Back to Journals » Journal of Inflammation Research » Volume 17
Systemic Immune-Inflammation Index and Systemic Inflammation Response Index Predict the Response to Radioiodine Therapy for Differentiated Thyroid Cancer
Authors Wang Y , Chang J, Hu B , Yang S
Received 28 August 2024
Accepted for publication 4 November 2024
Published 9 November 2024 Volume 2024:17 Pages 8531—8541
DOI https://doi.org/10.2147/JIR.S493397
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Adam Bachstetter
Yan Wang,1,2 Junshun Chang,1 Ben Hu,3 Suyun Yang1
1Department of Nuclear Medicine, First Hospital of Shanxi Medical University, Taiyuan, Shanxi, 030001, People’s Republic of China; 2Academy of Medical Sciences, Shanxi Medical University, Taiyuan, Shanxi, 030001, People’s Republic of China; 3The Fifth Clinical Medical School of Anhui Medical University, Hefei, Anhui, People’s Republic of China
Correspondence: Ben Hu; Suyun Yang, Email [email protected]; [email protected]
Purpose: This research sought to evaluate the clinical value of systemic immune-inflammation index and systemic inflammation response index in predicting the response to radioactive iodine (RAI) therapy in individuals diagnosed with differentiated thyroid cancer.
Patients and Methods: This retrospective study included 406 patients with differentiated thyroid cancer who received initial RAI therapy and follow-up from December 2019 to December 2023. Patients were divided into two groups based on imaging and serum indicators to evaluate the response to radioactive iodine treatment: the ER group (excellent response) and the non-ER group (suboptimal response). Systemic immune-inflammation index and systemic inflammation response index were calculated based on peripheral blood cell counts before treatment. Multivariable logistic regression analysis was used to assess the independent associations of these indices with the therapeutic response to radioiodine treatment. Receiver operating characteristic (ROC) curves were graphed and the area under the curve (AUC) was calculated to evaluate their predictive ability.
Results: Compared to the ER group, patients in the non-ER group had significantly elevated systemic immune-inflammation index and systemic inflammation response index levels (p < 0.001). After adjusting for confounding factors, there was a significant association between these indices and the response to radioactive iodine treatment in patients with differentiated thyroid cancer. The optimal cutoff values for predicting the response to RAI treatment were 668.91 for systemic immune-inflammation index (AUC=0.692, sensitivity 58.2%, specificity 73.1%, 95% CI: 0.639– 0.745, p < 0.001) and 0.47 for systemic inflammation response index (AUC=0.664, sensitivity 85.6%, specificity 42.7%, 95% CI: 0.612– 0.717, p < 0.001).
Conclusion: Systemic immune-inflammation index and systemic inflammation response index could be valuable for predicting the response to RAI treatment in individuals diagnosed with differentiated thyroid cancer. Further research is needed to explore their practical utility, and these novel inflammation markers could serve as adjunct tools in clinical practice.
Keywords: systemic immune-inflammation index, systemic inflammation response index, differentiated thyroid cancer, radioactive iodine therapy
Introduction
Thyroid cancer is the most common endocrine malignancy, and its incidence has been steadily increasing in recent decades.1,2 According to the International Agency for Research on Cancer of the World Health Organization, thyroid cancer ranked ninth in global cancer incidence in 2020.3 Differentiated thyroid cancer (DTC) accounts for over 90% of all types of thyroid cancer, including papillary, follicular, and oncocytic subtypes.4,5 It is typically an indolent tumor with low mortality and good prognosis.6 Radioactive iodine (RAI) therapy uses the radioactive isotope iodine-131 and is currently a widely used and effective treatment for DTC postoperatively. According to the treatment objectives, it can be divided into three levels: remnant ablation, adjuvant therapy, and treatment of known disease.7,8 In 2015, the American Thyroid Association (ATA) proposed a dynamic response assessment system, emphasizing that the initial response to RAI therapy is crucial for dynamically estimating the risk of recurrence and monitoring the disease outcome in DTC patients.9 It has been reported that approximately 15–20% of patients still experience recurrence/residual disease or gradually lose response to RAI after initial treatment.4,10,11 Consequently, these patients with suboptimal treatment response have increased rates of recurrence and disease-specific mortality.12 Furthermore, the inability to accurately identify populations with unsatisfactory prognosis results in a lack of clinical strategies to balance treatment risks and disease progression risks based on individual patient characteristics. This leads to a significant phenomenon of overtreatment with radioactive iodine in DTC, resulting in wastage of healthcare resources and decreased health-related quality of life for patients.13–15 Therefore, it is necessary to identify the factors influencing the response to RAI therapy in order to screen patients with suboptimal treatment efficacy early. However, current research on factors related to the response to RAI therapy mainly focuses on physiological factors associated with radioactive iodine avidity and thyroid function indicators. It is crucial to search for and validate additional potential prognostic markers, as it holds significant importance in identifying the clinical characteristics of patients with unsatisfactory treatment response and providing individualized ongoing management plans.
