Back to Journals » Clinical Ophthalmology » Volume 18
Telemedicine at a University Ophthalmology Practice During the Beginning of the COVID-19 Pandemic
Authors Oganov AC, Chou TY , Hanson PM, Abazari A, Kung P, Weissbart SB, Lenoci JN, Honkanen RA
Received 4 March 2024
Accepted for publication 7 August 2024
Published 23 August 2024 Volume 2024:18 Pages 2369—2380
DOI https://doi.org/10.2147/OPTH.S460454
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
Anthony C Oganov, Timothy Y Chou, Paris M Hanson, Azin Abazari, Preston Kung, Sarah B Weissbart, Jacqueline N Lenoci, Robert A Honkanen
Department of Ophthalmology, Renaissance School of Medicine, Stony Brook University, Stony Brook, NY, 11974, USA
Correspondence: Timothy Y Chou, Department of Ophthalmology, Renaissance School of Medicine, Stony Brook University, HSC L2, Rm 152, Stony Brook, NY, 11974, USA, Tel +1 631444-1131, Fax +631444-4089, Email [email protected]
Purpose: The aim of the research was to evaluate the use of teleophthalmology at a university practice during the COVID-19 pandemic, specifically examining precision, effectiveness, and patient satisfaction.
Patients and Methods: Telemedicine visits were offered to new and established patients requesting appointments with the Stony Brook University Department of Ophthalmology between March 30 and June 2, 2020. Records from these visits were reviewed for chief complaint, past medical and ocular history, diagnoses, treatment/management, and providers’ sub-specialty. Precision was determined by comparing agreement between diagnoses of the telemedicine visit with those of the subsequent in-person visit. The decision to follow up in person was made by the physician and patient. Diagnostic precision as well as progression, improvement, or stability of patients’ symptoms were determined by the physician’s assessment at follow-up visits. Post-telemedicine visit satisfaction surveys were sent to all patients.
Results: Telemedicine visits were offered to 783 patients, 520 (66.4%) of whom accepted. Of these 520 patients, 409 (78.7%) were established and 105 (20.2%) had in-person, follow-up visits. Overall, the diagnostic precision of the follow-up visits was 89.5%. Precision differed significantly across ophthalmologic subspecialties. Of the patients who had in-person follow-up visits, 56.8% remained stable, 32.4% improved, and 10.8% worsened. Established patients presented with more extensive ocular histories/procedures and experienced a higher percentage of worsening symptoms/disease stage compared to new patients. Oculoplastics/orbit was the most prevalent diagnostic subspecialty that worsened. Surveys were sent to all patients completing telemedicine visits, 15.0% of whom responded. Overall satisfaction was 91.9%, although only 23.0% of respondents preferred telemedicine to an in-office visit.
Conclusion: Telehealth provides high levels of precision and patient satisfaction for a wide range of ophthalmologic visits, although most patients still prefer in-office examinations. Employing teleophthalmology for follow-up and emergency care may provide patients with an effective alternative during pandemic situations and beyond.
Plain Language Summary: Telemedicine involves integration of modern telecommunications technology into medical practice. Over the years, it has demonstrated greater and more widespread utility for different medical specialties, including ophthalmology.
As a response to the recent COVID-19 pandemic, the Stony Brook University Department of Ophthalmology provided an option of telemedicine for patients in lieu of in-person eye examinations. In this paper, Stony Brook ophthalmologists report on their experience with teleophthalmology, particularly regarding its utilization, accuracy, effectiveness, precision, and acceptability. The authors examined the records of 520 patients who had telemedicine encounters between March 30 and June 2, 2020. Precision was determined by comparing the initial and final diagnoses of all patients who had an in-person follow-up appointment following a telemedicine visit. Of 105 patients that followed up, precision was determined to be 89.5%. Precision was compared across ophthalmologic subspecialties and found to be statistically similar (p> 0.05). Approximately a third of patients improved, while nearly 11% worsened. Established and oculoplastics patients were more significantly likely to worsen. Surverys were sent out to study patients to gauge their satisfaction with their telemedicine experience. Although satisfaction was nearly 92%, only 23% of patients preferred telemedicine to an in-person physician encounter. The authors conclude that teleophthalmology provides a high level of diagnostic precision and patient satisfaction; nevertheless, most patients prefer in-person physician encounters. Telemedicine may provide an effective alternative to in-person ophthalmology assessments, especially during a pandemic. There appears to be a lesser but potentially useful role for teleophthalmology in a non-pandemic setting.
