with OCT in healthy Saudi females. In addition, the association between the RNFL thickness profile and other variables, such as AL, CCT, and body height was performed. Furthermore, the relationship between ALCSD and other variables, such as age, spherical equivalent, IOP, CCT, and AL, was assessed.
Study Design
This study was a cross-sectional, prospective, non-randomized, and observational study. It got the Institutional Review Board (IRB) approval from Health Sciences Colleges Research on Human Subjects, College of Medicine, King Saud University, Riyadh, Saudi Arabia (No. E-22-6620). The study protocol adhered to tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants after the study procedures were explained.
Subjects and Methods
This study included 62 eyes (only right eyes) of 62 healthy Saudi females aged from 20 to 39 yrs. All subjects were recruited from King Saud University (KSU), female section, Riyadh, Saudi Arabia, by non-randomized convenience sampling method from February to April 2022. The study included healthy participants with best-corrected visual acuity of ≥20/20; IOP ≤ 21 mmHg without anti-glaucoma medications and normal-looking optic disc without any signs of glaucomatous or ischemic optic neuropathy. The study excluded participants who have a refractive error of more than 5 dioptres of the sphere and 3 dioptres of the cylinder, amblyopic eye, previous eye surgery including cataract or refractive surgery, neurological disease, macular degeneration, glaucoma or diabetes, ONH abnormalities. A comprehensive ophthalmologic examination was performed for all subjects. In addition, AL and CCT were measured using Oculus Pentacam HR for all participants. Also, body height was measured for each subject.
Corneal Biomechanical Parameters
Corneal biomechanical parameters were measured using CST with an automatic release mode. A high-speed Scheimpflug camera recorded the process of corneal deformation after applying an air impulse within 8.5 mm of the corneal apex. CST measurement was carried out three times, and the averages of CST parameters were calculated. CST quantifies twelve different parameters which include the biomechanical response of the cornea at the moment of the first and second applanations, (A1/2) time, A1/2 length, A1/2 velocity, A1/2 deformation amplitude, peak distance, highest deformation amplitude, highest concavity time and radius.6
Stereoscopic Disk Photography
Stereoscopic disk photography was obtained by spectral domain OCT (3D OCT-2000, Topcon. Fundus photography was gained in a dark room without mydriatic eye drops. RNFL thickness was measured using the RNFL 3.4 mm circle scan. The center of the scan circle was utilized as the disc’s center in the analysis. Then the temporal-superior-nasal-inferior-temporal (TSNIT) cpRNFL thickness curve was profiled to measure the angle between the ST and IT peaks of cpRNFL thickness profile. Then, the distance between ST and IT RNFL peaks was converted to an angular value by dividing it by the entire distance and multiplying by 360.6
The 3D image (6 × 6 mm) was recreated at first. Then, the three equidistant planes were made and defined as plane 1, plane 2, and plane 3. In this model, plane 2 corresponds to the mid-horizontal plane, and planes 1 and 3 correspond to the superior and inferior planes, respectively. ALCSD was measured at all planes, defined as the distance from the line connecting the two Bruch’s membrane opening (BMO) edges (reference line) to the anterior LC surface. It was measured in the direction perpendicular to the reference plane at three points: the maximum depth point and two additional points (100 and 200 μm apart from the maximum depth point to the temporal direction). The average of three measurements was taken as the ALCSD of each plane. The average of the ALCSDs from all planes was defined as the mean ALCSD of the eye.8
Statistical Analysis
Statistical Package for the Social Sciences (SPSS) version 21.0 software (SPSS Inc., NY, II, USA) was used for data analysis. The associations between the corneal biomechanical parameters and the cpRNFL peak angle, ALCSD, and the other variables were analyzed using linear regression analysis and Pearson’s Correlation coefficients. P < 0.05 was considered statistically significant.
Results
Sixty-two eyes were enrolled in this study. The mean age was 21.94 ± 3.67 (20–39) years. The mean spherical equivalent (SE) was −0.93 ± 1.16 (1.00 to −4.25) D. Moreover, the mean AL was 23.43 ± 1.09 mm (20.3–25.9) mm. The mean reported IOP was 17.76 ± 2.29 (13.6–21.0) mmHg. The mean CCT was 567.69 ± 31.07 (494–655) μm. The mean body height of the participants was 159.73 ± 5.8 (149–170) cm. The mean RNFL thickness was 113.14 ± 6.81 (101.0–124.0) μm. The mean disc area was 1.58–2.72 (1.58–2.72) mm². The mean C/D ratio was 0.30 ± 0.11 (0.09–0.51). In addition, the mean cpRNFL peak angle was 142.74 ± 20.24 (107–189) degrees. Figure 1 shows the circumpapillary retinal nerve fiber layer (cpRNFL) peak angle. Figure 2 displays a histogram for the distribution of participants within the study sample (n = 62) according to cpRNFL peak angle, this study shows that a higher number of participants (n = 18) reported cpRNFL peak angle between (123.4 to less than 139.8) degrees, and a lower share (n = 16) reported a cpRNFL peak angle between (139.8 to less than 156.2) degrees, and the lowest share of participants (n = 4) reported cpRNFL peak angle between (172.6 to 189) degrees.