Promoting tumor inflammation and avoiding immune destruction are closely associated with the occurrence, development, and prognosis of cancer.16 In recent years, inflammatory markers, as biological molecules capable of reflecting the degree of host inflammation and immune function balance, have gained significant attention and have been proven to be prognostic indicators for various types of cancer.17 Compared to traditional inflammatory markers, inflammatory markers calculated using peripheral whole blood cell counts have the advantages of being easily obtainable and simple and cost-effective. Examples include the systemic immune-inflammation index (SII), systemic inflammation response index (SIRI), platelet-lymphocyte ratio (PLR), and neutrophil-lymphocyte ratio (NLR). Furthermore, a ten-year follow-up study involving 85,154 participants demonstrated that SII and SIRI have superior predictive capabilities for cancer prognosis compared to NLR and PLR.18
Given that the interaction between inflammatory factors and immune cells in the tumor microenvironment (TME) is an important factor influencing the prognosis and treatment outcomes of DTC, it is essential to explore the potential value of inflammatory markers in predicting the prognosis of DTC.19,20 However, research on their association with the prognosis of DTC is limited, and there have been no studies focusing on the predictive value of the novel inflammatory markers SII and SIRI for the response to radioactive iodine therapy in DTC. Therefore, the aim of this study is to analyze the correlation between the SII and SIRI levels before initial iodine therapy in DTC patients and treatment response, as well as to evaluate the predictive value of SII and SIRI for the response to RAI therapy.
Materials and Methods
Study Design and Participants
From December 2019 to December 2023, data was gathered from patients with DTC who received RAI treatment at the First Hospital of Shanxi Medical University in this retrospective study. Inclusion criteria: (1) Age ≥18 years; (2) The surgical procedure of thyroidectomy includes the complete or near-complete removal of the thyroid gland, with or without dissection of neck lymph nodes; (3) First-time RAI treatment; (4) Pre-treatment anti-thyroglobulin antibodies (TgAb) <115 IU/mL and thyroid-stimulating hormone (TSH) >30 uIU/mL. Among these patients, those meeting the following criteria were excluded: (1) Presence of autoimmune diseases; (2) Acute inflammatory diseases; (3) Participants with myeloproliferative and lymphoproliferative disorders; (4) Incomplete baseline data; (5) Participation in drug research institution trials; (6) Lack of follow-up records after RAI treatment or incomplete follow-up data. In the end, a total of 406 patients were included. This study adhered to the principles of the Helsinki Declaration and was approved by the Ethics Committee of the First Hospital of Shanxi Medical University (No. KYLL-2024-110). Given the retrospective nature of the study and the confidential handling of all patient data, the Ethics Committee of the First Hospital of Shanxi Medical University waived the requirement for informed consent. The participant flowchart is shown in Figure 1. This manuscript adheres to the corresponding STROBE checklist (Supplementary Table 1).
