Back to Journals » Journal of Inflammation Research » Volume 17
Study on the Predictive Value of Renal Resistive Index Combined with β2-Microglobulin in Patients with Urosepsis Complicated with Acute Kidney Injury
Authors Li H , Zhou J, Wang Q, Zhu Y, Zi T, Qin X, Zhao Y, Jiang W, Li X, Wang X, Xu C, Chen X, Wu G
Received 24 August 2024
Accepted for publication 10 November 2024
Published 25 November 2024 Volume 2024:17 Pages 9583—9599
DOI https://doi.org/10.2147/JIR.S492858
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Adam Bachstetter
Haopeng Li,1,* Juan Zhou,2,* Qinghua Wang,1 Yaru Zhu,1 Tong Zi,1 Xin Qin,1 Yan Zhao,1 Wei Jiang,1 Xilei Li,1 Xin’an Wang,1 Chengdang Xu,1 Xi Chen,1 Gang Wu1
1Department of Urology, Tongji Hospital, School of Medicine, Tongji University, Shanghai, 200092, People’s Republic of China; 2Department of ICU, Tongji Hospital, School of Medicine, Tongji University, Shanghai, 200092, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xi Chen; Gang Wu, Email [email protected]; [email protected]
Purpose: This study aims to evaluate the predictive value of the renal resistive index (RRI) and β 2-microglobulin (β 2-MG) for acute kidney injury (AKI) in urosepsis patients and to develop a clinical prediction model for AKI risk.
Methods: Data from 108 urosepsis patients at Tongji Hospital were analyzed. Patients were divided into AKI (67 patients) and non-AKI (41 patients) groups based on KDIGO guidelines. Univariate analysis identified potential AKI risk factors, which were further assessed using multivariate logistic regression. A nomogram was constructed based on significant predictors, with internal validation via the bootstrap method. The model’s accuracy and clinical utility were evaluated using ROC curves and Decision Curve Analysis (DCA).
Results: Multivariate analysis identified RRI, β 2-MG, procalcitonin (PCT), and serum creatinine (Scr) as independent AKI risk factors. The combined predictive indicators yielded an AUC of 0.879, outperforming individual markers (P < 0.05). The prediction model achieved an AUC of 0.949, with high sensitivity (92.5%) and specificity (82.9%). Further analysis revealed that RRI, β 2-MG, PCT, and APACHE II scores were independent predictors of poor prognosis in urosepsis-related AKI, with combined RRI and β 2-MG predictions showing superior performance.
Conclusion: Elevated RRI, β 2-MG, PCT, and Scr levels are independent predictors of AKI in urosepsis. RRI, β 2-MG, PCT, and APACHE II scores also predict poor prognosis in urosepsis-related AKI. The nomogram combining these factors demonstrates high predictive accuracy and clinical applicability.
Keywords: renal resistive index, β 2-microglobulin, urosepsis, acute kidney injury
Introduction
Sepsis 3.0 defines sepsis as a syndrome characterized by life-threatening organ dysfunction caused by a dysregulated host response to infection.1 Previously, the diagnosis of urosepsis was primarily based on the presence of urinary tract infection (UTI) evidence combined with the fulfillment of at least two criteria of the systemic inflammatory response syndrome (SIRS).2 With the update of recent guidelines,3,4 the diagnostic criteria for urosepsis now require a Sequential Organ Failure Assessment (SOFA) score ≥ 2, in conjunction with a UTI. Urosepsis accounts for approximately 9–31% of sepsis cases and is caused by infections of the genitourinary system.5 Recent studies on septic shock indicate that the mortality rate of this condition may reach 28.3% to 41.1%. Among the various sources of infection leading to septic shock, urinary tract infections rank third, following pulmonary and abdominal infections.6 The incidence of septic shock is relatively higher in males, with Gram-negative bacteria being the primary infectious agents. In recent years, with the widespread application and rapid development of endourological techniques, the associated complications have increasingly become a focal point in the medical community.7 For certain specific populations, the case fatality rate of urosepsis is approximately 25%-60%, highlighting the significant clinical importance of improving the early diagnosis and management of urosepsis. Sepsis-associated acute kidney injury (S-AKI) is a common and life-threatening complication among hospitalized and critically ill patients. S-AKI not only significantly increases in-hospital mortality by 6–8 times compared to patients without S-AKI, but it also substantially elevates the risk of chronic kidney disease (CKD), increasing it by threefold.8 Of greater concern, approximately one-quarter of S-AKI patients may require renal replacement therapy (RRT) to sustain life.9 The current diagnosis of acute kidney injury primarily relies on serum creatinine levels and urine output.10 However, this method of diagnosis based on serum creatinine and urine output has inherent delays and is influenced by multiple factors.11 For instance, individuals with normal renal function may exhibit elevated serum creatinine (SCR) levels due to factors such as high muscle mass or the use of specific medications (eg, trimethoprim and cimetidine).12 However, serum creatinine levels may show only minimal fluctuations within the first 72 hours of onset, potentially delaying diagnosis. Urine output (UO) can also be unreliable, as it is influenced by diuretic use and fluid resuscitation. Notably, only persistent oliguria serves as a reliable indicator of acute kidney injury (AKI), limiting the utility of UO for timely diagnosis.13 Furthermore, the changes in SCR and UO lag significantly behind the critical structural alterations occurring in the kidneys during AKI. By the time these markers exhibit substantial deviations, renal function is often already severely compromised, reducing the likelihood of timely intervention and potentially missing the optimal window for treatment.14,15 Studies have shown that urinary sediment analysis can aid in the diagnosis of AKI severity.16 Microscopic examination of urine in S-AKI patients reveals higher scores, demonstrating higher specificity and aiding in the prognosis of AKI.