 |
Figure 1 The Circumpapillary Retinal Nerve Fiber Layer (cpRNFL) Peak Angle. |
 |
Figure 2 Histogram of the Circumpapillary Retinal Nerve Fiber Layer (cpRNFL) Peak Angles (in Degrees). |
Regarding the measurement of ALCSD in this study, 40 eyes were excluded because of poor visibility of LC and difficult identification of the anterior LC surface in certain areas of the images due to prominent shadows of retinal blood vessels. Therefore, the ALCSD of only 22 eyes was measured. This study showed the mean ALCSD at the superior, middle, and inferior planes was 248.56 ± 88.87, 276.83 ± 106.06, and 214.11 ± 93.09 μm, respectively. The mean ALCSD was 246.35 ± 89.98 μm. Demographics and Clinical Data of the subjects are shown in Table 1. Descriptive statistics for corneal biomechanics parameters measured in this study are summarized in Table 2 and Figure 3 shows corneal biomechanical parameters measured using CST.
 |
Table 1 Demographics and Clinical Data of the Subjects (n = 62 Eyes) |
 |
Table 2 Descriptive Statistics of the Corneal Biomechanical Parameters Measured by Corvis ST |
 |
Figure 3 The Corneal Biomechanical Parameters Measured using Corvis-ST. |
This study demonstrated a significant weak positive correlation between cpRNFL peak angle and only A2-length (mm) (r = 0.293, P = 0.021). However, this study documented no significant correlation between cpRNFL peak angle and the other corneal biomechanical properties. Also, no significant correlation between cpRNFL peak angle and the other variables (age, SE, AL, CCT, IOP, body height) was reported in this study. The correlation between the cpRNFL peak angle and all variables is shown in Table 3. The adjusted R2 and corrected Akaike Information Criterion (AICc) measurements were used to evaluate the goodness of fit test for obtaining the optimum model predict cpRNFL peak angle based on this study sample which is to use A2-length parameter, with Beta coefficient = 13.723, P = 0.02. Tables 4 and 5 show multiple regression model results with cpRNFL as dependent variable. The linear fitting model shows that a rise of one (mm) in A2-Length leads to an increase of 13.72 degrees in the cpRNFL peak angle considering all other parameters are constant. Figure 4 shows the linear fitting model between the A2-Length and cpRNFL peak angle.
 |
Table 3 Correlation Between Circumpapillary Retinal Nerve Fiber Layer Peak Angle and All Variables |
 |
Table 4 Multiple Regression Model Results with Circumpapillary Retinal Nerve Fiber Layer Peak Angle as Dependent Variable |
 |
Table 5 Optimum Model Results with Circumpapillary Retinal Nerve Fiber Layer Peak Angle as Dependent Variable |
 |
Figure 4 The Linear Fitting Model between A2-Length (mm) and cpRNFL Peak Angle (Degrees). |
Pearson correlation analysis demonstrated that RNFL has a significant moderate negative association with AL (r = −.446, P = 0.037). The linear fitting model between the peripapillary RNFL thickness and AL shows that an increase of one mm unit in AL resulted in a decrease of 3.47 μm in RNFL thickness in this study sample. Figure 5 shows the linear fitting model between the peripapillary RNFL thickness and AL. Moreover, this study found a moderately positive association between the peripapillary RNFL thickness and CCT (r = 0.445, P = 0.038). The linear fitting model shows an increase of one mm unit in CCT resulting in a rise of 0.08 μm in RNFL thickness in this study sample. Figure 6 shows the linear fitting model between the peripapillary RNFL thickness and CCT.