 |
Figure 1 The participant flowchart. |
Radioactive Iodine Therapy
Patients were instructed to adhere to a low-iodine dietary regimen for a period ranging from 2 to 4 weeks prior to the commencement of treatment, and to cease the intake of levothyroxine for a duration of 3 to 4 weeks as per physician’s instructions. On the day of admission, blood biochemistry tests and thyroid-related imaging studies were performed to comprehensively assess their baseline condition. The I-131 dose ranges from 1.11–5.55GBq (30–150mCi) or higher. All patients underwent a post-therapeutic I-131 whole-body scan (Rx-WBS) 2 to 7 days following the treatment. Subsequently, patients underwent regular follow-up visits to monitor changes in thyroid function indicators after I-131 therapy, adjust thyroid hormone doses, and maintain serum TSH levels within a reasonable suppression range in a timely manner.
Response Assessment
According to the 2015 ATA guidelines, the response to RAI therapy is assessed within 6–12 months post-RAI treatment based on both serological and imaging results.9 Serological results include changes and trends in thyroglobulin (Tg) and TgAb levels, while imaging results include neck ultrasound, diagnostic I-131 whole-body scan (Dx-WBS), CT, magnetic resonance imaging (MRI), whole-body bone scan, PET/CT, etc. According to the guidelines,9 patient treatment responses are classified as excellent response (ER), biochemical incomplete response (BIR), structural incomplete response (SIR), and indeterminate response (IDR). This process was independently carried out by two experienced nuclear medicine physicians, and the results were finally compiled and unified. In this study, we further transformed the four-category outcome into a two-category outcome: ER and non-ER (BIR+SIR+IDR).
Peripheral Blood Parameters
To ensure the sensitivity and accuracy of the test results, elbow venous blood samples were collected from each patient on the treatment day in the morning on an empty stomach. The collected blood parameters included platelet count, neutrophil count, lymphocyte count, and monocyte count. The formula for calculating SII is platelet count multiplied by neutrophil count divided by lymphocyte count, and the formula for calculating SIRI is neutrophil count multiplied by monocyte count divided by lymphocyte count.
Data Collection
Data collection was based on biological considerations and published literature,21–23 including age, gender, body mass index (BMI), smoking history, alcohol history, hypertension history, cardiovascular disease (CVD) history, diabetes history, time interval between thyroid surgery and RAI treatment, I-131 dose, tumor location, maximum tumor diameter, extrathyroidal extension, multifocality, number of lymph node metastases, location of lymph node metastases, pre-treatment stimulated thyroglobulin (presTg), and Rx-WBS results. According to the 8th edition of the American Joint Committee on Cancer (AJCC) guidelines and the 2015 ATA guidelines,9,24 patients were classified based on TNM staging, AJCC staging, and ATA risk stratification for recurrence. The results of data organization were carefully examined by two clinical doctors and, if there were any doubts, evaluated in detail by a nuclear medicine specialist.
Statistical Analysis
Analysis was performed using EmpowerStats (www.empowerstats.com) and R software version 4.3.2 (http://www.R-project.org). Continuous variables following a normal distribution were presented as mean (standard deviation) and compared using t-tests. For data that do not conform to a normal distribution, descriptions were provided using median and interquartile range, and comparisons were conducted using the Mann–Whitney test. Categorical variables were presented as frequencies and percentages, and compared using the chi-square test or Fisher’s exact test. The SII and SIRI were categorized into tertiles, and the association of SII and SIRI with the response to RAI treatment was analyzed using multivariate logistic regression. The regression models (Model 1 to Model 2) were tested by adjusting for potential confounding factors. Model 1 was adjusted for age, gender, and body mass index, while Model 2 was fully adjusted for a set of variables including age, gender, body mass index, smoking history, alcohol history, hypertension history, cardiovascular disease (CVD) history, diabetes history, time interval between thyroid surgery and RAI treatment, I-131 dose, tumor location, maximum tumor diameter, extrathyroidal extension, multifocality, number and location of lymph node metastases, presTg levels, Rx-WBS results, TNM staging, AJCC staging, and ATA risk stratification for recurrence. Variables with a variance inflation factor (VIF) >5 were removed from the model to prevent multicollinearity, and the results were reported in terms of odds ratios (OR) along with corresponding 95% confidence intervals (CI). Receiver operating characteristic (ROC) curves were plotted, and Bootstrap resampling (500 iterations) was used to calculate the area under the curve (AUC) with a 95% CI to analyze the predictive value of SII and SIRI for the response to RAI treatment. The maximum value of the Youden index was used to determine the sensitivity and specificity of the predictive factors. P-value <0.05 was considered statistically significant.