Keywords: Teleophthalmology, teleglaucoma, teleretina, telehealth, coronavirus
A Letter to the Editor has been published for this article.
Introduction
Since its emergence in the 1950s, telemedicine has proven to be a useful tool in fields such as radiology, psychiatry, and dermatology by expanding access to care while still maintaining diagnostic accuracy, yet at the same time reducing hospital stays and medical center costs.1,2 One survey of 292 administrators and clinicians across 71 hospitals found that 95% agreed and 61% strongly agreed with the statement that “tele[medicine] improves the quality of care at my facility”.3
The current state of telemedicine in ophthalmology, known as teleophthalmology, is characterized by rapid growth and increasing integration into clinical practice. Teleophthalmology employs methods such as “store and forward”, where patient data and images are collected and reviewed by specialists at a later time, as well as live video consultations.2 These approaches are particularly beneficial for screening and monitoring conditions like diabetic retinopathy,4,5 age-related macular degeneration,6 and glaucoma,7 enabling earlier detection and ongoing management. Patients benefit from reduced travel burdens and increased access to care, especially in remote or underserved areas.8 Tele-ophthalmology is already used in a variety of healthcare settings in the United States including the Veteran’s Health Administration9 and Indian Health Service.10 However, challenges remain, and certain diagnostic procedures still require in-person visits to ensure accuracy.11 Further, certain patient populations such as the elderly face barriers to the use of telemedicine such as challenges and literacy difficulties.12
Starting December 2019, the novel SARS-CoV-2 beta coronavirus spread exponentially, launching the global COVID-19 pandemic and requiring rapid adaptation from our healthcare systems. In March 2020, the American Academy of Ophthalmology subsequently recommended the termination of all elective procedures and routine office visits, excluding urgent or emergency cases.13 The Department of Ophthalmology at Stony Brook University began utilizing telemedicine to provide access to medical care across Long Island in New York. Telemedicine appointments were offered in lieu of in-office visits at the discretion of the ophthalmology attendings. Further, regulatory changes during this time reduced physician liability and allowed for reimbursement of telemedicine visits.
Beyond the pandemic, teleophthalmology promises to transform healthcare delivery by improving access to specialist care, reducing costs, and maintaining continuity of care, thus highlighting its long-term potential in the healthcare landscape.5,14 Technological advancements, including high-resolution imaging devices and AI-driven diagnostic tools, have further enhanced the effectiveness of teleophthalmology.15–17
In this paper, we examine the utilization and precision of teleophthalmology during the COVID-19 pandemic as well as patient satisfaction with this modality of healthcare. Using the data from this unique timeframe, we hope to provide a study of the effectiveness and appropriateness of teleophthalmology to diagnose and treat a variety of ocular conditions.
Materials and Methods
Design of the Study
This is a retrospective, cross sectional, single-institution records review of patients who received ophthalmologic care at Stony Brook University Hospital (SBUH) and affiliated sites as well as a satisfaction survey of the patients seen virtually.
Ethics Approval
This study was approved as a Departmental Quality Assurance (QA) project and complied with the policies of SUNY Stony Brook Committee on Research Involving Humans. The Stony Brook University Institutional Review Board and Ethics Committee ruled that IRB approval and patient consent were not required for this study given its designation as a QA project. The described research adhered to the tenets of the Declaration of Helsinki and patient confidentiality and privacy were strictly maintained throughout the research process.
Participants
The SBUH electronic medical records (EMR) for all telemedicine visits that occurred between March 30th and June 2nd, 2020, were examined. This timeframe was chosen as it included a period of four weeks in which university policy prohibited in-person elective ophthalmology visits. Patients were tracked until four weeks after this time to allow for adequate follow-up. All patients who successfully scheduled and completed a telemedicine appointment with a board-certified ophthalmologist within this time period were included, and patients who cancelled, did not show up for, or rescheduled their appointments outside of the study window were excluded. Pediatric patients under 18, whose parents accompanied them to both telemedicine and in-person follow-up visits, were also included. A total of 520 patients who had telemedicine encounters during this time and that met these parameters were identified.
