Back to Journals » Clinical Ophthalmology » Volume 18
Surgical Outcomes of Mitomycin-C Augmented Trabeculectomy in Neovascular Glaucoma and Prognostic Factors for Surgical Failure in Thailand
Authors Threetong T , Yongsiri S, Annopawong K
Received 27 August 2024
Accepted for publication 23 October 2024
Published 1 November 2024 Volume 2024:18 Pages 3111—3123
DOI https://doi.org/10.2147/OPTH.S485331
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Thanatporn Threetong,1 Somchai Yongsiri,2 Kornkamol Annopawong3
1Department of Ophthalmology, Faculty of Medicine, Burapha University, Chonburi, Thailand; 2Department of Medicine, Faculty of Medicine, Burapha University, Chonburi, Thailand; 3Department of Ophthalmology, Rajavithi Hospital and College of Medicine, Rangsit University, Bangkok, Thailand
Correspondence: Kornkamol Annopawong, Department of Ophthalmology, Rajavithi Hospital and College of Medicine, Rangsit University, 2, PhayaThai Road, Thung PhayaThai, Ratchathewi, Bangkok, 10400, Thailand, Tel +66949951594, Email [email protected]
Purpose: To evaluate the surgical outcomes and identify ocular and systemic prognostic factors of trabeculectomy with mitomycin C (MMC) in the eyes of patients with neovascular glaucoma (NVG) in Thailand.
Patients and Methods: This retrospective study was conducted by reviewing records of Thai patients with NVG who underwent trabeculectomy with MMC between 2013 and 2022. Criterion failure was defined as intraocular pressure (IOP) > 21 mmHg or less than a 20% reduction below baseline on two consecutive study visits after 3 months, IOP ≤ 5 mmHg on two consecutive study visits after 3 months, reoperation for glaucoma, and loss of light perception. Kaplan–Meier survival curves were used to examine success rates, and risk factors were analyzed using Cox’s proportional hazard model.
Results: The study included 106 eyes of 106 patients with a mean age of 57 years (range, 27– 87 years). The cause of NVG was proliferative diabetic retinopathy (PDR) in 63 eyes (59.43%), central retinal vein occlusion (CRVO) in 39 eyes (36.79%), and ocular ischemic syndrome (OIS) in 4 eyes (3.77%). The cumulative probability of success in the first year was 73.6% with anti-glaucoma medication and 54.7% without medication. The multivariate model demonstrated that major cardiovascular events (hazard ratio [HR], 2.778 p=0.001) and preoperative systemic antiglaucoma medication use (HR, 1.837, p=0.045) were prognostic factors for surgical failure among all NVG patients. Postoperative manipulation with a subconjunctival injection of MMC occurred significantly more frequently in the failure group (HR, 3.100; p< 0.001).
Conclusion: Trabeculectomy with MMC effectively reduced the elevated IOP associated with NVG in Thailand. Underlying systemic diseases involving major vascular events and the use of adjunct systemic IOP-lowering medications were prognostic factors for surgical failure.
Keywords: intraocular pressure, major vascular events, stroke, myocardial infarction, vascular endothelial growth factor
Introduction
Neovascular glaucoma (NVG) is known to cause severe vision loss due to an imbalance of angiogenic factors, resulting in neovascularization of the anterior chamber structures and progressive angle closure.1 This condition often arises from certain ocular diseases, particularly ischemic retinal conditions such as proliferative diabetic retinopathy (PDR), central retinal vein occlusion (CRVO), and ocular ischemic syndrome (OIS).2 The primary treatment objective is to limit and minimize ocular and retinal ischemia using laser pan-retinal photocoagulation (PRP) and intravitreal anti-vascular endothelial growth factor (anti-VEGF) injection.1,2 Nevertheless, it is crucial to note that this treatment strategy alone may not be sufficient for intraocular pressure (IOP) control. When antiglaucoma medications are maximally tolerated, trabeculectomy and glaucoma drainage device (GDD) implantation are the treatments of choice, with comparable surgical success and IOP reduction in NVG.3,4 However, trabeculectomy requires fewer surgical instruments and shorter operation time, and may represent a more cost-effective measure compared with GDD implantation.