Results
Clinical Characteristics
A comparison was made between 146 patients in the non-ER group and 260 patients in the ER group. Table 1 presents the differences in baseline data between the two groups of patients. Compared to the ER group, the non-ER group showed statistically significant differences in terms of gender, extrathyroidal extension, number and location of lymph node metastases, AJCC stage, ATA risk stratification, RAI dose, Rx-WBS results, tumor size, presTg levels, neutrophils, lymphocytes, SII, and SIRI. The SII and SIRI values in the non-ER group were significantly elevated (Figure 2). However, no significant differences were observed between the two groups in terms of platelet count and monocyte count (p>0.05).
 |
Table 1 Comparison of Baseline Data Between the ER and Non-ER Groups |
 |
Figure 2 Violin plots of SII (A) and SIRI (B) in the ER and non-ER groups. |
Association of SII and SIRI with RAI Treatment Response
In the unadjusted model, compared to the SII Q1 group as the reference, the risk of suboptimal response to radioactive iodine treatment was nearly 1.52 times higher in the Q2 group (OR=2.52; 95% CI: 1.42–4.46; p=0.002) and 5.36 times higher in the Q3 group (OR=6.36; 95% CI: 3.62–11.15; p<0.001); compared to the SIRI Q1 group, the risk of poor response to radioactive iodine treatment was nearly 3.01 times higher in the Q2 group (OR=4.01; 95% CI: 2.29–7.04; p<0.001) and 3.08 times higher in the Q3 group (OR=4.08; 95% CI: 2.33–7.15; p<0.001). In models 1 and 2, after adjusting for potential confounding factors, the association between SII, SIRI, and the response to radioactive iodine treatment remained significant, as shown in Table 2.
 |
Table 2 Association of SII, SIRI and RAI Treatment Response |
Predictive Value of SII and SIRI for RAI Treatment Response
For predicting the response to initial RAI treatment, the ROC curve results (Figure 3 and Table 3) showed that the AUC for SII was 0.692 (95% CI: 0.639–0.745, P < 0.001), with a sensitivity of 58.2% and specificity of 73.1%, and the optimal cutoff value was 668.91. The AUC for SIRI was 0.664 (95% CI: 0.612–0.717, P < 0.001), with a sensitivity of 85.6% and specificity of 42.7%, and the optimal cutoff value was 0.47.
 |
Table 3 ROC Analysis Showed the Value of SII and SIRI in Predicting the Response to Radioactive Iodine Therapy |
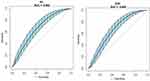 |
Figure 3 Receiver Operating Characteristic (ROC) Curves for SII and SIRI. |
Discussion
This study analyzed the role of SII and SIRI in predicting the response to initial RAI treatment in patients with DTC. The results of the study showed that compared to the ER group, the SII and SIRI values were significantly elevated in the non-ER group (p < 0.001). After adjusting for covariates, the association between SII, SIRI, and the response to RAI treatment remained significant. ROC curve analysis revealed that the AUC for SII was 0.692 (95% CI: 0.639–0.745, P < 0.001) with an optimal cutoff value of 668.91; the AUC for SIRI was 0.664 (95% CI: 0.612–0.717, P < 0.001) with an optimal cutoff value of 0.47. Compared to SIRI, SII is more effective in identifying patients who may have an adverse prognosis. The above results indicate that high levels of SII and SIRI indicate immune-inflammatory stimulation in patients with DTC, suggesting that before the initial iodine treatment, we should pay close attention to improving the tumor microenvironment of DTC patients.