Telemedicine Procedure
All patients that had an appointment during the peak of the pandemic in our region were offered a telemedicine appointment. As patients were not allowed in the clinic for non-emergent reasons per university policy, in-person office visits were made at the discretion of the physician. We would note that telemedicine visits had not been offered at our institution before the pandemic. Both patients and providers utilized computers or mobile devices with video and audio capability. Telemedicine visits were conducted using the Microsoft Teams application (1.3.00.4461). After scheduling a visit, both the provider and the patient received an Email with a link to join the visit. On the day of the appointment, and prior to the scheduled visit, an ophthalmic technician contacted the patient. The technician recorded the patient’s chief complaint, history of present illness, past medical/surgical/ocular history, allergies, and list of current medications. The physician contacted the patient by joining the Microsoft Teams meeting at the scheduled time. The provider conducted the remote eye examination by first sharing the screen and then using the Eye Handbook application (Cloud Nine Development, LLC). Assessment included testing the patient for near and color vision, and with the Amsler grid (when applicable). Actual physical evaluation of the eye was conducted by the patient holding their eye or both eyes close to their video screen, and the examiner then viewing their own screen, and recording their findings. The duration of each telemedicine visit was recorded in the EMR.
Measures and Statistical Analysis
Patient electronic medical records were reviewed, and the following information was tabulated: age, sex, whether the patient was new or established, type of visit (routine, follow-up, urgent, non-urgent), duration of appointment, past medical history, past ocular history, and past ocular surgeries. A new patient was defined as one without any previous completed appointments (virtual or in-person) at the practice, while an established patient had documentation of at least one completed appointment. An urgent visit was defined as a telemedicine visit that was scheduled on the same day as the visit for an acute complaint. A non-urgent visit was defined as all other telemedicine visits that were not defined as urgent, including routine and post-operative visits. A routine visit was defined as a telemedicine visit without a specific chief complaint. A follow-up visit was defined as an in-person appointment after the telemedicine visit for the purpose of confirming the telemedicine diagnosis as well as assessing the status of the patient’s chief complaint (improving, stable, worsening). The duration of each appointment was determined by the total length of time the patient spent on the Microsoft Teams video chat with the attending physician.
The mean number of prior diagnoses, procedures, and surgeries listed was used to determine how extensive the ocular and procedural history was for each patient. A chi-squared test was then applied to determine whether new or established patients had comparatively more documented (thus “more extensive” as an estimate of severity) past ocular procedures and diagnoses. By extension, patients that had comparatively less documented ocular procedures and diagnoses were described as having “less extensive” histories.
The chief complaint, diagnoses, management plans, and whether the patient was subsequently seen in person for follow-up were recorded. Based on the primary complaint, visits were grouped into the following categories: refractive error, cornea and external disease, cataract, glaucoma, oculoplastic and orbit, pediatric, neuro-ophthalmology, retina, uveitis, or high-risk medication monitoring. Treatments for the patient’s chief complaint without medical intervention – such as observation, lid hygiene, and artificial tears – were considered “conservative” management, while treatments with medication were considered “complex”. By evaluating the exam findings, ancillary tests, and the patient’s subjective opinion, the attending ophthalmologist determined whether symptoms or disease stage had overall improved, remained stable, or worsened since the preceding telemedicine visit. This outcome was determined with respect to the patient’s chief complaint and not to other patient history. For example, if a patient presented for dry eye but had concurrent glaucoma, then only dry eye was documented as improving, remaining stable, or worsening.
All patients who had a telemedicine visit were offered an in-person follow-up. We confirmed that the same attending who saw the patient during their telemedicine visit also saw them during their in-person follow-up visit; therefore, no patients were excluded from the analysis on this basis.