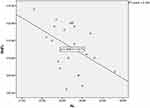 |
Figure 5 The Linear Fitting Model between the Peripapillary Retinal Nerve Fiber Layer Thickness (μm) and the Axial Length (mm). |
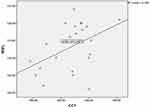 |
Figure 6 The linear fitting model between the Peripapillary Retinal Nerve Fiber Layer Thickness (μm) and Central Corneal Thickness (μm). |
Regarding the correlation between corneal biomechanics and ONH parameters: This study documented only a significant moderate negative association between the C/D ratio and radius (r = −.513, P = 0.015). Figure 7 shows the linear fitting model between the C/D ratio and radius. Radius is defined as the central curvature radius at the highest concavity. The linear fitting model between radius (μm) and C/D ratio shows an increase of 0.1 in C/D ratio resulting in a decrease of 4.58 mm in radius of this study sample. However, there was no significant correlation between the corneal biomechanics and ALCSD. Figure 8 shows ALCSD measured by spectral domain OCT. Furthermore, no significant association was detected between ALCSD and the other variables in this study. Table 6 shows descriptive statistics of ALCSD and the other ONH parameters. Table 7 shows the correlation between ALCSD, the other ONH parameters, and the other variables. Table 8 shows the correlation between the corneal biomechanics, ALCSD, and the other ONH parameters. On the other hand, IOP reported a significant strong positive correlation with A1-time (ms) (r = 0.938, P < 0.001), a strong negative correlation with A1-V (ms) (r = −.854, P < 0.001), a moderately negative correlation with highest concavity deformation amplitude (mm) (r = −.766, P < 0.001). Furthermore, this study found a significant moderate positive association correlation between CCT (μm) and A2-length (mm) (r = 0.522, P = 0.013).
 |
Table 6 Descriptive Statistics of ALCSD and the Other Nerve Head Parameters (n = 22 Eyes) |
 |
Table 7 Correlation between ALCSD and the Other Optic Nerve Head Parameters and the Other Variables (n = 22) |
 |
Table 8 Correlation Between the Corneal Biomechanics and ALCSD and the Other Nerve Head Parameters |
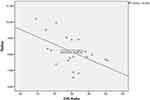 |
Figure 7 The Linear Fitting Model between Radius (mm) and C/D Ratio. |
 |
Figure 8 Anterior Lamina Cribrosa Surface Depth (ALCSD) Measured by Spectral Domain OCT. |
Discussion
This study found that the mean cpRNFL peak angle was 142.74 ± 20.24 (107–189) degrees compared to 130.6 ± 25.4 (77.8–207.0) degrees in Matsuura et al6. The current study demonstrated a significant weak positive correlation between cpRNFL peak angle and only A2-length. A2-length is defined as the length of the flattened cornea at the second applanation. However, Matsuura et al6 reported a significant correlation between cpRNFL peak angle and A1-length, A1-time, and A2-time. “A1/2 time” is defined as the length of time from the initiation of the air puff to the first (cornea moves inwards) or second applanation (cornea moves outwards). A1-length is defined as the length of the flattened cornea at the first applanation. Matsuura et al6 evaluated the cpRNFL peak angle and its relations in 97 eyes of 97 young healthy Japanese volunteers compared to 62 eyes of 62 healthy Saudi females in our study. This variance in ethnicity and sample size may explain the dissimilar findings of the two studies.
The current study reported no statistically significant correlation between cpRNFL peak angle and AL. Conversely, Matsuura et al6 reported a significant correlation between cpRNFL peak angle and AL. This finding can be explained by the small AL 23.43 ± 1.09 (20.3–25.9) mm in our study compared to the longer AL 25.2 ± 1.3 (22.6–28.5) mm in their research. Matsuura et al6 confirmed that cpRNFL peak angle was shallower in eyes with longer AL which was in agreement with Yoo et al.9 They suggested that eyes with poor corneal energy absorption evidenced by shorter A1-length, shorter A1-time, and shorter A2-time have sharp stretched posterior pole of retina demonstrated by shallow cpRNFL peak angle away from the influence of elongated AL. Understanding the impact of corneal biomechanics on cpRNFL thickness profiles is important to recognize retinal structure in eyes with myopia and structural changes in glaucomatous eyes and it needs more attention.
This study showed the mean ALCSD (22 eyes) was 246.35 ± 89.98 μm compared to 371.88 ± 114.62 μm in Elagamy et al10. Bartolomé et al7 reported mean ALCSD (74 eyes) was 329.15 ± 60.85 µm. Furlanetto et al10 demonstrated that the mean ALCSD (57 eyes) was 353 ± 70 µm. The differences in ALCSD may be explained by the different sample sizes in these studies.
This study found a significant moderate negative association between the C/D ratio and radius. Radius is defined as the central curvature radius at the highest concavity. However, our study discovered no association between corneal biomechanics and optic disc area. This finding matched Insull et al11 who reported no correlation between optic disc area and CH.