As research in the field of cancer treatment advances, scholars increasingly recognize the ongoing, dynamic interaction between the tumor microenvironment and the biological behavior of cancer cells, as well as their response to treatment methods. An increasing number of studies suggest that immune-inflammatory cells in the tumor microenvironment can influence the functionality of DTC cells and the effectiveness of RAI treatment.4,25 The involved mechanism may be that activated immune cells in the TME stimulate tumor cells and stromal cells to release pro-inflammatory chemokines, activating the inflammatory pathways to promote the activation of cancer-associated fibroblasts (CAFs), leading to the deposition and remodeling of the extracellular matrix (ECM). At the same time, the secretion of factors such as interleukin-6 (IL-6), interleukin-1 beta (IL-1β), vascular endothelial growth factor (VEGF), colony-stimulating factor 1 (CSF-1), C-C motif chemokine ligand 2 (CCL2), etc., promotes the accumulation of regulatory T cells (Tregs) and immune suppression, thereby driving increased resistance to RAI.20,26–28 Given the complexity of the response process to RAI therapy, further in-depth research is still needed to elucidate the specific mechanisms by which immune-inflammatory cells participate in the response to RAI treatment. This will provide new therapeutic insights for patients with unsatisfactory response to RAI therapy.
SII and SIRI, as two novel inflammation markers composed of three subtypes of platelets and leukocytes, do not solely rely on changes in a single cell type. They can more comprehensively reflect the balance of host inflammation and immune status.29 Italian scholars compared the SII values of 93 DTC patients with those of 33 healthy individuals and found that the SII of DTC patients was higher compared to the healthy population (p=0.000).30 Zhao et al analyzed the clinical data of 702 papillary thyroid carcinoma (PTC) patients and found that SII is an independent predictor of lateral lymph node metastasis in PTC.31 In Pang et al’s study, machine learning models were used to complement the predictive role of SIRI for central lymph node metastasis in PTC.32 The above studies have different limitations, including small sample sizes, the clinical applicability of predictive models needing further investigation, and only investigating the relationship between SII, SIRI, and the prognosis of DTC surgical treatment. As is well known, prognostic studies of DTC involve three stages: surgical treatment, RAI treatment, and TSH suppression therapy.9 In addition, existing studies have shown that presTg levels, TSH levels and intestinal microbiota have predictive value for the prognosis of RAI treatment.33–35 However, there is currently no literature evaluating the predictive efficacy of RAI treatment response using convenient peripheral blood parameters. Therefore, compared to other studies, this research reveals the roles of SII and SIRI in predicting the prognosis of initial RAI treatment, providing a valuable complement to current research on DTC and inflammatory markers. Moreover, our study identified the potential of SII and SIRI in early identification of unsatisfactory RAI treatment response. As cost-effective and convenient inflammatory markers, they possess certain clinical utility.
Furthermore, we observed gender differences in the response of DTC patients to RAI treatment. Despite the higher incidence of DTC in female patients,36 they exhibit a more favorable response to RAI treatment, consistent with previous research findings.37 A large multicenter retrospective cohort study in Korea revealed that female gender was a significant predictor of ER (p<0.001).22 Unfortunately, the specific mechanisms underlying gender differences have not been clarified. Future studies could be designed to investigate through which pathways gender differences specifically influence the response to RAI treatment. Additionally, studies have reported that butyrylcholinesterase (BChE) may serve as a potential biomarker for thyroid cancer,38 and its role in immune regulation and inflammatory response has been well-established.39–41 Therefore, investigating the relationship between BChE levels and the response to RAI therapy may represent an intriguing direction for future research.