Several surgical techniques of trabeculectomy for NVG had been modified to improve surgical outcome. For example, intraoperative antimetabolites have been used to improve trabeculectomy outcomes. In addition, mitomycin-C (MMC), a more potent fibroblast inhibitor than 5-fluorouracil (5-FU), downregulates subconjunctival fibrosis and enhances surgical success.5 The use of anti-VEGF has been recommended as an adjunct to trabeculectomy because it has demonstrated to enhance surgical success and reduce postoperative complications.6,7 VEGF is well recognized as a core factor that mediates inflammation and both physiological and pathological angiogenesis.8 It plays a significant role in the pathogenesis of intraocular neovascularization in NVG.9 The coexistence of systemic vascular diseases is commonly observed in most patients with NVG. VEGF gene expression is also present in arteries from the early to advanced stages of atherosclerosis, and the degree of expression is associated with the severity of the disease.10
A number of preoperative baseline characteristics in NVG patients were reported as prognostic factors for trabeculectomy outcome; PDR, persistent neovascularization of the iris (NVI), a higher number of anti-VEGF injections, delayed trabeculectomy,11 a greater extent of peripheral anterior synechia (PAS),12 a lower preoperative IOP (<30 mmHg), vitrectomy after trabeculectomy,13 and history of vitrectomy12,14 were associated with poorer surgical outcomes. However, the impact of age to surgical success is inconclusive.11,14 Furthermore, postoperative hyphema was significantly correlated with the outcome of trabeculectomy for NVG.15
The primary objective of this study was to evaluate the surgical outcomes and identify prognostic factors of trabeculectomy with MMC as a treatment for NVG. Notably, our investigation incorporated an assessment of systemic risk factors, a unique aspect that, to the best of our knowledge, apart from age and sex, has not been addressed in previous studies.
Material and Methods
Patients
We retrospectively reviewed the medical records of Thai patients with neovascular glaucoma aged >18 years who were referred to two tertiary centers (1, Burapha University Hospital, Chonburi, eastern Thailand; 2, Rajavithi Hospital, Bangkok, central Thailand) between 2013 and 2022. Only patients who underwent primary trabeculectomy with MMC were included. The exclusion criteria were: 1) no light perception, 2) eyes with any other prior glaucoma surgery, and 3) less than 6 months postoperative follow-up period. This study was approved by the Institutional Review Board of both hospitals (Ethics approval numbers 026/2566 and 110/2567, respectively). The informed consents were obtained from all participants. However, the lost-to-follow participants by the data collection period, informed consents were waived by the Institutional Review Board ethics committee of both hospitals regarding to retrospective nature of this study. The study adhered to patient data confidentiality and was conducted in compliance with the principles of the Declaration of Helsinki.
NVG was categorized based on the presence of neovascularization of the iris (NVI) and/or neovascularization of the angle (NVA), coupled with an IOP exceeding 21 mmHg. If both eyes satisfied the qualifying criteria, only the left eye was included in the study.
The following information was collected at baseline. Systemic factors included age, sex, laterality, glomerular filtration rate (GFR-mL/min/1.73 m2), and underlying diseases (diabetes mellitus, hypertension, coronary artery disease, stroke, and dyslipidemia). Ocular factors include the cause of NVG (PDR, CRVO, and OIS), presence of concurrent vitreous hemorrhage, prior vitrectomy, IOP (mmHg - examined by Goldmann applanation tonometer [GAT]), antiglaucoma medications, peripheral anterior synechiae (PAS-quadrant), prior pan-retinal photocoagulation (PRP), number and time of anti-vascular endothelial growth factor (anti-VEGF) injection, lens status, and visual acuity (LogMAR) taken at the nearest visit before the surgery. Eyes without form vision were assigned the following scores: counting finger = 2.3, hand motion = 2.6, light perception = 2.9, and no light perception = 4.0.
Postoperative assessments, including visual acuity, IOP, and the number of antiglaucoma medications, were documented for 12 months. Additionally, other postoperative complications and subsequent management procedures, such as the administration of anti-VEGF, PRP, needling, and subconjunctival anti-metabolites (MMC and 5-FU), were recorded.
Surgical Technique
PRP was administered whenever feasible prior to the surgery. Additionally, intravitreal anti-VEGF injections (1.25 mg of bevacizumab) were delivered using a sterile technique under topical anesthesia before surgery. Trabeculectomy was performed by glaucoma specialists or in-training glaucoma fellows under supervision in a fornix-based manner. There are two MMC application techniques: subconjunctival injection and sub-tenon-soaked sponge, depending on the surgeon’s preferences. The subconjunctival injection technique involved 10–20 µg / 0.1–0.2 mL after conjunctival closure. The sub-tenon-soaked sponge technique used multiple pieces of 0.4 mg/mL MMC-soaked sponge directly applied to the sub-tenon’s pocket without touching the conjunctival edges for 2–4 minutes. After removing the sponges, irrigation with balanced salt was performed. A rectangular or square scleral flap, approximately 40–60% of the scleral thickness was created. A 2×2 mm sclerostomy was then created using a punch, and peripheral iridectomy was performed. The scleral flap was sutured using at least one stitch of 10–0 nylon. Postoperatively, each patient was properly educated about postoperative care by assigned expert medical personnel and was prescribed topical antibiotics four times a day for one month, coupled with a topical steroid administered in a gradually decreasing dosage for a minimum of three months. Laser suture lysis could be performed according to IOP status and bleb morphology.