In cases where the patient had an in-office follow-up visit, the precision of the telemedicine visit was determined. The newly-made diagnoses from the telemedicine visit were compared to those from the ensuing in-office visit. When the new diagnoses on both visits were the same, the telemedicine visit was defined as diagnostically “precise”. Precision for established patient who already had diagnoses was determined based on comparison of newly made diagnoses between the two visits. Visits that were not precise were further divided into one group with only a single diagnostic difference, and another group with more than one different diagnosis. Precision of diagnosis was determined overall, as well as separately by subspecialty: glaucoma, comprehensive/cornea/external, oculoplastics/orbit, pediatrics, and retina.
Results were reported with sample sizes and proportions for all categorical variables. Mean and standard deviation (SD) were calculated for all demographic data involving continuous variables. Chi square analysis was used to determine the significance of differences in diagnostic precision, across specialties. Student’s t-test was used to compare all means. All continuous data was normally distributed. All statistical analysis and results were analyzed and compiled using Python 3.8.2 (Python Software Foundation). Data was collected and checked by three independent researchers and the analysis was validated using two independent coding methodologies in Python to ensure reliability.
Survey
To assess patient satisfaction, a post telemedicine visit survey was sent to patients using the SurveyMonkey web application (SurveyMonkey, San Mateo, CA, USA; http://www.surveymonkey.com). The survey was self-created, unvalidated, and included 6 prompts: “It was easy to schedule my telemedicine appointment”; “I found telemedicine easy to use”; “Telemedicine adequately addressed my problem or condition”; “I am satisfied with the care I received during my telemedicine visit”; “I would participate in another telemedicine visit in the future”; “I prefer a telemedicine visit to an in-office visit”. All questions were measured on a 5-point Likert scale with the following possible responses: “Strongly Disagree”, “Disagree”, “Neutral”, “Agree”, and “Strongly Agree”. Patients were required to answer all multiple-choice questions to submit the survey. An optional “patient comment” section was included at the end of the survey. Responses from the survey were linked to their respective telemedicine visits.
Results
Telemedicine visits were offered to 783 patients, 520 (66.4%) of whom accepted (Table 1). Of these 520 study patients, 409 (78.7%) were established with the practice. One hundred five (20.2%) of the study patients, 78 (74.3%) of whom were established, had subsequent in-person follow-up visits. Among established patients, 14 (3.4%) of visits were for postoperative care.
 |
Table 1 Telemedicine Visit Details |
Approximately 1700 different diagnoses were recorded and organized into 12 major categories. The percentage of visits from each category was calculated (Figure 1). The mean age of all patients was 34.9±30.1 years. There was no significant age difference between patients who accepted or declined their telemedicine offers (p>0.05). This held true even after excluding pediatric patients (age <18), whose parents made attendance decisions on their behalf (p>0.05).
 |
Figure 1 Diagnoses made or confirmed via telemedicine visit divided by ophthalmologic specialty (N=1710 diagnoses). |
Of the telemedicine encounters where there was also an in-person, follow-up visit, the diagnostic precision was 89.5%. A majority (92.0%) of the remaining, in-person follow-up visits differed from their original telemedicine visits by only a single diagnosis. The mean duration of all telemedicine visits was 28.0±10.0 minutes. The duration of a telemedicine visit had no bearing on the precision of its diagnoses (p>0.05). Diagnoses given to new patients tended to have a higher precision (93.5%) than that of established patients (88.6%), but this difference was not statistically significant (p>0.05). When we looked at whether subspecialty factored diagnostic precision, diagnoses for telemedicine and subsequent in-person visits agreed 100% (N=25) of the time for pediatrics, 94.1% (N=36) for glaucoma, 89.5% (N=19) for oculoplastics/orbit, 80.8% (N=26) for comprehensive/cornea/external, and 60% (N=5) for retina. The difference in diagnostic precision across all subspecialty groupings was found to be statistically significant in a chi-square analysis (p<0.05; Table 2). Oculoplastics/orbit was the most prevalent subspecialty represented among those following up (66/105, or 62.9%) (p<0.05).