Our work still has some limitations. Firstly, this study only included baseline values of SII and SIRI, their dynamic changes may provide better prognostic value. Secondly, although patients with diseases that could affect peripheral blood inflammatory indices were excluded, peripheral blood parameters may still be influenced by other factors, leading to some variability and instability. Therefore, forthcoming investigations should prioritize the implementation of multicenter, large-sample, prospective cohort studies or randomized controlled trials to enhance the completeness, accuracy, reliability, and generalizability of the data. Finally, it is important to note that cytological examination can reveal pathological features of immune-inflammatory responses. Future research could explore whether thyroid cytological assessments, such as the Bethesda classification system, provide additional insights into predicting patient response to RAI therapy.
Conclusion
The results of this study suggest that SII and SIRI could be valuable for predicting the response to RAI therapy in individuals diagnosed with differentiated thyroid cancer. They may serve as auxiliary tools for monitoring the patient’s status. In clinical practice, promptly monitor patients displaying abnormal inflammatory markers and implement targeted measures. Compared to SIRI, SII may be more effective in identifying patients who may have an unfavorable prognosis. Further research is needed to assess their clinical utility.
Data Sharing Statement
The datasets generated and/or analyzed during the study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This study adhered to the principles of the Helsinki Declaration and was approved by the Ethics Committee of the First Hospital of Shanxi Medical University (No. KYLL-2024-110). Given the retrospective nature of the study and the confidential handling of all patient data, the Ethics Committee of the First Hospital of Shanxi Medical University waived the requirement for informed consent.
Funding
A project grant from the Shanxi Provincial Science and Technology Department Science and Technology Strategy Research Project (Grant No. 202204031401144) supported this work.
Disclosure
Yan Wang is the first author. The authors declare that they have no financial or conflicts of interest.
References
1. Chen DW, Lang BHH, McLeod DSA, Newbold K, Haymart MR. Thyroid cancer. Lancet. 2023;401(10387):1531–1544. doi:10.1016/S0140-6736(23)00020-X
2. Miranda-Filho A, Lortet-Tieulent J, Bray F, et al. Thyroid cancer incidence trends by histology in 25 countries: a population-based study. Lancet Diabetes Endocrinol. 2021;9(4):225–234. doi:10.1016/S2213-8587(21)00027-9
3. Pizzato M, Li M, Vignat J, et al. The epidemiological landscape of thyroid cancer worldwide: GLOBOCAN estimates for incidence and mortality rates in 2020. Lancet Diabetes Endocrinol. 2022;10(4):264–272. doi:10.1016/S2213-8587(22)00035-3
4. Liu Y, Wang J, Hu X, et al. Radioiodine therapy in advanced differentiated thyroid cancer: resistance and overcoming strategy. Drug Resist Updat. 2023;68:100939. doi:10.1016/j.drup.2023.100939
5. Pacini F, Fuhrer D, Elisei R, et al. 2022 ETA consensus statement: what are the indications for post-surgical radioiodine therapy in differentiated thyroid cancer? Eur Thyroid J. 2022;11(1). doi:10.1530/ETJ-21-0046
6. Wilhelm A, Conroy PC, Calthorpe L, et al. Disease-specific survival trends for patients presenting with differentiated thyroid cancer and distant metastases in the United States, 1992–2018. Thyroid. 2023;33(1):63–73. doi:10.1089/thy.2022.0353
7. Sparano C, Moog S, Hadoux J, et al. Strategies for radioiodine treatment: what’s new. Cancers. 2022;14(15). doi:10.3390/cancers14153800
8. Valerio L, Maino F, Castagna MG, Pacini F. Radioiodine therapy in the different stages of differentiated thyroid cancer. Best Pract Res Clin Endocrinol Metab. 2023;37(1):101703. doi:10.1016/j.beem.2022.101703
9. Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133. doi:10.1089/thy.2015.0020
10. Liu H, Yang D, Li L, Tu Y, Chen C, Sun S. Appraisal of radioiodine refractory thyroid cancer: advances and challenges. Am J Cancer Res. 2020;10(7):1923–1936.