Main Outcome
Trabeculectomy was considered a complete success if the IOP remained at or below 21 mmHg without the need for ocular hypotensive medication, and the visual acuity was light perception or better. Conversely, qualified success was achieved if the same criteria were met with the use of medications. Failure was defined as IOP exceeding 21 mmHg or demonstrating less than a 20% reduction below baseline on two consecutive visits 3 months after the procedure. Additionally, failure criteria included IOP remaining at or below 5 mmHg on two consecutive visits after 3 months, the need for additional intraoperative procedures (excluding needling) to control the IOP, or loss of light perception.
Statistical Analysis
Data analysis was conducted using SPSS software (IBM SPSS Statistics 28, IBM Corp., New York). Continuous data are presented as means and standard deviations, while categorical data are presented as percentages (%). The cumulative probability of success was determined using Kaplan–Meier survival curves. Risk factors for failure, postoperative complications, and postoperative manipulations were assessed through Cox proportional hazards regression analysis. Statistical significance was established with a two-sided p-value of less than 0.05.
Results
A total of 106 patients met the inclusion criteria. The mean age of the patients was 57.07 ± 11.79 years, ranging from 27 to 87 years. Sixty-three patients (59.43%) were male and 43 patients (40.57%) were female. Underlying diseases included diabetes mellitus (80.19%), hypertension (73.58%), and major vascular events (coronary artery disease and stroke, 16.98%). Then mean GFR was 60.34 ± 30.83 mL/min/1.73 m2 with a range from 4.2 to 124.0, stratified into chronic kidney disease in different stages including stage 1 (22.64%), stage 2 (27.36%), stage 3a (19.81%), stage 3b (9.43%), stage 4 (11.32%), and stage 5 (9.43%), according to Kidney Disease Improving Global Outcomes (KDIGO) criteria. Among these patients, seven underwent renal replacement therapy, with two receiving hemodialysis (HD) and five undergoing continuous ambulatory peritoneal dialysis (CAPD). The baseline systemic characteristics are summarized in Table 1.
 |
Table 1 Systemic Baseline Characteristics |
Of the ocular baseline characteristics, 22 patients had bilateral NVG and 6 underwent bilateral trabeculectomy. Only the left eyes in patients who satisfied the inclusion criteria were included in the study. Overall, there was an equal distribution between the right and left eyes (50.94% and 49.06%, respectively). The primary cause of NVG was PDR in 63 (59.43%) eyes. This was followed by CRVO in 39 eyes (36.97%) and OIS in 4 eyes (3.77%). The average visual acuity was 1.89 ± 0.86 Log MAR (range, 0.1–2.9 Log MAR). Most eyes (76.42%) had severe visual loss, with a visual acuity of less than 20/200. Only 10.38% of patients had a visual acuity of 20/70 or better. The mean IOP before surgery was 38.78 ± 13.01 (range, 10–74) mmHg. Eighty-one eyes (76.42%) had an IOP of at least 30 mmHg, whereas 25 eyes (23.58%) had an IOP <30 mmHg. Fifty-one eyes (48.11%) required only topical IOP-lowering medications; all of them took at least two medications, but the majority (41 eyes, 80.39%) had four topical medications. However, 55 eyes (51.89%) received adjunct systemic IOP-lowering medications including oral acetazolamide and/or glycerin. Almost all eyes (94 eyes, 88.68%) had gonioscopic angle closure, defined as the presence of PAS in 2–4 quadrants in 5.66%, 9.43%, and 73.58% of eyes, respectively. Twenty-five eyes (23.58%) had a history of cataract surgery and 13 (12.26%) had undergone vitreoretinal surgery. Thirty-seven patients (34.91%) had concurrent vitreous hemorrhage. Eighty-two eyes (77.36%) had undergone laser PRP preoperatively, and 100 eyes (94.34%) had intravitreous anti-VEGF within 7 days in 24%, 7–30 days in 43%, and after 30 days in 33% of cases. Ocular demographic data of the patients are summarized in Table 2.
 |
Table 2 Ocular Baseline Characteristics |
Kaplan–Meier analysis exhibited that the overall success rates at one year with and without medication were 73.6% and 54.7%, respectively (Figure 1).
