Back to Journals » Clinical Ophthalmology » Volume 19
Relationships of the Duration from Onset and Macular Morphology with Metamorphopsia After Surgery for Macula-Off Rhegmatogenous Retinal Detachment
Authors Sato T, Akagi T , Kobayashi D, Anraku A, Nozaki Y, Ando T , Yoshida H, Terashima H, Hasebe H, Fukuchi T
Received 15 December 2024
Accepted for publication 26 February 2025
Published 30 March 2025 Volume 2025:19 Pages 1119—1128
DOI https://doi.org/10.2147/OPTH.S512396
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tadanobu Sato,1 Tadamichi Akagi,1 Daigo Kobayashi,1 Akiko Anraku,2 Yohei Nozaki,1 Takumi Ando,1 Hiromitsu Yoshida,1 Hiroko Terashima,1 Hiruma Hasebe,2 Takeo Fukuchi1
1Division of Ophthalmology and Visual Science, Graduate School of Medical and Dental Sciences, Niigata University, Niigata, Japan; 2Department of Ophthalmology, Saiseikai Niigata Hospital, Niigata, Japan
Correspondence: Tadamichi Akagi, Division of Ophthalmology and Visual Science, Graduate School of Medical and Dental Sciences, Niigata University, 1-757, Asahimachi-dori, Chuo-ku, Niigata, 951-8510, Japan, Tel +81-25-227-2296, Fax: +81-25-227-0785, Email [email protected]
Purpose: To investigate the relationships among postoperative metamorphopsia and postoperative macular morphological changes and the duration from the onset of visual field disturbance to surgery (DVD) in patients who underwent surgery for macula-off rhegmatogenous retinal detachment (RRD).
Patients and Methods: We retrospectively reviewed 33 eyes of 33 patients who underwent pars plana vitrectomy (PPV) for macula-off RRD with known onset of symptoms of visual field disturbance at Niigata University Medical and Dental Hospital or Saiseikai Niigata Hospital and were followed up for at least 6 months postoperatively. Optical coherence tomography images of the macula obtained at 6 months postoperatively and DVD were analyzed, and the associations of the DVD with vertical metamorphopsia (vM) and horizontal metamorphopsia (hM) at 6 months postoperatively were evaluated using M-CHARTS.
Results: vM was significantly correlated with the DVD and ellipsoid zone (EZ) disruption (P = 0.004 and P = 0.008, respectively), while hM was significantly correlated only with the DVD (P = 0.018). vM was significantly smaller in eyes with a DVD ≤ 7 days (0.34 ± 0.35)) than in eyes with a DVD ≥ 8 days (0.69 ± 0.32) (P = 0.005). In the multivariate analyses, postoperative vM was significantly associated with EZ disruption and the DVD (≤ 7 or ≥ 8 days) (P = 0.012 and P = 0.014, respectively).
Conclusion: Metamorphopsia after PPV for macula off RRD was associated with the DVD and EZ disruption.
Keywords: pars plana vitrectomy, optical coherence tomography, vision disorders, macula-off rhegmatogenous retinal detachment
Introduction
Rhegmatogenous retinal detachment (RRD) has an incidence of 6.3 to 17.9 per 100,000 people and can lead to blindness if left untreated.1 RRD can be repaired through surgery in a high percentage of cases.2,3 However, even after retinal reattachment and visual acuity improvement, postoperative metamorphopsia can lead to poor patient satisfaction, particularly in patients who have undergone surgery for macula-off RRD.4–6
Previous studies using optical coherence tomography (OCT) have suggested that postoperative metamorphopsia and visual acuity are closely associated with postoperative morphological changes in the macula, including those concerned with the integrity of the external limiting membrane (ELM) and ellipsoid zone (EZ), irregularity of the interdigitation zone (IZ), and the thickness measured from the EZ to the retinal pigment epithelium (RPE) in patients who have undergone surgery for macula-off RRD.7–10 However, the association between postoperative metamorphopsia and these changes is yet to be fully understood.