No significant correlation between corneal biomechanics measured by CST and ALCSD was detected in this study. Bartolomé et al7 measured corneal biomechanics by ORA. They reported only a significant weak association between CRF and lamina cribrosa thickness (r = 0.264; P = 0.045). However, they did not demonstrate any relationship between ALCSD and IOPcc, IOPg, CH. On the other hand, Sun et al12 evaluated the relationship between corneal stiffness parameters and LC curvature in normal tension glaucoma. They used the mean adjusted LC curvature index (maLCCI) to measure LCD by swept-source optical coherence tomography (SS-OCT). However, in this study, ALCSD was measured from the BMO reference plane to the surface of anterior LC by spectral domain OCT (3D OCT-2000, Topcon). Unlike ALCSD, the maLCCI does not depend on the variations in BMO location. They demonstrated that younger age (P = 0.010), thinner CCT (P = 0.002), and lower stiffness parameters at applanation 1 (SP-A1) (P < 0.001) were significantly associated with greater maLCCI. Furthermore, no significant association was detected between ALCSD and the other variables in this study, such as age, SE, IOP, and CCT. This finding matched Elagamy et al13 and Seo et al8 who did not detect any correlation between ALCSD and age, refractive errors, IOP, CCT, or disk area. In addition, this study and Elagamy et al13 confirmed that ALCSD did not correlate with AL. This result mismatched Seo et al8 study that found a significant negative correlation between ALCSD and AL. They included subjects with AL > 25 mm (high myopic eye, ≥−8.0 D). The mean AL in our study and Elagamy et al13 was 23.43 ± 1.09 mm and 23.50 ± 0.872, respectively. This disagreement may be explained by the differences in mean AL between the studies. Furthermore, no significant association between ALCSD and RNFL was reported in the current study. This result matched Elagamy et al13 and Ren et al14.
Pearson correlation analysis demonstrated that the peripapillary RNFL thickness has a significant moderate negative association with AL. Yoo et al9 and Porwal et al15 confirmed the significant association between the peripapillary RNFL thickness and AL.
Moreover, this study found a significant moderate positive association between the peripapillary RNFL and CCT. Mohamed et al16 documented a significant positive association between the CCT and RNFL thickness (r = 0.621, P ≤ 0.001). However, this result disagreed with Pakravan et al17 who found no correlation between the peripapillary RNFL thickness and CCT (P = 0.66). On the other hand, no association between the corneal biomechanics and the peripapillary RNFL thickness was found in our study. This result agreed with Mansouri et al3 who did not confirm any significant association between CH and CRF and retinal nerve fiber layer thickness measured by GDxECC after modifying CCT and AL by age.
IOP in this study showed a significant strong positive correlation with A1-time, a strong negative correlation with A1-V, and a moderately negative correlation with the highest concavity deformation amplitude. In agreement with our findings, Asaoka et al18 found that IOP measured with Goldmann applanation tonometry (IOP-G) showed a positive correlation with A1-time, a negative correlation with A1-V, and maximum deformation amplitude. Furthermore, this study found a significant moderate positive association between CCT and A2-length. This finding matched Asaoka et al18 who confirmed that CCT was a predictor of A2-length.
This study has the following limitations. First, all participants were Saudi females; hence, the findings might not apply to males in Saudi Arabia and other countries. Second, the small sample size was another limitation due to a technical error in CST which forced us to stop data collection. Third, the inability to measure ALCSD in many eyes due to poor visibility of the anterior LC surface and the limitation of Topcon 3D OCT-2000.
Conclusion
This study reported a significant positive correlation between cpRNFL peak angle and A2-length. In addition, the current study documented a significant moderate negative association between C/D ratio and radius. However, there was no significant correlation between ALCSD and the corneal biomechanical properties in this study. Evaluation of the association between ALCSD and corneal biomechanics may help to understand the impact of the corneal biomechanical parameters on lamina cribrosa depth and thickness. Further studies are recommended on larger study populations including males, different ethnic populations, high myopic eyes, glaucomatous eyes, and different age groups using advanced imaging techniques, such as swept-source OCT or enhanced depth imaging OCT, to verify the impact of corneal biomechanics on ONH parameters and further investigate its role in the pathophysiology of glaucoma.
Acknowledgment
The authors extend their appreciation to the Researchers Supporting Project number (RSPD2024R716), King Saud University, Riyadh, Saudi Arabia.