 |
Figure 1 Kaplan–Meier analysis of trabeculectomy with MMC for NVG (red line-complete success, blue line-qualified success). Abbreviation: NVG, neovascular glaucoma. |
From the clinical data, the leading cause of trabeculectomy failure owing to failure criterion was uncontrolled IOP (defined as IOP >21 mmHg or less than a 20% reduction below baseline on two consecutive study visits after 3 months) in 25 eyes (52.1%), followed by reoperation, loss of light perception, and hypotony (defined as IOP ≤5 mmHg on 2 consecutive study visits after 3 months) in 13, 8, and 2 eyes (27%, 16.7%, and 4.2%) respectively (Table 3). The most common reoperative procedure was GDD implantation in 10 eyes (76.9%), followed by cyclophotocoagulation and revised trabeculectomy in 2 eyes (15.4%) and 1 eye (7.7%), respectively (Table 4).
 |
Table 3 Failure Reason |
 |
Table 4 Reoperation Procedure |
We evaluated the systemic risk factors for trabeculectomy failure (Table 5). Cox proportional hazards regression analysis demonstrated that hypertension was correlated with the risk of trabeculectomy failure (crude hazard ratio [HR], 2.164, p=0.046). Major vascular events (crude HR 2.695, p=0.002) were also significant prognostic factors of surgical failure. The age of the patients (<50 or ≥50 years) and sex did not seem to affect the survival (p=0.485, 0.333 respectively). Other investigated underlying systemic diseases, including diabetes mellitus, dyslipidemia, CKD stage, and renal replacement therapy, also had no significant effect on survival rate in the univariate analysis.
 |
Table 5 Cox Proportional Hazard Regression Analysis Assesses Systemic Factors |
Kaplan–Meier survival analysis was performed to compare the surgical success rates between eyes with and without major vascular events (Figure 2; p=0.002).
 |
Figure 2 Kaplan–Meier analysis of trabeculectomy with MMC for NVG (red line-major vascular event, blue line-no major vascular event). Abbreviation: NVG, neovascular glaucoma. |
In multivariate Cox regression analysis, only major vascular events were ascertained as predictive factors for surgical failure independent of each other (HR, 2.778, p=0.001).
The potential ocular prognostic factors influencing survival time are listed in Table 6. The prognostic factors found to be significant were the number of antiglaucoma medications (p=0.026) and additional systemic IOP-lowering medications (HR, 1.987, p=0.022) in the univariate analysis. However, significant differences were found only for additional systemic IOP-lowering medications (HR, 1.837, p=0.045) in the multivariate analysis. Other preoperative ocular factors studied were laterality, cause of NVG, visual acuity, IOP, PAS, stage of NVG, lens status, previous vitreoretinal surgery, concurrent vitreous hemorrhage, preoperative PRP, and preoperative anti-VEGF. They had no significant effect on trabeculectomy outcomes.
 |
Table 6 Cox Proportional Hazard Regression Analysis Assesses Ocular Factors |
Kaplan–Meier survival analysis was performed to compare the surgical success rates between eyes with and without combined systemic medications (Figure 3, p=0.045).
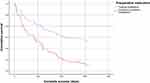 |
Figure 3 Kaplan-Meier analysis of trabeculectomy with MMC for NVG (red line-combined systemic medication, blue line-only topical medication). |
Cox proportional hazards regression analysis demonstrated that postoperative manipulation with anti-VEGF, PRP, and 5-FU had no significant effect on survival rate. Needling and MMC subconjunctival augmentation were correlated with trabeculectomy failure in the univariate analysis, p=0.007 and p<0.001 respectively. In multivariate Cox regression analysis, postoperative subconjunctival MMC was identified as significant association with trabeculectomy failure (Table 7, HR, 3.100, p<0.001). Survival analysis revealed that patients who underwent postoperative MMC subconjunctival injection had significantly poorer outcomes than those who did not receive MMC (Figure 4, p<0.001).
 |
Table 7 Cox Proportional Hazard Regression Analysis Assesses Postoperative Manipulation |
 |
Figure 4 Kaplan-Meier analysis of trabeculectomy with MMC for NVG (red line-MMC, blue line-no MMC). |
Complications encountered during the postoperative period are listed in Table 8. The most common postoperative complications included hyphema in 14.15% of the cases followed by hypotony, choroidal detachment (CD), and bleb leak accounting for 11.32%, 9.43%, and 5.66%, respectively. However, no significant differences were observed in the univariate analysis.