The renal resistive index (RRI) reflects intrarenal blood flow resistance and is obtained by Doppler ultrasound, which measures the peak systolic velocity (PSV) and end diastolic velocity (EDV) within the arcuate or interlobar arteries. The RRI is then calculated using the formula RRI = (PSV - EDV) / PSV. An RRI of less than 0.70 is generally considered normal, although the normal reference range of RRI may be age-related.17 Currently, it is believed that the normal reference range of the mean RRI in healthy individuals is (0.58 ± 0.05) to (0.64 ± 0.04).18 The Renal Resistive Index (RRI) has been extensively used for assessing renal perfusion and can predict Acute Kidney Injury (AKI) as well as the recovery from AKI in the ICU. In cases of sepsis and acute kidney injury, systemic inflammatory responses and inadequate effective circulating blood volume result in the kidneys being more sensitive to vasoconstrictive agents, leading to more pronounced renal vasoconstriction compared to peripheral vessels. Consequently, changes in RRI can reflect peripheral and renal microcirculation status at an early stage. Studies have shown that RRI may have better predictive value for various durations of AKI compared to cystatin C, and when combined with creatinine and SOFA scores, RRI’s value in predicting different stages of AKI increases.18,19 In septic shock patients, RRI within the first 24 hours aids in predicting sepsis-induced AKI, especially when combined with central venous pressure (CVP) measurements.20 Furthermore, elevated RRI (RRI value >0.795) has been found to diagnose persistent AKI more effectively than urinary biomarkers, indicating that RRI can serve as a marker for renal function recovery in critically ill patients.21 Recent meta-analyses confirm the diagnostic performance of RRI in predicting the short-term reversibility of AKI, although significant heterogeneity exists among the included studies.22 In a study on fluid resuscitation requiring vasoactive drugs in septic shock patients, RRI was found to be indicative of the recovery of mean arterial pressure and helpful in hemodynamic management.23
In the clinical context of sepsis, acute kidney injury is a common complication, and timely prediction and proactive intervention are crucial. Researchers are striving to identify biomarkers for AKI to guide early sepsis treatment. Doppler ultrasound, with its convenience, speed, and repeatability, has been widely used in clinical settings, and its close association with AKI is well-recognized. However, early prediction of S-AKI with a single biomarker remains challenging. Traditional markers like creatinine, urine output, C-reactive protein, and procalcitonin have their respective limitations. Notably, β2-microglobulin (β2-MG) has shown significant advantages in diagnosing AKI. β2-MG is a small protein present on the cell membranes of all nucleated cells, including lymphocytes.24 Under normal physiological conditions, its production and release are stable, approximately 150 to 200 mg daily. In pathological states like inflammation or allergic reactions, β2-MG release increases. Normally functioning kidneys filter β2-MG through glomeruli, and about 99% is reabsorbed and metabolized in renal tubules, resulting in minimal urinary excretion.25 Since β2-MG metabolism relies heavily on renal function, its process is impaired when kidney function declines. A 50% decrease in glomerular filtration rate (GFR) doubles the serum β2-MG level, whereas serum creatinine only increases when GFR falls to 70% of normal. Thus, elevated serum β2-MG may indicate glomerular filtration impairment or increased filtration load earlier and more prominently than serum creatinine.26,27
We propose investigating the predictive value of combining RRI with β2-MG, an emergency renal injury biomarker, for acute kidney injury associated with urosepsis. This approach aims to improve the diagnosis and prognosis assessment of urosepsis-related acute kidney injury, providing a theoretical basis for clinical treatment.
Methods
Clinical Data
This study is a prospective observational study. It includes patients with urosepsis who were consecutively admitted to the Department of Urology and the Intensive Care Unit (ICU) at Tongji Hospital, affiliated with Tongji University, between January 1, 2022, and December 30, 2023. The data were obtained from the hospital’s Case 360 Management System.
Inclusion Criteria and Exclusion Criteria
Inclusion Criteria
(1) The patient was hospitalized for more than 24 hours; (2) The patient met the diagnostic criteria for urosepsis; (3) Complete clinical data were provided; (4) The patient or their legal representative signed an informed consent form.
Exclusion Criteria
(1) Patients with chronic kidney injury; (2) Patients with specific cardiac diseases affecting hemodynamics; (3) Patients with long-term diuretic use; (4) Patients with a recent history of AKI; (5) Patients who have recently used contrast agents; (6) Patients with abdominal compartment syndrome; (7) Patients with immune-related diseases; (8) Patients undergoing short-term or long-term hemodialysis; (9) Patients who have undergone kidney transplantation; (10) Pregnant female patients; (11) Patients under 18 years of age.
Research Methods
All the Enrolled Patients Were Treated According to Relevant Diagnosis and Treatment Standards
The basic information of all patients, such as gender, age, and other relevant clinical data, including vital signs and comorbidities, were recorded. Blood parameters measured within 24 hours of admission included hemoglobin, white blood cell count, C-reactive protein, neutrophil percentage, procalcitonin (PCT), blood lactate, bilirubin, creatinine, blood urea nitrogen, blood glucose, potassium, prothrombin time (PT), activated partial thromboplastin time (APTT), interleukin-6, as well as leukocytes, erythrocytes, nitrites in urine, and urine culture results. Upon admission, detailed records were made regarding whether the patient received mechanical ventilation, renal replacement therapy, or vasopressor treatment. Additionally, the patient’s β2-MG level within 24 hours, urine output during the first 24 hours, APACHE II score, and SOFA score were also documented.