One of the preoperative background factors, the duration from the onset of visual field disturbance to surgery (DVD), has been reported to be an important prognostic factor for visual acuity in patients with RRD.11,12 However, the association between postoperative metamorphopsia and DVD has not been well investigated. Metamorphopsia, quantitatively assessed using M-CHARTS, was reported to be strongly associated with the vision-related quality of life in patients with epiretinal membrane (ERM).13 In the present study, we investigated the associations among postoperative metamorphopsia assessed using M-CHARTS and postoperative macular morphological and DVD in patients who underwent surgery for macula-off RRD.
Patients and Methods
This retrospective, observational study was approved by the Research Ethics Committee of Niigata University Hospital (IRB No. 2021–0166) and adhered to the tenets of the Declaration of Helsinki. We included 33 eyes of 33 consecutive patients who underwent uncomplicated pars plana vitrectomy (PPV) for primary macula-off RRD between April 2021 and January 2024 at Niigata University Hospital or Saiseikai Niigata Hospital. The exclusion criteria were unknown onset of symptoms of visual field disturbance, concomitant scleral buckling, history of intraocular surgery other than cataract surgery and presence of diabetic retinopathy, age-related macular degeneration, ocular trauma, proliferative vitreoretinopathy, macular hole (MH), preoperative ERM, very severe vitreous hemorrhage that prevented fundus observation, or cases that required re-operation during the course of treatment. Preoperatively, all patients underwent a comprehensive ophthalmic examination, including best-corrected visual acuity (BCVA) assessment, dilated slit-lamp examination, axial length measurement (IOLMaster 500, Carl Zeiss Meditec, Dublin, CA, USA), fundus photography, and swept-source OCT (SS-OCT) (Deep-Range Imaging [DRI] Triton, Topcon, Tokyo, Japan). A complete medical history, including that regarding the DVD, was recorded. One month after surgery, the axial length measurement was repeated for accuracy and was used for analysis. All patients underwent ophthalmic examinations, including BCVA assessment, vertical and horizontal M-CHARTS assessments, dilated slit-lamp examination, fundus photography, and SS-OCT, at 1, 3, and 6 months postoperatively.
PPV was performed under sub-tenon anesthesia, followed by core and peripheral vitrectomy, subretinal fluid drainage, fluid-air exchange, retinal photocoagulation, and sulphur hexafluoride (SF6) gas tamponade. Internal limiting membrane (ILM) peeling was not performed in any case. PPV was combined with phacoemulsification and foldable acrylic IOL implantation in 22 patients with cataracts or those over 60 years of age.
DVD was defined as the time from the date of onset of visual field disturbance to the date of surgery. Eyes were included in this study only if the DVD was accurately documented for a specific 24-hour period.
M-CHARTS was used to evaluate metamorphopsia. M-CHARTS consists of straight and dotted lines as test indices with a total visual angle of 20°, individual dots with a visual angle of 0.1°, a fixation point with a visual angle of 0.3°, and 19 dashed lines with increasing distances between dots ranging from 0.2 to 2.0°.14,15 The test was performed vertically and horizontally by rotating the test chart to 90°.
Imaging
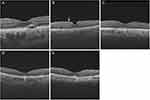
SS-OCT was performed after mydriasis. Twelve radial B-scan images (12 mm) centered on the fovea were acquired. Speckle noises were reduced by averaging 16 B-scans to improve image quality. SS-OCT images were evaluated for central retinal thickness (CRT), presence of cystoid macular oedema (CME), subretinal fluid (SRF), ERM, ELM disruption, EZ disruption, and IZ disruption (Figure 1A-1E). CRT was defined as the average of a 6-mm diameter area centered on the fovea. CME and ERM were classified based on their presence or absence within a 6-mm diameter area centered on the fovea. The status of the ELM, EZ, and IZ was evaluated to determine whether it was continuous or disrupted in the horizontal and vertical scan images within a 6-mm diameter area centered on the fovea, as reported previously.7 Disruption was defined if the ELM, EZ, or IZ was not continuous in either of these images. SRF was classified according to its presence or absence in the fovea. All gradings were performed by two authors (T.S. and D.K). Both graders were blinded to patients’ clinical findings, including visual acuity and metamorphopsia. If a disagreement between the graders occurred, both of them reviewed the OCT image of another adjacent slice, and a third adjudicator (T.A.) determined the grade.