 |
Table 8 Postoperative Complication |
Discussion
This study investigated the surgical success rate and systemic and ocular prognostic factors of trabeculectomy with MMC for NVG in Thailand. Survival analysis showed that the overall complete and qualified success rates at one year were 54.7% and 73.6%, respectively. Our complete success rate was favorable compared to that of a previous study,11 where a complete success rate of 50% at one year was observed in the NVG group with proliferative diabetic retinopathy. However, the results were much higher in a study by Higashide et al in 2015,13 which reported a complete success rate of 86.9% in 61 eyes treated with NVG. This discrepancy in outcomes may be attributed to the differences in baseline characteristics among the study populations. Notably, over 90% of the participants in our study were in the advanced stage of neovascular glaucoma (closed angle), in contrast to the 59% reported in a previous study. This finding is also supported by the Kiuchi study,12 which demonstrated a significant correlation between extensive PAS and increased surgical failure rates. In terms of qualified success, these research results aligned consistently with prior studies (62.6–93.4%).11–14,16–18 Researchers must exercise caution when interpreting and comparing success results, because previous studies may have possibly employed varying definitions of failure. While some studies included hypotony (IOP ≤5 mmHg) as a failure criterion,11,13 others did not.12,14,16–18 Furthermore, some studies13 have focused on achieving a specific percentage reduction in the IOP.
Several studies have investigated the ocular risk factors of trabeculectomy in patients with NVG. The prognostic factors varied among the studies. Takihara et al concluded that a younger age and a history of vitrectomy were predictive factors for surgical failure.14 According to Senthil et al, factors associated with trabeculectomy failure include older age, PDR, persistent NVI, a higher number of anti-VEGF injections, and delayed trabeculectomy.11 Kiuchi et al found that patients with NVG with a greater extent of peripheral anterior synechia and a history of vitrectomy had poorer outcomes,12 whereas Higashide et al reported that a lower preoperative IOP (<30 mmHg) and vitrectomy after trabeculectomy were associated with higher trabeculectomy failure in NVG.13 To the best of our knowledge, no study has examined the systemic risk factors other than age and sex in patients with NVG and surgical failure of trabeculectomy with MMC.
In this study, underlying major vascular events (HR, 2.778; p=0.001) were identified as significant risk factors for surgical failure according to the complete success criteria in multivariate analysis. There have been no previous reports of cardiovascular disease and stroke associated with trabeculectomy failure in NVG. However, three cases have been reported on the incidence of neovascular glaucoma (one case from OIS19 and two cases from PDR20,21 after the early postoperative coronary artery bypass graft [CABG] procedure in cardiovascular disease patients). Oda et al reported a case of stroke in one month after NVG due to PDR.22 According to Nielsen, neovascular glaucoma is also significantly associated with macrovascular diseases, including cardiovascular disease, hypertension, cerebrovascular stroke, and gangrene amputation.23
From both the molecular and clinical perspectives, it is evident that NVG and ischemic stroke share similar pathogenesis, supported by elevated VEGF levels observed during the progression of both conditions.9,24–28 VEGF levels are increased in the aqueous humor of patients with glaucoma and rabbit models, indicating its role in the disease process. Additionally, studies have demonstrated that VEGF stimulates fibroblast proliferation in vitro, potentially leading to scar formation after filtration surgery.29 Park et al highlighted a noteworthy association between higher levels of VEGF in Tenon’s capsule at the time of surgery and a greater risk of failure and poorer IOP outcomes at one year in patients with primary open-angle glaucoma (POAG).30 The study by Kim et al in 2009 also confirmed the same relationship in NVG patients who underwent Ahmed implantation.31 These findings suggest the potential benefits of adjunctive anti-VEGF therapy in trabeculectomy to enhance surgical outcomes, correlating with a recent systematic review of 2023.7
Major vascular events, especially myocardial infarction, may secrete the circulatory cytokines growth differentiation factor 3 (GDF-3),32 galectin-3,33,34 and arginase-135 in response to ischemia. These cytokines promote cell proliferation and fibroblast activation in the ischemic heart. Angiogenesis has also been established to compensate for the reductions in blood flow and oxygen supply.36 Angiogenesis is essential for recovery and protection following cerebral ischemia. The expression of activin receptor-like kinase 5 (ALK5) was significantly elevated after ischemic stroke and could promote extracellular matrix production, stimulate mesenchymal cell differentiation, and induce vascular maturation.37 These secretory cytokines from compensatory mechanisms promote local tissue remodeling. However, the effects contributing to ocular tissue fibrosis and angiogenesis, resulting in adverse consequences at the trabeculectomy site, need to be further elucidated.
In our multivariate analysis, we discovered that preoperative systemic medication use was associated with an increased risk of trabeculectomy failure. The use of systemic medication often indicates more severe NVG, which could independently affect surgical outcomes. The administration of systemic medications, such as oral acetazolamide and/or glycerin, indicated that NVG eyes already had maximal tolerable topical medications, potentially harming conjunctival tissue and affecting trabeculectomy outcomes.38–40 However, in our study, the number of preoperative topical medications showed a significant association with the risk of failure in the univariate analysis but failed to show significance in the multivariate analysis.