Measurement of Renal Artery Resistive Index (RRI)
Within the first 6 hours of patient admission, an intensivist trained in bedside ultrasound performed RRI measurements using an ultrasound device equipped with a convex array probe (frequency 2 to 5 MHz). To maintain consistency, the right kidney was selected for all measurements. The procedure began by capturing a two-dimensional ultrasound image of the kidney, clearly displaying the longitudinal section. Advanced color Doppler technology was then used to accurately identify the intrarenal vascular network, and the interlobar or arcuate arteries were selected for RRI measurement (Figure 1). Using pulsed Doppler mode, the peak systolic velocity (PSV) and end diastolic velocity (EDV) were measured within a sample volume of 2–5 mm, and the RRI was calculated. Each measurement was performed at least three times, with the average value taken as the final result. The RRI was calculated using the formula: Renal Artery Resistive Index = (PSV - EDV) / PSV. If any measurement errors occurred, the process was repeated and recalculated.
Statistical Methods
Statistical analyses were conducted using R Studio (integrated with R version 3.6.3). The mean and standard deviation were used to describe the central tendency and dispersion of continuous variables that followed or approximately followed a normal distribution. To assess differences between groups, independent samples t-tests were performed. For data that did not conform to a normal distribution, the median and interquartile range were used to describe the distribution characteristics, and non-parametric tests were applied to analyze differences between groups. Continuous variables that showed statistical significance in univariate analysis were further analyzed using ROC curve analysis. After determining cut-off values, these variables were included in the regression equation, with appropriate reference levels selected for categorical variables. The entry method for variables was the enter method, using the odds ratio (OR) as the risk assessment parameter, and a multivariate binary logistic regression model was established to identify independent predictors. A nomogram was developed for the predictive model, with internal validation conducted through Bootstrap resampling, repeated 1000 times. The predictive ability of the model was evaluated by plotting ROC curves and calculating the area under the curve (AUC). The calibration curve, comparing predicted and actual values, was used to assess the predictive model for AKI risk in urosepsis patients. Decision curve analysis (DCA) was employed to evaluate the clinical value of the nomogram by analyzing net benefits across different threshold probabilities. Survival analysis was performed using Prism 9 software.
Results
Patient Enrollment and Grouping
A total of 121 urosepsis patients were initially screened for this study. Of these, 1 patient was under 18 years of age, 10 had a hospital stay of less than 24 hours, 2 had specific cardiac diseases, and 1 had an autoimmune disease. Ultimately, 108 urosepsis patients were included in the study. Among the enrolled patients, 67 (60.8%) developed AKI, while 41 (39.2%) did not. The AKI group was further divided into a deceased group and a survival group based on 28-day outcomes (Figure 2).
 |
Figure 2 Flow chart of patient selection. |
Baseline Characteristics of No-AKI Group and AKI Group
Statistical analysis revealed no significant differences between the two groups (P > 0.05) in the following aspects: age, gender distribution, comorbidities (including hypertension, cancer, diabetes, cerebral infarction, etc)., sources of infection (such as urinary stones, benign prostatic hyperplasia, renal abscess, urinary retention, scrotal gangrene, ureterostomy, etc)., length of hospital stay, use of vasopressors, systolic and diastolic blood pressure, mean arterial pressure levels, and the proportions of patients receiving mechanical ventilation and CRRT. Additionally, there was no statistically significant difference in urine output within the first 24 hours between the two groups.
However, significant differences were observed between the two groups in serum creatinine, RRI, PCT, β2-MG, APACHE II, and SOFA scores, all of which were statistically significant (P < 0.05). Specifically, the median serum creatinine value in the AKI group (132.00) was significantly higher than in the non-AKI group (74.70); the mean RRI in the AKI group (0.73) was significantly higher than in the non-AKI group (0.65); the median β2-MG value in the AKI group (6.50) was significantly higher than in the non-AKI group (2.10); the median PCT value in the AKI group (29.68) was significantly higher than in the non-AKI group (1.20); the mean APACHE II score in the AKI group (19.90) was significantly higher than in the non-AKI group (15.24); and the mean SOFA score in the AKI group (9.00) was significantly higher than in the non-AKI group (6.00). Additionally, a significant difference was observed in the 28-day prognosis between the two groups (Table 1).
 |
Table 1 Baseline Characteristics of No-AKI Group and AKI Group |
Multivariate Logistic Regression Analysis of AKI Patients
To identify risk factors for the development of acute kidney injury (AKI) in patients with urosepsis, we conducted a multivariate logistic regression analysis. In this analysis, the occurrence of AKI was set as the dependent variable, and the variables found to be significant in the prior univariate analysis were selected as independent variables. These variables included RRI, β2-MG, SOFA, APACHE II, PCT, and serum creatinine levels. The multivariate logistic regression analysis revealed that RRI, β2-MG, PCT, and serum creatinine levels were independent predictors of AKI in urosepsis patients, with all factors showing P-values less than 0.05, indicating significant statistical relevance (Table 2).
 |
Table 2 Multivariate Logistic Regression Analysis of AKI Patients |
The Predictive Value of RRI, β2-MG, PCT, SCr, and the Combined Use of RRI and β2-MG for AKI Occurrence in Urosepsis
To evaluate the predictive ability of RRI, β2-MG, PCT, serum creatinine, and the combined use of RRI and β2-MG in determining the occurrence of AKI in patients with urosepsis, we plotted ROC curves. A larger area under the ROC curve (AUC) indicates a stronger predictive capability of the variable in forecasting poor AKI outcomes in urosepsis patients. The AUC values for RRI, β2-MG, PCT, and serum creatinine in predicting AKI were 0.771, 0.789, 0.745, and 0.770, respectively, with all P-values < 0.05. When RRI and β2-MG were combined for AKI prediction, the AUC increased to 0.879 (P < 0.05), indicating that the combined use of RRI and β2-MG offers a higher predictive value for AKI in urosepsis patients (Table 3 and Figure 3).