11. Taprogge J, Abreu C, Yusuf S, et al. The role of pretherapy quantitative imaging and dosimetry in radioiodine therapy for advanced thyroid cancer. J Nucl Med. 2023;64(7):1125–1130. doi:10.2967/jnumed.122.264913
12. Song HJ, Qiu ZL, Shen CT, Wei WJ, Luo QY. Pulmonary metastases in differentiated thyroid cancer: efficacy of radioiodine therapy and prognostic factors. Eur J Endocrinol. 2015;173(3):399–408. doi:10.1530/EJE-15-0296
13. Ullmann TM, Papaleontiou M, Sosa JA. Current controversies in low-risk differentiated thyroid cancer: reducing overtreatment in an era of overdiagnosis. J Clin Endocrinol Metab. 2023;108(2):271–280. doi:10.1210/clinem/dgac646
14. Ming H, Yu H, Liu Y, Yang L, Chen Y. Effect of radioiodine therapy under thyroid hormone withdrawal on health-related quality of life in patients with differentiated thyroid cancer. Jpn J Clin Oncol. 2022;52(10):1159–1166. doi:10.1093/jjco/hyac113
15. Helvaci BC, Yalcin MM, Yalcin SNG, Arslan E, Altinova AE, Toruner FB. Differentiated thyroid cancer: effect on quality of life, depression, and anxiety. Hormones. 2023;22(3):367–374. doi:10.1007/s42000-023-00449-3
16. Chen JH, Zhai ET, Yuan YJ, et al. Systemic immune-inflammation index for predicting prognosis of colorectal cancer. World J Gastroenterol. 2017;23(34):6261–6272. doi:10.3748/wjg.v23.i34.6261
17. Ravindranathan D, Master VA, Bilen MA. Inflammatory markers in cancer immunotherapy. Biology. 2021;10(4). doi:10.3390/biology10040325
18. Jin Z, Wu Q, Chen S, et al. The associations of two novel inflammation indexes, SII and SIRI with the risks for cardiovascular diseases and all-cause mortality: a ten-year follow-up study in 85,154 individuals. J Inflamm Res. 2021;14:131–140. doi:10.2147/JIR.S283835
19. Galdiero MR, Varricchi G, Marone G. The immune network in thyroid cancer. Oncoimmunology. 2016;5(6):e1168556. doi:10.1080/2162402X.2016.1168556
20. Ferrari SM, Fallahi P, Galdiero MR, et al. Immune and inflammatory cells in thyroid cancer microenvironment. Int J Mol Sci. 2019;20(18). doi:10.3390/ijms20184413
21. Schlumberger M, Leboulleux S. Current practice in patients with differentiated thyroid cancer. Nat Rev Endocrinol. 2021;17(3):176–188. doi:10.1038/s41574-020-00448-z
22. Kwon SY, Lee SW, Kong EJ, et al. Clinicopathologic risk factors of radioactive iodine therapy based on response assessment in patients with differentiated thyroid cancer: a multicenter retrospective cohort study. Eur J Nucl Med Mol Imaging. 2020;47(3):561–571. doi:10.1007/s00259-019-04634-8
23. Cheng F, Xiao J, Huang F, et al. Delay of initial radioactive iodine therapy beyond 3 months has no effect on clinical responses and overall survival in patients with thyroid carcinoma: a cohort study and a meta-analysis. Cancer Med. 2022;11(12):2386–2396. doi:10.1002/cam4.4607
24. Underwood HJ, Patel KN. Comparing the 7th and 8th editions of the American joint committee on cancer staging systems for differentiated thyroid cancer: improvements observed and future horizons. Ann Surg Oncol. 2019;26(9):2653–2654. doi:10.1245/s10434-019-07490-w
25. Hamidi S, Hofmann MC, Iyer PC, et al. Review article: new treatments for advanced differentiated thyroid cancers and potential mechanisms of drug resistance. Front Endocrinol. 2023;14:1176731. doi:10.3389/fendo.2023.1176731
26. Valkenburg KC, de Groot AE, Pienta KJ. Targeting the tumour stroma to improve cancer therapy. Nat Rev Clin Oncol. 2018;15(6):366–381. doi:10.1038/s41571-018-0007-1