Our retrospective cohort study also found that postoperative MMC injections were significantly associated with surgical failure (HR, 3.100; p<0.001). This likely results from the higher possibility of postoperative subconjunctival MMC injections observed in cases prone to failure.
This study had some limitations. First, the retrospective design and lack of a control group are the major limitations. Second, the involvement of multiple surgeons across two tertiary care centers may have hindered the standardization of surgical procedures. Additionally, there was a potential for selection bias, because the study was conducted in a tertiary center where more complex or advanced cases are often referred. Furthermore, the relatively short follow-up period might have restricted our ability to identify additional long-term prognostic factors.
The strength of our study lies in its pioneering analysis of preoperative systemic factors as prognostic contributors to trabeculectomy with MMC outcomes in NVG patients, providing valuable additional insights. This study identified associations between baseline clinical characteristics, including major vascular events, and the risk of trabeculectomy with MMC failure in NVG. These results may initiate the design of an ideally prospective randomized study with a larger sample size and longer follow-up period to validate the association of major vascular events, including cardiovascular disease and stroke, after trabeculectomy with MMC survival in patients with NVG.
Conclusion
We found that trabeculectomy with MMC effectively reduced elevated IOP associated with NVG in Thailand. Among the risk factors identified for trabeculectomy with MMC failure using the complete success criteria, underlying major vascular events and adjunct preoperative systemic IOP-lowering medications were significant negative prognostic factors.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Senthil S, Dada T, Das T, et al. Neovascular glaucoma-A review. Indian J Ophthalmol. 2021;69(3):525–534. doi:10.4103/ijo.IJO_1591_20
2. Shazly TA, Latina MA. Neovascular glaucoma: etiology, diagnosis and prognosis. Semin Ophthalmol. 2009;24(2):113–121. doi:10.1080/08820530902800801
3. Shen CC, Salim S, Du H, Netland PA. Trabeculectomy versus Ahmed glaucoma valve implantation in neovascular glaucoma. Clin Ophthalmol. 2011;5(1):281–286. doi:10.2147/OPTH.S16976
4. Tokumo K, Komatsu K, Yuasa Y, et al. Treatment outcomes in the neovascular glaucoma tube versus trabeculectomy study. Graefes Arch Clin Exp Ophthalmol. 2021;259(10):3067–3076. doi:10.1007/s00417-021-05257-2
5. Katz GJ, Higginbotham EJ, Litcher PR, et al. Mitomycin C versus 5-Fluorouracil in high-risk glaucoma filtering surgery Extended follow-up. Ophthalmology. 1995;102(9):1263–1269. doi:10.1016/S0161-6420(95)30875-5
6. Saito Y, Higashide T, Takeda H, Ohkubo S, Sugiyama K. Beneficial effects of preoperative intravitreal bevacizumab on trabeculectomy outcomes in neovascular glaucoma. Acta Ophthalmol. 2010;88(1):96–102. doi:10.1111/j.1755-3768.2009.01648.x
7. Zhou X, Chen J, Luo W, Du Y. Short-term outcomes of trabeculectomy with or without anti-VEGF in patients with neovascular glaucoma: a systematic review and meta-analysis. Transl Vis Sci Technol. 2023;12(9):12. doi:10.1167/tvst.12.9.12
8. Dabravolski SA, Khotina VA, Omelchenko AV, Kalmykov VA, Orekhov AN. The role of the VEGF family in atherosclerosis development and its potential as treatment targets. Int J Mol Sci. 2022;23(2):931. doi:10.3390/ijms23020931
9. Tripathi RC, Li J, Tripathi BJ, Chalam KV, Adamis AP. Increased level of vascular endothelial growth factor in aqueous humor of patients with neovascular glaucoma. Ophthalmology. 1998;105(2):232–237. doi:10.1016/S0161-6420(98)92782-8
10. Morsi WG, Shaker OG, Ismail EF, et al. HO-1 and VGEF gene expression in human arteries with advanced atherosclerosis. Clin Biochem. 2006;39(11):1057–1062. doi:10.1016/j.clinbiochem.2006.08.003