 |
Table 3 The Predictive Value of RRI, β2-MG, PCT, SCr, and the Combined Use of RRI and β2-MG for AKI Occurrence in Urosepsis |
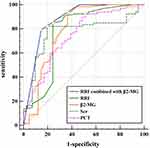 |
Figure 3 ROC curve of RRI, β 2-MG, PCT, Scr, and RRI combined with β 2-MG for the AKI development in urosepsis. |
Development of a Clinical Prediction Model for AKI in Urosepsis
Based on the results of multivariate logistic regression analysis, RRI, β2-MG, PCT, and serum creatinine were identified as independent predictors of AKI in urosepsis patients. These variables were incorporated into a clinical prediction model for AKI in urosepsis, and a nomogram was generated. The model’s goodness-of-fit was confirmed by the Hosmer-Lemeshow test (χ² = 5.388, P = 0.495 > 0.05), indicating a good fit (Figure 4).
 |
Figure 4 Nomogram of the clinical prediction model for the development of AKI in urosepsis. |
In the provided nomogram, the first row lists the reference values for each variable’s score. For each patient, the corresponding score (Points) is assigned based on the specific values of these variables. The total score (Total Points) is then calculated by summing these individual scores. In the penultimate row of the chart, a corresponding mapped value for the total score can be found. Finally, by matching this mapped value with the probability in the Risk row, the likelihood of the patient developing AKI based on their variables can be determined.
Validation of the Clinical Prediction Model for AKI in Urosepsis
ROC curve analysis (Figure 5) demonstrated that the nomogram model had an AUC of 0.949, with a 95% confidence interval (CI) of 0.867–1.000. At the optimal cutoff value of 0.148, the sensitivity was 92.5% and the specificity was 82.9%, indicating that the model possesses strong predictive ability. The model’s C-index was 0.949, with a standard deviation (SD) of 0.042, a Z-score of 21.150, and a P-value less than 0.05, confirming the statistical significance of the concordance test and the model’s high predictive value.
 |
Figure 5 Area under the ROC curve of the clinical prediction model for AKI in urosepsis. |
Calibration curve analysis (Figure 6) revealed that internal validation of the model’s predictive capability was conducted using the Bootstrap resampling technique with 1000 iterations. The results showed that the actual curve closely aligned with the corrected curve, demonstrating high consistency. Additionally, the fit of the actual model results closely matched the expected model results and the bias-corrected outcomes, with the data points uniformly distributed near the diagonal line. This indicates the model’s high robustness and reliability. The nomogram model shows good agreement between the predicted probability and the actual probability of AKI occurrence in urosepsis patients.
 |
Figure 6 Calibration curve of clinical prediction model for AKI occurrence of urosepsis. |
Evaluation of the Clinical Decision Curve for Predicting AKI in Urosepsis Patients
To further assess the predictive risk model for AKI in urosepsis patients, we constructed a Decision Curve Analysis (DCA) aimed at providing clinicians with a more precise and practical decision-support tool (Figure 7). The DCA results indicate that within the threshold probability range of 0.02 to 0.80, utilizing this AKI risk assessment tool significantly enhances net benefit compared to intervening in all patients or not intervening at all, thereby optimizing clinical decision-making. The predictive risk model demonstrates considerable clinical utility in assessing AKI occurrence in urosepsis patients.
 |
Figure 7 Clinical decision curve (DCA curve for AKI). |
28-Day Survival Analysis of the AKI and No-AKI Groups
This study further analyzed the 28-day survival outcomes of patients with urosepsis. (Figure 8) Among the 67 patients in the AKI group, 27 patients died, resulting in a mortality rate of 40.3%. In contrast, in the non-AKI group of 41 patients, 7 patients died, yielding a mortality rate of 17.1%. The difference between the two groups was statistically significant (P = 0.02). Kaplan-Meier survival curves were constructed for both groups.
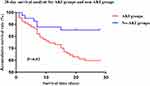 |
Figure 8 28-day survival analysis of the AKI and no-AKI groups. |
Comparison of Relevant Indicators Between Different Prognosis Groups in Urosepsis Patients with AKI
Significant differences were observed between the two prognosis groups regarding RRI, PCT, β2-MG, APACHE II score, SOFA score, lactate, IL-6, and PT levels (P < 0.05) (Table 4). The median RRI in the deceased group (0.76) was notably higher than that in the survival group (0.72). The median β2-MG level in the survival group (5.40) was significantly lower than that in the deceased group (9.50). The median SOFA score in the survival group (8.00) was also significantly lower than that in the deceased group (9.00). Additionally, the survival group had a lower median APACHE II score (19.00) compared to the deceased group (21.00). Lactate levels were lower in the survival group (median 2.10) compared to the deceased group (median 3.10). The median PT in the deceased group (14.8) was higher than that in the survival group (13.20). Similarly, the median PCT level in the deceased group (31.80) exceeded that in the survival group (6.93), and the median IL-6 level in the deceased group (1009.00) was substantially higher than in the survival group (251.00).
 |
Table 4 Comparison of Correlation Indicators Between Different Outcomes of AKI in Urosepsis |
Multivariate Logistic Regression Analysis of Prognostic Factors Affecting AKI Outcomes in Urosepsis Patients
To further explore the risk factors influencing the prognosis of urosepsis patients who develop AKI, we conducted a multivariate logistic regression analysis (Table 5). In this analysis, patient mortality, an essential indicator of prognosis, was used as the dependent variable. The independent variables were selected from those that had shown statistical significance in the univariate analysis, including RRI, PCT, β2-MG, APACHE II score, SOFA score, lactate levels, IL-6, and PT. These variables have been identified as closely related to the occurrence and prognosis of AKI in urosepsis patients. The multivariate logistic regression analysis aimed to understand the relationships between these independent variables and the dependent variable, determining which factors significantly impact patient prognosis. The results indicated that RRI, β2-MG, PCT, and APACHE II score are independent predictors of AKI outcomes in urosepsis patients, with all P-values being less than 0.05.