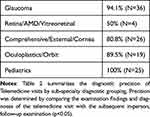 |
Table 2 Precision of Diagnosis by Diagnostic Grouping |
Disease stage improved in 34 (32.4%) of the 105 patients who had in-office follow-up visits, remained stable in 60 (56.8%), and worsened in 11 (10.8%). Five of the 11 patients that worsened were oculoplastics/orbit patients, a proportion that was statistically higher than the other subspecialties (p<0.05) None of the oculoplastics/orbit patients that worsened experienced an actual emergency, though one patient ended up requiring a procedure for bilateral epiphora. Of the 77 established patients with an in-person follow-up, 28 (36.4%), 40 (51.9%), and 9 (11.7%) improved, remained stable, and worsened, respectively. Of the 28 new patients with an in-person follow-up visit 7 (25.0%), 21 (75.0%), and 0 (0.0%) patients improved, remained stable, and worsened, respectively. Established patients were significantly more likely to suffer worsening of their symptoms or disease stage compared to new patients (p<0.05).
Urgent telemedicine visits were completed for 17 patients who also had in-office follow-up. Seven (41.2%), 9 (52.9%), and 1 (5.9%) of these patients improved, remained stable, and worsened, respectively. Eighty-eight non-urgent patients also had in-person follow-ups, of which 29 (33.0%) improved, 51 (58.0%) remained stable, and 8 (9.0%) worsened. There was no significant difference in progression of disease stage or symptoms between urgent and non-urgent patients (p>0.05).
Figure 2 presents the chief complaints, ocular history, ocular procedural history, and management for all telemedicine visits. These were compared based on patient type (new vs established), degree of urgency, and whether or not the patient followed up in person. Established patients typically utilized telemedicine for routine visits (74.9%). However, most of these established patients (81.2%) were not subsequently seen in person for follow-up throughout the duration of the study. Ocular history differed significantly between established vs new patients (p<0.05), patients with follow-up vs those without (p<0.05), and urgent vs non-urgent patients, respectively (p<0.05). However, none of these groups differed in ocular surgical history (p>0.05). All patient groups, including established vs new, follow-up vs not, and urgent vs non-urgent differed significantly in their chief complaints (p>0.05). Finally, established vs new patients (p<0.05) and urgent vs non-urgent patients (p<0.05) had significantly different management, while patients with follow-up and those without did not (p>0.05).
 |
Figure 2 Normalized ocular history (Top Left), ocular procedures (Top Right), reasons for visit (Bottom Left), and management (Bottom Right) for all patients (blue, N=520), established patients (black, N=409), new patients (Orange, N=111), patients with urgent visits (green, N= 48), patients with non-urgent visits (purple, N=472), patients with in-person follow up by June 2nd, 2020 (gray, N=105), and patients without an in-person follow up by June 2nd, 2020 (red, N=415). Groups that were compared statistically are established vs new patients, patients with follow up vs those without, and emergency visits vs non-emergency visit, and p-values are included in the legend. A Student’s t-test was used for all comparisons and Table 4 denotes all statistical comparisons. *Full variable was ”Routine Visit, Pediatric Exams, and Strabismus”. **Full variable was ”Observation, Conservative Management, Artificial Tears”. |
A satisfaction survey was sent to each patient at the completion of their telemedicine visit (Table 3). Of the 520 study patients, 78 (15.0%) completed the survey. Four of the returned surveys could not be correlated with visit data and were excluded from the analysis. Forty-eight of the 74 patients (64.9%) who completed the questionnaire were female. The mean age of respondents was 50.3±30.3 years. The mean duration of telemedicine visits for survey patients was 27.8±10.2 minutes. Patients who completed the survey were preponderantly established patients (85.1%). The majority of patients who responded to the survey were seen by comprehensive/cornea providers (32.4%) and pediatric (28.4%) specialists. Curiously, only one retina patient (1.4%) responded. Overall, patients expressed positivity about their teleophthalmology experience. Most respondents considered telemedicine easy to use (83.8%) and were satisfied with the care they received (88.9%). Most patients (85.3%) stated they would participate in another telemedicine visit in the future, but only 23.0% preferred their telemedicine visit to an in-office visit. There were no statistically significant differences between the distribution of responses and patient sex, age, visit type (new, established, post-operative), or subspecialty (p>0.05). However, patients whose telemedicine visits were longer in duration (28.65 vs 21.09 minutes) found telemedicine easier to use (p<0.05) and were more likely to want to participate in another telemedicine visit in the future (p<0.01).
 |
Table 3 Patient Satisfaction Survey Results (n=74) |
 |
Table 4 Statistical Comparisons |
Discussion
In the past few decades, telemedicine has greatly increased its imprint on healthcare. While teleophthalmology had previously been established as a means of consultation and referrals, the COVID-19 pandemic has provided an opportunity to analyze its utility in providing routine, urgent, and postoperative patient care.