11. Senthil S, Chary R, Ali MH, et al. Trabeculectomy for neovascular glaucoma in proliferative diabetic retinopathy, central retinal vein occlusion, and ocular ischemic syndrome: surgical outcomes and prognostic factors for failure. Indian J Ophthalmol. 2021;69(11):3341–3348. doi:10.4103/ijo.IJO_1516_21
12. Kiuchi Y, Sugimoto R, Nakae K, Saito Y, Ito S. Trabeculectomy with mitomycin C for treatment of neovascular glaucoma in diabetic patients. Ophthalmologica. 2006;220(6):383–388. doi:10.1159/000095865
13. Higashide T, Ohkubo S, Sugiyama K, Shukla D. Long-term outcomes and prognostic factors of trabeculectomy following intraocular bevacizumab injection for neovascular glaucoma. PLoS One. 2015;10(8):e0135766. doi:10.1371/journal.pone.0135766
14. Takihara Y, Inatani M, Fukushima M, Iwao K, Iwao M, Tanihara H. Trabeculectomy with mitomycin C for neovascular glaucoma: prognostic factors for surgical failure. Am J Ophthalmol. 2009;147(5):912–918. doi:10.1016/j.ajo.2008.11.015
15. Nakatake S, Yoshida S, Nakao S, et al. Hyphema is a risk factor for failure of trabeculectomy in neovascular glaucoma: a retrospective analysis. BMC Ophthalmol. 2014;14:55. doi:10.1186/1471-2415-14-55
16. Takihara Y, Inatani M, Kawaji T, et al. Combined intravitreal bevacizumab and trabeculectomy with mitomycin C versus trabeculectomy with mitomycin C alone for neovascular glaucoma. J Glaucoma. 2011;20(3):196–201. doi:10.1097/IJG.0b013e3181d9ce12
17. Miki A, Oshima Y, Otori Y, Matsushita K, Nishida K. One-year results of intravitreal bevacizumab as an adjunct to trabeculectomy for neovascular glaucoma in eyes with previous vitrectomy. Eye. 2011;25(5):658–659. doi:10.1038/eye.2010.234
18. Kobayashi S, Inoue M, Yamane S, Sakamaki K, Arakawa A, Kadonosono K. Long-term outcomes after preoperative intravitreal injection of bevacizumab before trabeculectomy for neovascular glaucoma. J Glaucoma. 2016;25(3):281–284. doi:10.1097/IJG.0000000000000211
19. Chaturvedi PK, Kumar S, Kumar P, Prasad SP. Ocular ischemic syndrome: a rare cause of postoperative visual loss following coronary artery bypass graft (CABG) surgery. Med J Armed Forces India. 2016;72:S123–S125. doi:10.1016/j.mjafi.2015.11.013
20. Raman V, Lambley R. Rapidly progressive neovascular glaucoma following coronary artery bypass graft surgery in a patient with type 1 diabetes mellitus: a case report. J Med Case Rep. 2018;12(1):36. doi:10.1186/s13256-018-1564-8
21. Chadha V, Styles C. Progression of diabetic retinopathy following coronary artery bypass graft. Eye. 2007;21(6):864–865. doi:10.1038/sj.eye.6702731
22. Oda Y, Hashimoto Y, Ueyama H, Uchino M, Araki S. A case of ischemic oculopathy followed by border zone infarction. Clin Neurol. 1989;29(6):747–753.
23. Nielsen NV. The prevalence of glaucoma and ocular hypertension in type 1 and 2 diabetes mellitus: an epidemiological study of diabetes mellitus on the island of Falster, Denmark. Acta Ophthalmol. 1983;61(4):662–672. doi:10.1111/j.1755-3768.1983.tb04357.x
24. Shoamanesh A, Preis SR, Beiser AS, et al. Circulating biomarkers and incident ischemic stroke in the Framingham offspring study. Neurology. 2016;87(12):1206–1211.
25. Giordano M, Ciarambino T, D’amico M, et al. Circulating mIRNA-195-5p and-451a in transient and acute ischemic stroke patients in an emergency department. J Clin Med. 2019;8(2):130. doi:10.3390/jcm8020130
26. Matsuo R, Ago T, Kamouchi M, et al. Clinical significance of plasma VEGF value in ischemic stroke-research for biomarkers in ischemic stroke (REBIOS) study. BMC Neurol. 2013;13:32. doi:10.1186/1471-2377-13-32
27. Xue L, Chen H, Zhang T, Chen J, Geng Z, Zhao Y. Changes in serum vascular endothelial growth factor and endostatin concentrations associated with circulating endothelial progenitor cells after acute ischemic stroke. Metab Brain Dis. 2017;32(2):641–648. doi:10.1007/s11011-017-9953-z
28. Slevin M, Krupinski J, Slowik A, Kumar P, Szczudlik A, Gaffney J. Serial measurement of vascular endothelial growth factor and transforming growth factor-1 in serum of patients with acute ischemic stroke. Stroke. 2000;31:1863–1870. doi:10.1161/01.STR.31.8.1863