 |
Table 5 Multivariate Logistic Regression Analysis Affecting the Outcome of AKI in Urosepsis |
Predictive Value of RRI, β2-MG, PCT, APACHE II Score, and Combined RRI and β2-MG for Prognosis in Urosepsis-Associated AKI
To evaluate the predictive value of RRI, β2-MG, PCT, APACHE II score, and the combination of RRI and β2-MG for adverse outcomes in urosepsis patients with AKI, ROC curves were plotted with these five variables as predictors and adverse prognosis post-AKI as the outcome variable. The areas under the ROC curves (AUC) for each variable were compared to assess their predictive performance. The AUC values for RRI, β2-MG, APACHE II score, and PCT alone in predicting AKI were 0.802, 0.782, 0.656, and 0.671, respectively, all with P-values less than 0.05. When combined, RRI and β2-MG yielded an AUC of 0.811 for predicting adverse outcomes in AKI, with a P-value less than 0.05, indicating that the combination of RRI and β2-MG has a higher predictive value for adverse prognosis in urosepsis-associated AKI (Table 6 and Figure 9).
 |
Table 6 Predictive Value of RRI, β 2-MG, PCT, APACHE II Score, and RRI Combined with β 2-MG for AKI Outcome in Urosepsis |
 |
Figure 9 ROC curve analysis of RRI, β2-MG, PCT, APACHE II score, and RRI combined with β2-MG to affect the outcome of AKI in urosepsis. |
Discussion
Urosepsis is a life-threatening condition characterized by organ dysfunction resulting from a dysregulated host response to an infection originating from the urinary tract or male genital organs.28 It constitutes 9% to 31% of all sepsis cases, with many patients presenting with additional high-risk factors such as urinary stones, obstruction, or history of endoscopic procedures.29 The most common pathogen causing urosepsis is Escherichia coli, though other pathogens such as Proteus species, Enterobacter species, and Gram-positive bacteria are also prevalent. Common conditions associated with urosepsis include urinary stones and structural or functional abnormalities of the urogenital tract, such as benign prostatic hyperplasia and neurogenic bladder. Prolonged indwelling catheters are also significant risk factors for infection, which leads to a higher incidence and mortality.30 Urosepsis is more severe than simple urinary tract infections, necessitating early diagnosis and prompt treatment to prevent progression to septic shock and multiple organ dysfunction.31 Sepsis and AKI have a bidirectional relationship, with sepsis being a leading cause of AKI in intensive care units (ICU). AKI in sepsis is associated with poorer outcomes, longer hospital stays, and higher mortality rates.32 Increasing evidence suggests that sepsis is a key precipitating factor for AKI, with a higher risk of infection or sepsis following AKI. Some researchers propose that AKI should be considered an early sign of sepsis.33
Currently, the clinical diagnosis of AKI largely relies on urine output and serum creatinine levels, which have certain limitations and can lead to delays in diagnosis. Early identification of sepsis-associated AKI (S-AKI) remains challenging for clinicians, highlighting the need for early identification systems to improve early diagnosis rates and predict adverse outcomes. This study primarily investigates the predictive value of the renal resistive index (RRI) combined with β2-microglobulin (β2-MG) for emergency renal injury associated with urosepsis. Additionally, it constructs and validates a clinical prediction model using RRI and β2-MG as key risk factors.
The study results indicate that RRI, β2-MG, PCT, and serum creatinine levels are independent risk factors for AKI in urosepsis patients. Furthermore, RRI, β2-MG, PCT, and APACHE II scores are identified as independent risk factors for poor prognosis following AKI in urosepsis. Analysis reveals that the combined use of RRI and β2-MG exhibits superior predictive capability for AKI compared to individual indicators. The combination also shows a higher predictive value for adverse outcomes following AKI. Based on these findings, a clinical prediction model for AKI in urosepsis patients was developed. This model demonstrates high discrimination and calibration, indicating its substantial clinical applicability and potential for use in practice.
In this study, 108 patients were included and categorized into AKI and non-AKI groups. Univariate analysis of baseline data and test results showed that over 60% of patients in both groups had urinary stones, consistent with previous literature indicating that urinary obstruction is a primary cause of urosepsis.34 Due to anatomical features of the urinary tract, stones can cause obstruction and hydronephrosis, creating conditions conducive to bacterial biofilm formation and subsequent infection. Additionally, the use of irrigation fluids during stone-related procedures (eg, ureteroscopy and percutaneous nephrolithotomy) can increase renal pelvic pressure and exacerbate infection, leading to sepsis.35 In this study, the rates of positive urine cultures were 52.2% in the AKI group and 36.6% in the non-AKI group. The relatively low positivity rates may be due to the choice of culture media and early use of antibiotics. Therefore, negative cultures do not completely rule out urinary infections, and positive cultures alone cannot predict poor prognosis.36
Among the included urosepsis patients, high SOFA and APACHE II scores were observed, consistent with the diagnosis of sepsis. Relevant studies37,38 also indicate that SOFA and APACHE II scores are valuable for diagnosing and predicting sepsis outcomes. Multivariate logistic regression analysis identified APACHE II score as an independent predictor of poor prognosis in urosepsis with AKI. The APACHE II score, developed by Knaus et al, ranges from 0 to 71 and includes age, comorbid conditions, and acute physiological parameters. It has demonstrated good calibration and discrimination across various disease processes and remains widely used in ICU prognosis assessment.39