Statistical Analyses
All continuous variables are represented as mean ± standard deviation (SD) values. The Shapiro–Wilk test was performed to assess whether continuous variables were normally distributed. Differences in BCVA, vertical metamorphopsia (vM), and horizontal metamorphopsia (hM) at 1, 3, and 6 months postoperatively were determined using the Kruskal–Wallis test and repeated-measures analysis of variance (ANOVA), and a post hoc test was performed to compare between measurements at 1 month and 3 months or 1 month and 6 months using Wilcoxon rank-sum tests. Spearman’s rank correlation coefficient analysis was performed to assess the correlations among vM and hM and various parameters. Differences in vM, hM, and various parameters between groups were analyzed using the Mann–Whitney U or Fisher’s exact test. Statistical significance was defined as P < 0.05. Bonferroni correction was used to assess vM, hM, and the DVD. For the calculation of the cumulative mean metamorphopsia score: if the DVD is x (days), the cumulative mean vertical metamorphopsia score is the average value of vM from DVD 1 to x. All statistical analyses were performed using IBM SPSS version 29.0 (SPSS Inc., Chicago, IL, USA).
Results
This study included 33 eyes of 33 patients (Table 1). The mean age was 60.9 ± 10.4 years, and the mean DVD was 7.9 ± 4.8 days (range 1–22 days). All eyes showed macula-off RRD, extending to three or more quadrants in 13 eyes and two or less quadrants in 20 eyes. Six eyes were pseudophakic, and 22 eyes underwent PPV combined with phacoemulsification and intraocular lens implantation.
 |
Table 1 Patient Characteristics |
Table 2 summarizes postoperative longitudinal changes in BCVA (logMAR) and M-CHARTS scores. BCVAs in PPV alone and in PPV combined with cataract surgery at 6 months postoperatively were 0.07±0.15 and −0.00±0.10, respectively, which were not significantly different (P = 0.28). Both BCVA and metamorphopsia improved over 6 months postoperatively. BCVA, vM, and hM results were divided into three groups each at 1, 3, and 6 months postoperatively, respectively, and significant differences in BCVA and hM (P = 0.026 and P = 0.013, respectively) were observed. The BCVA results at 3 and 6 months postoperatively were significantly better than those at 1 month postoperatively (P = 0.016 and P < 0.001, respectively). The hM scores were significantly lower at 6 months than at 1 month postoperatively (P < 0.001), whereas changes in vM scores were not significant (P > 0.05).
 |
Table 2 Postoperative Longitudinal Changes in Best-Corrected Visual Acuity and Metamorphopsia |
Table 3 shows the correlations between metamorphopsia and patient characteristics, including OCT parameters, at 6 months postoperatively. The mean CRT at 6 months postoperatively was 0.28 ± 0.02 mm. There were no patients with central macular oedema at 6 months postoperatively. SRF, ERM, ELM disruption, EZ disruption, and IZ disruption were observed in six, nine, six, 19, and 29 eyes, respectively, at 6 months postoperatively. vM at 6 months postoperatively had significant positive correlations with DVD and EZ disruption (P = 0.004 and P = 0.008, respectively). hM at 6 months postoperatively was significantly correlated only with DVD (P = 0.018). The other variables were not significantly associated with metamorphopsia at 6 months postoperatively.