29. Li Z, van Bergen T, van de Veire S, et al. Inhibition of vascular endothelial growth factor reduces scar formation after glaucoma filtration surgery. Invest Ophthalmol Vis Sci. 2009;50(11):5217–5225. doi:10.1167/iovs.08-2662
30. Park HYL, Kim JH, Ahn MD, Park CK. Level of vascular endothelial growth factor in tenon tissue and results of glaucoma surgery. Arch Ophthalmol. 2012;130(6):685–689. doi:10.1001/archophthalmol.2011.2799
31. Kim YG, Hong S, Lee CS, et al. Level of vascular endothelial growth factor in aqueous humor and surgical results of Ahmed glaucoma valve implantation in patients with neovascular glaucoma. J Glaucoma. 2009;18(6):443–447. doi:10.1097/IJG.0b013e3181895e5c
32. Masurkar N, Bouvet M, Logeart D, et al. Novel cardiokine GDF3 predicts adverse fibrotic remodeling after myocardial infarction. Circulation. 2023;147(6):498–511. doi:10.1161/CIRCULATIONAHA.121.056272
33. Suthahar N, Meijers WC, Silljé HHW, Ho JE, Liu FT, de Boer RA. Galectin-3 activation and inhibition in heart failure and cardiovascular disease: an update. Theranostics. 2018;8(3):593–609. doi:10.7150/thno.22196
34. Wang X, Gaur M, Mounzih K, et al. Inhibition of galectin-3 post-infarction impedes progressive fibrosis by regulating inflammatory profibrotic cascades. Cardiovasc Res. 2023;119(15):2536–2549. doi:10.1093/cvr/cvad156
35. Tengbom J, Cederström S, Verouhis D, et al. Arginase 1 is upregulated at admission in patients with ST-elevation myocardial infarction. J Intern Med. 2021;290(5):1061–1070. doi:10.1111/joim.13358
36. Losordo DW, Dimmeler S. Therapeutic angiogenesis and vasculogenesis for ischemic disease: part I: angiogenic cytokines. Circulation. 2004;109(21):2487–2491. doi:10.1161/01.CIR.0000128595.79378.FA
37. Li S, Hafeez A, Noorulla F, et al. Preconditioning in neuroprotection: from hypoxia to ischemia. Prog Neurobiol. 2017;157:79–91. doi:10.1016/j.pneurobio.2017.01.001
38. Servat JJ, Bernardino CR. Effects of common topical antiglaucoma medications on the ocular surface, eyelids and periorbital tissue. Drug Aging. 2011;28(4):267–282. doi:10.2165/11588830-000000000-00000
39. Leng F, Liu P, Li H, Zhang J. Long-term topical antiglaucoma medications cause enhanced Tenon’s capsule fibroblast proliferation and abnormal TGF-β and MMP expressions: potential effects on glaucoma filtering surgery. Curr Eye Res. 2011;36(4):301–309. doi:10.3109/02713683.2010.547648
40. Broadway DC, Grierson I, O’brien C, Hitchings RA. Adverse effects of topical antiglaucoma medication II. the outcome of filtration surgery. Arch Ophthalmol. 1994;112:1446–1454. doi:10.1001/archopht.1994.01090230060021
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Effect of the COVID-19 Pandemic on Emergency Department Visits of Patients with an Emergent or Urgent Diagnosis
Yeh CC, Chien CY, Lee TY, Liu CH
International Journal of General Medicine 2022, 15:4657-4664
Published Date: 4 May 2022
Late Onset Occurrence of Concomitant Myocardial Infarction and Ischemic Stroke in Hospitalized COVID-19 Patient: A Case Report
Ianniciello A, Attena E, Carpinella G, Uccello A, Mauro C, Russo V
International Journal of General Medicine 2022, 15:6621-6626
Published Date: 16 August 2022
Adverse Clinical Outcomes Attributable to Socioeconomic and Ethnic Disparities Among People with Type 2 Diabetes in New Zealand Between 1994–2018: A Multiple Linked Cohort Study
Yu D, Osuagwu UL, Pickering K, Baker J, Cutfield R, Wang Z, Cai Y, Orr-Walker BJ, Sundborn G, Zhao Z, Simmons D
Clinical Epidemiology 2023, 15:511-523
Published Date: 1 May 2023
Identifying Risk Factors for Cardiovascular Events Among Active-Duty Service Members and Veterans Prescribed Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Forbes WL, Petway J, Gressler LE, Thorfinnson H, Costantino RC, Atkinson TJ
Journal of Pain Research 2024, 17:1133-1144
Published Date: 15 March 2024
Generation of Risk Score for Serious Non-Steroidal Anti-Inflammatory Drug (NSAID) Induced Cardiovascular Events (NAÏVE) Among Active-Duty Service Members and Veterans
Atkinson TJ, Petway J, Forbes WL, Thorfinnson H, Costantino RC, Gressler LE
Journal of Pain Research 2025, 18:1081-1094
Published Date: 6 March 2025