Funding
This project was funded by the Researchers Supporting Project number (RSPD2024R716), King Saud University, Riyadh, Saudi Arabia.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chong J, Dupps WJ. Corneal biomechanics: Measurement and structural correlations. Exp. Eye Res. 2021;205:108508. doi:10.1016/j.exer.2021.108508
2. Pillunat KR, Hermann C, Spoerl E, et al. Analyzing biomechanical parameters of the cornea with glaucoma severity in open-angle glaucoma. Graefes Arch Clin Exp Ophthal. 2016;254(7):1345–1351. doi:10.1007/s00417-016-3365-3
3. Mansouri K, Leite MT, Weinreb RN, et al. Association between corneal biomechanical properties and glaucoma severity. Am J Ophthalmol. 2012;153(3):419–427. doi:10.1016/j.ajo.2011.08.022
4. Matsuura M, Hirasawa K, Murata H, et al. The usefulness of CorvisST Tonometry and the Ocular Response Analyzer to assess the progression of glaucoma. Sci Rep. 2017;7(1):40798. doi:10.1038/srep40798
5. Yamashita T, Asaoka R, Kii Y, et al. Structural parameters associated with location of peaks of peripapillary retinal nerve fiber layer thickness in young healthy eyes. PLoS One. 2017;12(5):e0177247. doi:10.1371/journal.pone.0177247
6. Matsuura M, Murata H, Nakakura S, et al. The relationship between retinal nerve fibre layer thickness profiles and CorvisST tonometry measured biomechanical properties in young healthy subjects. Sci Rep. 2017;7:414. doi:10.1038/s41598-017-00345-y
7. Bartolomé F, Martínez de la Casa J, Camacho I, et al. Correlating Corneal Biomechanics and Ocular Biometric Properties with Lamina Cribrosa Measurements in Healthy Subjects. Semi Ophthalmol. 2018;33(2).
8. Seo JH, Kim TW, Weinreb RN. Lamina cribrosa depth in healthy eyes. Invest Ophthalmol Vis Sci. 2014;55(3):1241–1250. doi:10.1167/iovs.13-12536
9. Yoo YC, Lee CM, Park JH. Changes in peripapillary retinal nerve fiber layer distribution by axial length. Optom Vis Sci. 2012;89:4–11. doi:10.1097/OPX.0b013e3182358008
10. Furlanetto RL, Park SC, Damle UJ, et al. Posterior displacement of the lamina cribrosa in glaucoma: in vivo interindividual and intereye comparisons. Invest Ophthalmol Vis Sci. 2013;54(7):4836–4842. doi:10.1167/iovs.12-11530
11. Insull E, Nicholas S, Ang GS, et al. Optic disc area and correlation with central corneal thickness, corneal hysteresis and ocular pulse amplitude in glaucoma patients and controls. Clin Experim Ophthalmol. 2010;38:839–844. doi:10.1111/j.1442-9071.2010.02373.x
12. Sun Y, Guo Y, Cao K, et al. Relationship between corneal stiffness parameters and lamina cribrosa curvature in normal tension glaucoma. European J Ophthal. 2020.
13. Elagamy A, Oteaf F, Berika M. Anterior Lamina Cribrosa Surface Depth in Healthy Saudi Females. Clin Ophthalmol. 2017;11:1045–1050. doi:10.2147/OPTH.S131612
14. Ren R, Yang H, Gardiner SK, et al. Anterior lamina cribrosa surface depth, age, and visual field sensitivity in the Portland Progression Project. Invest Opthalmol Vis Sci. 2014;55(3):1531. doi:10.1167/iovs.13-13382
15. Porwal S, Suneetha N, Joseph M, et al. Correlation of axial length and peripapillary retinal nerve fiber layer thickness measured by Cirrus HD optical coherence tomography in myopes. Indian J Ophthalmol. 2020;68(8):1584–1586. doi:10.4103/ijo.IJO_1778_19
16. Mohamed E, Basiony A, Ibrahim A. Correlation between central corneal thickness and retinal nerve fiber layer thickness in open-angle glaucoma. Delta J Ophthalmol. 2019;20(02):55–62. doi:10.4103/DJO.DJO_69_18
17. Pakravan M, Aramesh S, Yazdani S, et al. Peripapillary Retinal Nerve Fiber Layer Thickness Measurement by Three-Dimensional Optical Coherence Tomography in a Normal Population. J Ophthalmic Vis Res. 4(4).
18. Asaoka R, Nakakura S, Tabuchi H, et al. The Relationship between Corvis ST Tonometry Measured Corneal Parameters and Intraocular Pressure, Corneal Thickness and Corneal Curvature. PLoS One. 2015;20.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