While there is substantial research on the predictive value of sepsis and AKI, studies specifically on urosepsis-associated AKI are less common, and few include ultrasonographic indicators. Bedside ultrasound technology is widely used for assessing renal function in hospitalized patients due to its non-invasive, safe, convenient, and repeatable nature. This study innovatively incorporates RRI into the predictive analysis of urosepsis-related AKI and constructs a prediction model. The findings indicate significant differences in RRI between AKI and non-AKI groups, consistent with numerous clinical studies.40–42 Notably, a study on 107 patients with septic shock also found that survivors had significantly lower RRI values than non-survivors, highlighting RRI’s high predictive value for acute kidney injury in sepsis. This finding corroborates the importance and accuracy of RRI in predicting AKI in urosepsis. Routine circulatory monitoring focuses primarily on systemic circulation, while ultrasound-measured RRI can assess renal microcirculation changes. When effective circulatory blood volume is insufficient, peripheral vessels constrict compensatorily, and renal vessels, having a higher density of vasoconstrictor receptors, show more pronounced constriction, leading to increased renal vascular resistance. Thus, changes in RRI reflect peripheral and renal perfusion status, with elevated RRI often indicating inadequate renal perfusion.43 During urosepsis with AKI, inflammatory factors are released, causing hemodynamic changes and altering renal microcirculation, resulting in increased vascular pressure and elevated RRI levels. Renal vascular constriction is considered an early sign of AKI, with RRI reflecting not only the resistance of the renal artery trunk but also changes in the flow curves of arcuate or interlobar arteries, including the relationship between systolic peak and end-diastolic flow velocity.44 Elevated renal vascular resistance is closely related to hemodynamic parameters such as systolic and diastolic blood pressure, pulse pressure, and pulse wave velocity, reflecting renal artery stiffness and serving as a key method for monitoring renal vascular conditions.45
β2-MG is a small protein in the blood that is freely filtered by the glomeruli, with only a small amount excreted in the urine. Under normal conditions, β2-MG levels in the blood and urine remain relatively stable Recent studies46 have shown that increased blood β2-MG is associated with decreased glomerular filtration rate (GFR). Therefore, β2-MG is a good marker for reflecting glomerular filtration function and is widely used in diagnosing AKI in diseases such as diabetes and primary hypertension. When GFR drops to 50% of normal, blood β2-MG levels increase by a factor of two, whereas serum creatinine levels only rise when GFR decreases to 70% of normal. β2-MG levels increase earlier and more significantly than creatinine and are less affected by dietary factors. Thus, measuring blood β2-MG provides a better representation of glomerular filtration function. This study found that β2-MG has good predictive capability for AKI in urosepsis, aligning with the mechanisms of AKI. The combination of RRI and β2-MG captures both macro-level renal perfusion reduction and micro-level pathophysiological changes during AKI, explaining the higher predictive value of their combined use. Although serum creatinine is the gold standard for diagnosing AKI, it is not an ideal biomarker due to its sensitivity to non-renal factors such as age, sex, muscle mass, fluid balance, and medications affecting tubular secretion. Additionally, creatinine levels rise with a delay, only increasing after significant glomerular damage.47 The combined diagnostic prediction using the model in this study enhances the clinical value of serum creatinine and addresses its limitations to some extent. PCT is a recognized biomarker for diagnosing infections and guiding antibiotic treatment, with rapid increases in levels within the first 3–4 hours of infection or inflammation, peaking in 6–12 hours, and decreasing to normal levels within 5 days.48 It has been proposed for predicting AKI in clinical settings,49 but its predictive capability may be weakened due to the greater impact of infection on PCT levels compared to AKI. By comparing the diagnostic limitations of creatinine, PCT, and urine output, the study highlights the diagnostic value of β2-MG for urosepsis with AKI, and the combined use of RRI and β2-MG offers higher predictive value for diagnosis and prognosis, reflecting organ and systemic changes during disease onset. This provides a basis for better clinical guidance and reduced mortality rates in the future. To effectively apply our prediction model in clinical practice, it is essential to integrate it into electronic health record (EHR) systems for real-time risk assessment. Automated alerts based on key predictors, such as RRI and β2-microglobulin, could prompt early intervention. Training healthcare staff on how to interpret the nomogram and incorporate it into decision-making processes is equally important. Given that this study is based on single-center data, external validation through multi-center studies will be crucial to ensure the model’s reliability and generalizability. Collaboration across institutions can further enhance the model by promoting data sharing and continuous improvement. Additionally, monitoring the model’s performance and refining it with updated clinical data will ensure long-term effectiveness. This prediction model holds significant potential for early AKI detection, providing clinicians with actionable insights to improve patient outcomes, especially in cases of urosepsis.
This study has certain limitations: 1) It is a single-center study with a limited sample size, which may introduce selection bias. Subsequent research should involve multi-center collaborations and larger sample sizes to further explore the validity and generalizability of the results. 2) Although thorough internal validation was performed, additional external validation with a larger sample size is needed to enhance the evidence base for the predictive model.
Conclusion
In conclusion, this study identifies elevated levels of RRI, β2-MG, PCT, and Scr as independent predictors for the onset of AKI in urosepsis patients. Furthermore, RRI, β2-MG, PCT, and APACHE II scores are demonstrated to be independent indicators of poor prognosis in patients with urosepsis-induced AKI. Notably, the combined predictive value of RRI and β2-MG surpasses that of individual predictors. The nomogram incorporating RRI, β2-MG, PCT, and Scr exhibits high predictive value, with strong discrimination and calibration, highlighting its potential clinical applicability and efficiency in predicting AKI in urosepsis patients.
Ethics Approval
This study was conducted in compliance with the Declaration of Helsinki. This study fully obtained the informed consent from patients or family members, and signed the informed consent form, and passed the ethical review of Shanghai Tongji Hospital (2021-KYSB-143).
Acknowledgments
We express our gratitude to all the staff contributing to this study.