 |
Table 3 Factors Associated with Vertical Metamorphopsia and Horizontal Metamorphopsia After Six Months Postoperatively |
Figure 2 shows the relationship between the cumulative mean vM at 6 months postoperatively and DVD. The differences in metamorphopsia (vM and hM) at 6 months postoperatively, when classified based on the DVD, are shown in Table 4. Patients with a DVD of 7 days or less had significantly better postoperative vM than those with a DVD of 8 days or more, even after Bonferroni correction (0.34 ± 0.35 vs 0.69 ± 0.32, P = 0.005; α = 0.007). Between these two groups (DVD ≤ 7 days and DVD ≥ 8 days), a significant difference was not observed in any baseline characteristics (age, sex, axial length, preoperative BCVA, presence or absence of combination with cataract surgery, extent of RRD) and postoperative parameters (CRT, SRF, ERM, ELM disruption, EZ disruption, IZ disruption and BCVA) at 6 months postoperatively.
 |
Table 4 Metamorphopsia at Six Months After Surgery Based on the Duration from the Onset of Visual Field Disturbance to Surgery |
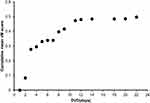 |
Figure 2 An association between the duration from the onset of visual field disturbance to surgery and cumulative mean vertical metamorphopsia score. |
Table 5 shows relationships between OCT macular status and metamorphopsia at 6 months postoperatively. vM at 6 months postoperatively was related to EZ disruption (0.26 ± 0.28 vs 0.65 ± 0.37, P = 0.008). The other macular status factors were not significantly associated with metamorphopsia at 6 months postoperatively.
 |
Table 5 Factors of Macular Status Related to Metamorphopsia at Six Months Postoperatively |
Univariate and multivariate analyses of the associations between vM at 6 months postoperatively and the DVD and EZ disruption are presented in Table 6. Univariate analysis showed that postoperative vM was significantly associated with the DVD (days; P = 0.040) and the DVD (≤ 7 or ≥ 8 days; P = 0.008) and EZ disruption (P = 0.007). In the multivariate analyses, postoperative vM was significantly associated with EZ disruption and the DVD (≤ 7 or ≥ 8 days) (P = 0.012 and P = 0.014, respectively).
 |
Table 6 Regression Analysis for Vertical Metamorphopsia at Six months Postoperatively |
Discussion
In the present study, postoperative BCVA and hM improved over the first 6 months, unlike postoperative vM, in patients who underwent PPV for macula-off RRD. vM and hM were significantly correlated with the DVD at 6 months postoperatively. Even in multiple regression analysis, the DVD, as well as EZ disruption, was significantly associated with vM.
The duration from the symptom onset has been suggested as a preoperative factor associated with visual acuity after macula-off RRD surgery.16,17 Surgical repair within 6 days of symptom onset improves visual acuity.11 Early surgical treatment within 3 days of the onset of macular detachment is recommended to improve postoperative visual acuity.12 However, no studies have focused on the effect of the duration from symptom onset to surgery on metamorphopsia after surgery for macula-off RRD. In one of the previous studies investigating postoperative metamorphopsia assessed using the Amsler grid in patients who underwent surgery for macula-off RRD, the mean DVD was 56.5 days (range, 4–365 days) in the group with metamorphopsia and 52.0 days (range, 6–300 days) in the group without metamorphopsia, which was not significantly different.10 In the present study, the mean DVD was much shorter than that observed in the previous study, and the method of evaluating metamorphopsia was different, which might explain the difference. In another study, the mean period from the onset of symptoms (either sudden floaters, visual field loss, or subjective visual loss) was 4.9 days in the group with an M-CHARTS score greater than 0.2 and 8.6 days in the group with an M-CHARTS score less than 0.2, which was not significantly different.18 In the present study, we did not consider the awareness of floaters to assess the duration of illness. The vM at 6 months postoperatively was significantly better when the DVD was 7 days or less than when the DVD was 8 days or more.