27. Peczek P, Gajda M, Rutkowski K, Fudalej M, Deptala A, Badowska-Kozakiewicz AM. Cancer-associated inflammation: pathophysiology and clinical significance. J Cancer Res Clin Oncol. 2023;149(6):2657–2672. doi:10.1007/s00432-022-04399-y
28. Pu W, Shi X, Yu P, et al. Single-cell transcriptomic analysis of the tumor ecosystems underlying initiation and progression of papillary thyroid carcinoma. Nat Commun. 2021;12(1):6058. doi:10.1038/s41467-021-26343-3
29. Huang P, Mai Y, Zhao J, Yi Y, Wen Y. Association of systemic immune-inflammation index and systemic inflammation response index with chronic kidney disease: observational study of 40,937 adults. Inflamm Res. 2024;73(4):655–667. doi:10.1007/s00011-024-01861-0
30. Kars A, Sahin A, Kilic K, Sakat MS, Bilen A. Systemic immune inflammation index in differentiated thyroid cancers. Acta Otorhinolaryngol Ital. 2022;42(2):150–154. doi:10.14639/0392-100X-N1665
31. Zhao L, Zhou T, Zhang W, et al. Blood immune indexes can predict lateral lymph node metastasis of thyroid papillary carcinoma. Front Endocrinol. 2022;13:995630. doi:10.3389/fendo.2022.995630
32. Pang J, Yang M, Li J, et al. Interpretable machine learning model based on the systemic inflammation response index and ultrasound features can predict central lymph node metastasis in cN0T1-T2 papillary thyroid carcinoma. Gland Surg. 2023;12(11):1485–1499. doi:10.21037/gs-23-349
33. Ju Y, Wang L, Cheng F, et al. Comparing the efficacy of thyroglobulin and thyroglobulin/ thyroid-stimulating hormone ratio models in predicting a successful response to radioactive iodine therapy. BMC Endocr Disord. 2023;23(1):19. doi:10.1186/s12902-022-01261-7
34. Yang X, Liang J, Li T, Zhao T, Lin Y. Preablative stimulated thyroglobulin correlates to new therapy response system in differentiated thyroid cancer. J Clin Endocrinol Metab. 2016;101(3):1307–1313. doi:10.1210/jc.2015-4016
35. Zheng L, Zhang L, Tang L, et al. Gut microbiota is associated with response to (131)I therapy in patients with papillary thyroid carcinoma. Eur J Nucl Med Mol Imaging. 2023;50(5):1453–1465. doi:10.1007/s00259-022-06072-5
36. Shobab L, Burman KD, Wartofsky L. Sex differences in differentiated thyroid cancer. Thyroid. 2022;32(3):224–235. doi:10.1089/thy.2021.0361
37. Faro FN, Bezerra A, Scalissi NM, et al. Intermediate-risk thyroid carcinoma: indicators of a poor prognosis. Arch Endocrinol Metab. 2021;64(6):764–771. doi:10.20945/2359-3997000000290
38. Kang W, Ma M, Xu L, et al. Customized fluorescent probe for peering into the expression of butyrylcholinesterase in thyroid cancer. Anal Chim Acta. 2023;1282:341932. doi:10.1016/j.aca.2023.341932
39. Verras GI, Mulita F. Butyrylcholinesterase levels correlate with surgical site infection risk and severity after colorectal surgery: a prospective single-center study. Front Surg. 2024;11:1379410. doi:10.3389/fsurg.2024.1379410
40. Zivkovic AR, Bender J, Brenner T, Hofer S, Schmidt K. Reduced butyrylcholinesterase activity is an early indicator of trauma-induced acute systemic inflammatory response. J Inflamm Res. 2016;9:221–230. doi:10.2147/JIR.S117590
41. Kinchen JM, Mohney RP, Pappan KL. Long-chain acylcholines link butyrylcholinesterase to regulation of non-neuronal cholinergic signaling. J Proteome Res. 2022;21(3):599–611. doi:10.1021/acs.jproteome.1c00538
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