Funding
This research was supported by A nucleotide targeting lncRNA ZNF518A for AR-V7-mediated castration-resistant prostate cancer (ZLZH2202), A Study on the Role and Mechanism of lncRNA SNHG3 in Regulating Glycolysis in Castration-Resistant Prostate Cancer (GJPY2208), Outstanding Discipline Reserve Talent Program of Tongji Hospital, Affiliated with Tongji University (HBRC1707), and “Rising Medical Stars” Young Medical Talent Development Support Program (2019-1Y).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
2. Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM consensus conference committee. Chest. 1992;101(6):1644–1655. doi:10.1378/chest.101.6.1644
3. Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–1247. doi:10.1007/s00134-021-06506-y
4. Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–377. doi:10.1007/s00134-017-4683-6
5. Wagenlehner FM, Tandogdu Z, Bjerklund Johansen TE. An update on classification and management of urosepsis. Curr Opin Urol. 2017;27(2):133–137. doi:10.1097/MOU.0000000000000364
6. Levy MM, Artigas A, Phillips GS, et al. Outcomes of the surviving sepsis campaign in intensive care units in the USA and Europe: a prospective cohort study. Lancet Infect Dis. 2012;12(12):919–924. doi:10.1016/S1473-3099(12)70239-6
7. Johansen TEB, Cai T. Facing urosepsis- The most deadly of all urological diseases. Scand J Urol. 2022;56(5–6):421–422. doi:10.1080/21681805.2022.2137230
8. Coca SG, Yusuf B, Shlipak MG, et al. Long-term risk of mortality and other adverse outcomes after acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis. 2009;53(6):961–973. doi:10.1053/j.ajkd.2008.11.034
9. Godin M, Murray P, Mehta RL. Clinical approach to the patient with AKI and sepsis. Semin Nephrol. 2015;35(1):12–22. doi:10.1016/j.semnephrol.2015.01.003
10. KDIGO. 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021;100(4s):S1–s276. doi:10.1016/j.kint.2021.05.021
11. Zarbock A, Nadim MK, Pickkers P, et al. Sepsis-associated acute kidney injury: consensus report of the 28th Acute Disease Quality Initiative workgroup. Nat Rev Nephrol. 2023;19(6):401–417. doi:10.1038/s41581-023-00683-3
12. Burwick RM, Moyle K, Java A, Gupta M. Differentiating hemolysis, elevated liver enzymes, and low platelet count syndrome and atypical hemolytic uremic syndrome in the postpartum period. Hypertension. 2021;78(3):760–768. doi:10.1161/HYPERTENSIONAHA.121.17311
13. Bianchi NA, Stavart LL, Altarelli M, Kelevina T, Faouzi M, Schneider AG. Association of oliguria with acute kidney injury diagnosis, severity assessment, and mortality among patients with critical illness. JAMA Network Open. 2021;4(11):e2133094. doi:10.1001/jamanetworkopen.2021.33094
14. Vanmassenhove J, Steen J, Vansteelandt S, et al. The importance of the urinary output criterion for the detection and prognostic meaning of AKI. Sci Rep. 2021;11(1):11089. doi:10.1038/s41598-021-90646-0
15. Xiao Z, Huang Q, Yang Y, et al. Emerging early diagnostic methods for acute kidney injury. Theranostics. 2022;12(6):2963–2986. doi:10.7150/thno.71064
16. Bagshaw SM, Haase M, Haase-Fielitz A, Bennett M, Devarajan P, Bellomo R. A prospective evaluation of urine microscopy in septic and non-septic acute kidney injury. Nephrol Dial Transplant. 2012;27(2):582–588. doi:10.1093/ndt/gfr331
17. Renberg M, Kilhamn N, Lund K, et al. Feasibility of renal resistive index measurements performed by an intermediate and novice sonographer in a volunteer population. Ultrasound J. 2020;12(1):28. doi:10.1186/s13089-020-00175-6
18. Choi YH, Cheon J-E, Kim WS, Kim I-O. Ultrasonography of hydronephrosis in the newborn: a practical review. Ultrasonography. 2016;35(3):198–211. doi:10.14366/usg.15073
19. Schnell D, Deruddre S, Harrois A, et al. Renal resistive index better predicts the occurrence of acute kidney injury than cystatin C. Shock. 2012;38(6):592–597. doi:10.1097/SHK.0b013e318271a39c
20. Song J, Wu W, He Y, et al. Value of the combination of renal resistance index and central venous pressure in the early prediction of sepsis-induced acute kidney injury. J Crit Care. 2018;45:204–208. doi:10.1016/j.jcrc.2018.03.016
21. Darmon M, Schortgen F, Vargas F, et al. Diagnostic accuracy of Doppler renal resistive index for reversibility of acute kidney injury in critically ill patients. Intensive Care Med. 2011;37(1):68–76. doi:10.1007/s00134-010-2050-y
22. Ninet S, Schnell D, Dewitte A, et al. Doppler-based renal resistive index for prediction of renal dysfunction reversibility: a systematic review and meta-analysis. J Crit Care. 2015;30(3):629–635. doi:10.1016/j.jcrc.2015.02.008
23. Deruddre S, Cheisson G, Mazoit JX, et al. Renal arterial resistance in septic shock: effects of increasing mean arterial pressure with norepinephrine on the renal resistive index assessed with Doppler ultrasonography. Intensive Care Med. 2007;33(9):1557–1562. doi:10.1007/s00134-007-0665-4
24. Zhang L, Sun J, Zhang M, et al. The significance of combined detection of CysC, urinary mAlb and β(2)-MG in diagnosis of the early renal injury in pregnancy-induced hypertension syndrome. Saudi J Biol Sci. 2019;26(8):1982–1985. doi:10.1016/j.sjbs.2019.07.013