In the present study, postoperative metamorphopsia was associated with macular status. Postoperative vM was significantly associated with EZ disruptions. Differences in the outer retinal layers, such as the ELM, EZ, and IZ, have been reported to be related to metamorphopsia after surgery for macula-off RRD.7–10 Saleh et al reported that the parafoveal cone density was lower in eyes that underwent surgery for macula-off RRD than in fellow eyes.19 These changes in the morphology of the outer retinal layer indicate abnormalities of cones and synapses and may be implicated in the development of metamorphopsia. The present study found significant differences in vM, but not in hM, in the presence of abnormalities in outer retinal layers. Fukuyama et al reported that folds in the outer retinal layer decreased over time after retinal restoration in patients with macula-off RRD. The horizontal fold density decreased over time, whereas the vertical fold density did not.20 The vector of folds in the outer retina after retinal restoration may result in the difference in temporal changes in vertical and horizontal metamorphopsia during the period from the appearance of visual field disturbances to surgery and in the presence or absence of EZ disruption. In addition, retinal displacement detected by fundus autofluorescence imaging is reported to be common and a major cause of metamorphopsia after PPV for RRD.21,22 En face OCT imaging has also been proposed for the assessment of EZ.23 Future studies using multimodal imaging may help clarify the relationship between metamorphopsia and retinal morphology.
vM and hM revealed different characteristics. Longitudinal improvement was significant in hM, but not in vM, at 6 months postoperatively, and EZ disruption was significantly associated with vM but not with hM. Although some previous studies have reported longitudinal improvements in both vM and hM after PPV for macula-off RRD,7,9,20 different features of vM and hM have been suggested in other diseases. For example, in macular holes, vM was reported to be consistently higher and correlated better with the BCVA and duration of symptoms than hM.24,25 Although the mechanisms of vM and hM have not been well clarified, vM might have correlated with superior perifoveal deformation of the vertical line on the fovea, and hM might have correlated with temporal perifoveal deformation of the horizontal line on the fovea.26 Further investigation is essential to clarify the mechanisms underlying the differences between vM and hM.
Morphological factors associated with metamorphopsia may vary among diseases. In patients with ERM, the structure of the inner retinal layer, including the thickness of the inner nuclear layer and ectopic inner foveal layer, was observed to be closely associated with preoperative and postoperative metamorphopsia.27–29 CRT has also been suggested to be associated with metamorphopsia in patients with ERM; however, in the present study, no significant correlation between CRT and metamorphopsia was observed in patients with RRD. Although the mechanism underlying metamorphopsia is not fully understood, its causes may vary among diseases.
The present study has several limitations. The first is the possible imprecision of the DVD. Symptom onset was determined when the patient was aware of visual field impairment. At that time, the RRD likely extended within the vascular arcade in most patients. A macular detachment was observed in all patients during the initial examination. However, the extent of RRD at the symptom onset and the exact timing of foveal involvement were unclear. Second, the sample size was extremely small, and the follow-up period was short. One of the main reasons for the small sample size was that we could obtain accurate histories from only a limited number of patients. Further prospective studies with large samples are warranted to validate these results.
Conclusion
Longer DVD and presence of EZ disruption were related to vM at 6 months postoperatively. It is recommended that patients be fully informed of the possibility of not only poor postoperative visual acuity but also metamorphopsia, especially in cases where the period after onset is long.
Data Sharing Statement
The data used to support the findings of this study are available on request from the corresponding author.
Ethics Approval and Informed Consent
This retrospective, observational study was approved by the Research Ethics Committee of Niigata University Hospital (IRB No. 2021-0166) and adhered to the tenets of the Declaration of Helsinki. In this study, informed consent was not obtained from each patient because of the retrospective, observational nature of the study; however, patients were given the option to withdraw consent at any time in an opt-out manner.
Acknowledgments
We would like to thank Editage (www.editage.co.kr) for English language editing.
Author Contributions
All authors made a significant contribution to the work reported, either in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors have not declared any grant for this work from any funding authority.
Disclosure
The authors report no conflict of interest in this work.