25. Petrica L, Petrica M, Vlad A, et al. Nephro- and neuroprotective effects of rosiglitazone versus glimepiride in normoalbuminuric patients with type 2 diabetes mellitus: a randomized controlled trial. Wien Klin Wochenschr. 2009;121(23–24):765–775. doi:10.1007/s00508-009-1279-3
26. Chen H, Li H. Clinical implication of cystatin C and β2-microglobulin in early detection of diabetic nephropathy. Clin Lab. 2017;63(2):241–247. doi:10.7754/Clin.Lab.2016.160719
27. Nozue T, Michishita I, Mizuguchi I. Predictive value of serum cystatin C, β2-microglobulin, and urinary liver-type fatty acid-binding protein on the development of contrast-induced nephropathy. Cardiovasc Interv Ther. 2010;25(2):85–90. doi:10.1007/s12928-010-0014-3
28. Shimoni Z, Salah M, Kasem A, et al. Bacterial resistance to cephalosporin treatment in elderly stable patients hospitalized with a urinary tract infection. Am J Med Sci. 2020;360(3):243–247. doi:10.1016/j.amjms.2020.05.008
29. Hsu S-L, Fan C-K, Liu H-Y. Obstructive hydronephrosis with secondary urosepsis. Clin Case Rep. 2022;10(4):e05689. doi:10.1002/ccr3.5689
30. Kaur R, Kaur R. Symptoms, risk factors, diagnosis and treatment of urinary tract infections. Postgrad Med J. 2021;97(1154):803–812. doi:10.1136/postgradmedj-2020-139090
31. Liang X, Zou W. Research advance in urosepsis]. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2019;44(4):455–460. doi:10.11817/j.issn.1672-7347.2019.04.018
32. Kuwabara S, Goggins E, Okusa MD. The pathophysiology of sepsis-associated AKI. Clin J Am Soc Nephrol. 2022;17(7):1050–1069. doi:10.2215/CJN.00850122
33. Lai T-S, Wang C-Y, Pan S-C. Risk of developing severe sepsis after acute kidney injury: a population-based cohort study. Crit Care. 2013;17(5):R231. doi:10.1186/cc13054
34. Shaikh N, Momin U, Atef Shible A, et al. Community acquired urosepsis: a surgical intensive care experience. Qatar Med J. 2020;2020(1):8. doi:10.5339/qmj.2020.8
35. Bhojani N, Miller LE, Bhattacharyya S, et al. Risk factors for urosepsis after ureteroscopy for stone disease: a systematic review with meta-analysis. J Endourol. 2021;35(7):991–1000. doi:10.1089/end.2020.1133
36. Gu J, Liu J, Hong Y, et al. Nomogram for predicting risk factor of urosepsis in patients with diabetes after percutaneous nephrolithotomy. BMC Anesthesiol. 2022;22(1):87. doi:10.1186/s12871-022-01629-1
37. Huang Y, Jiang S, Li W, et al. Establishment and effectiveness evaluation of a scoring system-RAAS (RDW, AGE, APACHE II, SOFA) for sepsis by a retrospective analysis. J Inflamm Res. 2022;15:465–474. doi:10.2147/JIR.S348490
38. Tekin B, Kiliç J, Taşkin G, et al. The comparison of scoring systems: SOFA, APACHE-II, LODS, MODS, and SAPS-II in critically ill elderly sepsis patients. J Infect Dev Ctries. 2024;18(1):122–130. doi:10.3855/jidc.18526
39. Patel P, Gupta S, Patel H, et al. Assessment of APACHE II score to predict ICU outcomes of patients with AKI: a single-center experience from Haryana, North India. Indian J Crit Care Med. 2022;26(3):276–281. doi:10.5005/jp-journals-10071-24142
40. Zhang Y, Zhu J, Zhang C, et al. Non-invasive early prediction of septic acute kidney injury by Doppler-based renal resistive indexes combined with echocardiographic parameters: an experimental study. Front Med. 2021;8:723837. doi:10.3389/fmed.2021.723837
41. Zhou W, Zhang N, Ma S, et al. Clinical value of renal artery resistance index and urinary angiotensinogen in early diagnosis of acute kidney injury in patients with sepsis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2022;34(11):1183–1187. doi:10.3760/cma.j.cn121430-20220302-00194
42. Patel ML, Mishra H, Sachan R, Singh VK, Gangwar R, Ali W. Diagnostic accuracy of plasma cystatin c and renal resistive index for acute kidney injury in critically Ill Patients: a prospective observational study. Niger Med J. 2023;64(5):692–703. doi:10.60787/NMJ-64-5-292
43. Darmon M, Ostermann M, Cerda J, et al. Diagnostic work-up and specific causes of acute kidney injury. Intensive Care Med. 2017;43(6):829–840. doi:10.1007/s00134-017-4799-8
44. Zhi HJ, Zhao J, Nie S. Prediction of acute kidney injury: the ratio of renal resistive index to semiquantitative power Doppler ultrasound score-A better predictor? A prospective observational study. Medicine. 2019;98(21):e15465. doi:10.1097/MD.0000000000015465
45. Devani K, Charilaou P, Radadiya D, et al. Acute pancreatitis: trends in outcomes and the role of acute kidney injury in mortality- A propensity-matched analysis. Pancreatology. 2018;18(8):870–877. doi:10.1016/j.pan.2018.10.002
46. Yang Y, Xiao W, X L, et al. Machine learning-assisted ensemble analysis for the prediction of acute pancreatitis with acute kidney injury. Int J Gen Med. 2022;15:5061–5072. doi:10.2147/IJGM.S361330
47. Edelstein CL. Biomarkers of acute kidney injury. Adv Chronic Kidney Dis. 2008;15(3):222–234. doi:10.1053/j.ackd.2008.04.003
48. Aggarwal A, Singh S, Singh R, Poddar B, Baronia A. Procalcitonin kinetics as a prognostic marker in severe sepsis/septic shock. Indian J Crit Care Med. 2015;19(3):140–146. doi:10.4103/0972-5229.152755
49. Kan WC, Huang YT, Wu VC, Shiao CC. Predictive ability of procalcitonin for acute kidney injury: a narrative review focusing on the interference of infection. Int J Mol Sci. 2021;22(13).
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