References
1. Mitry D, Charteris DG, Fleck BW, Campbell H, Singh J. The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol. 2010;94(6):678–684. doi:10.1136/bjo.2009.157727
2. Miller DM, Riemann CD, Foster RE, Petersen MR. Primary repair of retinal detachment with 25-gauge pars plana vitrectomy. Retina. 2008;28(7):931–936. doi:10.1097/IAE.0b013e31816b313a
3. Wong CW, Wong WL, Yeo IYS, et al. Trends and factors related to outcomes for primary rhegmatogenous retinal detachment surgery in a large Asian tertiary eye center. Retina. 2014;34(4):684–692. doi:10.1097/IAE.0b013e3182a48900
4. Koriyama M, Nishimura T, Matsubara T, Taomoto M, Takahashi K, Matsumura M. Prospective study comparing the effectiveness of scleral buckling to vitreous surgery for rhegmatogenous retinal detachment. Jpn J Ophthalmol. 2007;51(5):360–367. doi:10.1007/s10384-007-0463-0
5. Rossetti A, Doro D, Manfrè A, Midena E. Long-term follow-up with optical coherence tomography and microperimetry in eyes with metamorphopsia after macula-off retinal detachment repair. Eye. 2010;24(12):1808–1813. doi:10.1038/eye.2010.138
6. Okamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T. Metamorphopsia and optical coherence tomography findings after rhegmatogenous retinal detachment surgery. Am J Ophthalmol. 2014;157(1):214–220.e1. doi:10.1016/j.ajo.2013.08.007
7. Okuda T, Higashide T, Sugiyama K. Metamorphopsia and outer retinal morphologic changes after successful vitrectomy surgery for macula-off rhegmatogenous retinal detachment. Retina. 2018;38(1):148–154. doi:10.1097/IAE.0000000000001510
8. Murakami T, Okamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T. Changes in metamorphopsia and optical coherence tomography findings after successful retinal detachment surgery. Retina. 2018;38(4):684–691. doi:10.1097/IAE.0000000000001588
9. Xu S, Wang L, Kong K, Li G, Ni Y. Metamorphopsia and morphological changes in the macula after scleral buckling surgery for macula-off rhegmatogenous retinal detachment. J Ophthalmol. 2021;2021:5525049. doi:10.1155/2021/5525049
10. Kumar V, Naik A, Kumawat D, et al. Multimodal imaging of eyes with metamorphopsia after vitrectomy for rhegmatogenous retinal detachment. Indian J Ophthalmol. 2021;69(10):2757–2765. doi:10.4103/ijo.IJO_3658_20
11. Kim JD, Pham HH, Lai MM, Josephson JW, Minarcik JR, Von Fricken MV. Effect of symptom duration on outcomes following vitrectomy repair of primary macula-off retinal detachments. Retina. 2013;33(9):1931–1937. doi:10.1097/IAE.0b013e3182877a27
12. Miyake M, Nakao SY, Morino K, et al. Effect of duration of macular detachment on visual prognosis after surgery for macula-off retinal detachment: japan-Retinal Detachment Registry. Ophthalmol Retina. 2023;7(5):375–382. doi:10.1016/j.oret.2023.01.014
13. Okamoto F, Okamoto Y, Hiraoka T, Oshika T. Effect of vitrectomy for epiretinal membrane on visual function and vision-related quality of life. Am J Ophthalmol. 2009;147(5):869–874. doi:10.1016/j.ajo.2008.11.018
14. Matsumoto C, Arimura E, Okuyama S, Takada S, Hashimoto S, Shimomura Y. Quantification of metamorphopsia in patients with epiretinal membranes. Invest Ophthalmol Vis Sci. 2003;44(9):4012–4016. doi:10.1167/iovs.03-0117
15. Arimura E, Matsumoto C, Okuyama S, Takada S, Hashimoto S, Shimomura Y. Retinal contraction and metamorphopsia scores in eyes with idiopathic epiretinal membrane. Invest Ophthalmol Vis Sci. 2005;46(8):2961–2966. doi:10.1167/iovs.04-1104
16. Ross WH, Kozy DW. Visual recovery in macula-off rhegmatogenous retinal detachments. Ophthalmology. 1998;105(11):2149–2153. doi:10.1016/S0161-6420(98)91142-3
17. Hassan TS, Sarrafizadeh R, Ruby AJ, Garretson BR, Kuczynski B, Williams GA. The effect of duration of macular detachment on results after the scleral buckle repair of primary, macula-off retinal detachments. Ophthalmology. 2002;109(1):146–152. doi:10.1016/s0161-6420(01)00886-7
18. Yamada H, Imai H, Tetsumoto A, et al. The contribution of the proximity of the retinal detachment to the fovea for postoperative metamorphopsia after 27-gauge pars plana vitrectomy for the primary rhegmatogenous retinal detachment. PLoS One. 2021;16(10):e0258775. doi:10.1371/journal.pone.0258775
19. Saleh M, Debellemanière G, Meillat M, et al. Quantification of cone loss after surgery for retinal detachment involving the macula using adaptive optics. Br J Ophthalmol. 2014;98(10):1343–1348. doi:10.1136/bjophthalmol-2013-304813
20. Fukuyama H, Yagiri H, Araki T, et al. Quantitative assessment of outer retinal folds on enface optical coherence tomography after vitrectomy for rhegmatogenous retinal detachment. Sci Rep. 2019;9(1):2327. doi:10.1038/s41598-019-38751-z
21. Brosh K, Francisconi CLM, Qian J, et al. Retinal displacement following pneumatic retinopexy vs pars plana vitrectomy for rhegmatogenous retinal detachment. JAMA Ophthalmol. 2020;138(6):652–659. doi:10.1001/jamaophthalmol.2020.1046.
22. Schawkat M, Valmaggia C, Lang C, Scholl HPN, Guber J. Multimodal imaging for detecting metamorphopsia after successful retinal detachment repair. Graefes Arch Clin Exp Ophthalmol. 2020;258(1):57–61. doi:10.1007/s00417-019-04498-6
23. Figueiredo N, Sarraf D, Gunnemann F, et al. Longitudinal assessment of ellipsoid zone recovery using en face optical coherence tomography after retinal detachment repair. Am J Ophthalmol. 2022;236:212–220. doi:10.1016/j.ajo.2021.10.012
24. Wrzesińska D, Nowomiejska K, Nowakowska D, et al. Vertical and horizontal M-charts and microperimetry for assessment of the visual function in patients after vitrectomy with ILM peeling due to stage 4 macular hole. J Ophthalmol. 2019;2019:4975973. doi:10.1155/2019/4975973
25. Takeyama A, Imamura Y, Fujimoto T, et al. Predictors for metamorphopsia in eyes undergoing macular hole surgery. Sci Rep. 2023;13(1):810. doi:10.1038/s41598-023-28031-2
26. Park SH, Park KH, Kim HY, et al. Square grid deformation analysis of the macula and postoperative metamorphopsia after macular hole surgery. Retina. 2021;41(5):931–939. doi:10.1097/IAE.0000000000002955
27. Okamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T. Associations between metamorphopsia and foveal microstructure in patients with epiretinal membrane. Invest Ophthalmol Vis Sci. 2012;53(11):6770–6775. doi:10.1167/iovs.12-9683
28. Alkabes M, Fogagnolo P, Vujosevic S, Rossetti L, Casini G, Cillà SD D. Correlation between new OCT parameters and metamorphopsia in advanced stages of epiretinal membranes. Acta Ophthalmol. 2020;98(8):780–786. doi:10.1111/aos.14336
29. Yanagida K, Wakabayashi Y, Usui Y, et al. Ectopic inner foveal layer as a factor associated with metamorphopsia after vitrectomy for epiretinal membrane. Acta Ophthalmol. 2022;100(7):775–780. doi:10.1111/aos.15092
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Subfoveal Choroidal Thickness After Successful Retinal Detachment Repair with Persistent Subretinal Fluid at the Macula
Mansour AM, Parodi MB, Uwaydat SH, Lima LH, Charbaji S, Casella AM, López-Guajardo L, Belotto S, Wu L, Schwartz SG, Smiddy WE, Hassoun MM, Pérez-Salvador García E, Mansour HA, Elnahry AG, Hamam RN
Clinical Ophthalmology 2025, 19:1847-1854
Published Date: 11 June 2025