To date, several ophthalmology practices have described their approaches to adopting varying degrees of telemedicine.11,18–21 A 2020 study by Kalra et al assessed the implementation of telemedicine during the COVID-19 pandemic, describing the variety of diagnoses and management decisions made remotely.22 In our investigation, we have evaluated the diagnostic precision and patient acceptance of telemedicine across multiple specialties at a single academic institution. Nearly 90% of our telemedicine visits yielded diagnoses that were precise compared with diagnoses made at subsequent in-person follow-up visits. This finding is consistent with previous studies also suggesting a high precision of teleophthalmology.20 We additionally found that telemedicine offers high diagnostic precision relative to in-person visits for both new and established patients, regardless of duration of visit, patient age, or whether or not the visit was urgent.
Our data demonstrate that telemedicine may be a viable option for diagnosis and management of glaucoma and pediatric complaints, as some other studies suggest.4,7,14 Interestingly, although a study by Fydanaki supports that telemedicine may be appropriate for management of oculoplastic complaints,23 we found that oculoplastics/orbit was also the most common subspecialty category in which physicians required an in-person follow-up, as well as the most prevalent subspecialty of patients whose condition worsened. Further, teleophthalmology provided significantly higher precision for pediatric and glaucoma subspecialties than for oculoplastics, comprehensive/cornea/external disease, and retina subspecialties. The cause for relative differences among subspecialties may be related to differences in how thorough of an eye exam an ophthalmology subspecialist could perform via telemedicine. Using our particular type of video technology, examiners were still limited in their ability to elucidate certain exam findings such as intraocular pressure (IOP), corneal pathologies requiring slit lamp or surface stains, aqueous and vitreous cells, and diabetic macular thickening— not to mention ancillary testing or imaging technology. However, certain phenotypes of disease etiologies may be amenable for diagnosis by telemedicine. For example, some studies suggest that as much as 41–70% of patients have blepharitis.24 An important distinction in etiology is blepharitis caused by Demodex Folliculorum infestation, which may be present in as many as 42.1% of patients.25 A panel of experts agree that pathognomonic features such collarettes26 and clinical features such as itching26 are sufficient for diagnosis. It is reasonable to make a diagnosis based on these features via telemedicine. Further, recurrent chalazion27 due to demodex and rosacea-like demodicosis28,29 can similarly be identified using lesional areas30 and clinical characteristics. However, more studies of a similar methodology, namely, telemedicine with in-person follow-up, are needed to determine how precisely these diagnoses may be made and how effectively they may be managed virtually.
Nearly 90% of patients remained stable or improved following their teleophthalmology visits, but a smaller proportion worsened. Those that worsened were significantly more likely to be oculoplastics patients (5 of 11 = 45.5%), but oculoplastics/orbit was also the most prevalent subspecialty condition assessed and treated via teleophthalmology (66/105 = 44%). Ocular conditions for new patients were less likely to worsen than for established patients, but new patients also had the less severe chief complaints and ocular disease histories of the two groups. Because new patients had relatively milder ocular disease than established patients, it might seem logical that their conditions would worsen to a lower degree. At the same time, the decision to offer and initiate telemedicine visits was at the discretion of the attending ophthalmologists, and provider selection biases may have also factored into the results. For example, providers may have preferred to offer telemedicine visits to new patients with less severe chief complaints while being more willing to see established patients with more severe complaints remotely (as they would be more familiar with their relatively more complicated histories). Interestingly, the similarity in disease progression between urgent and non-urgent patients may suggest that teleophthalmology is as appropriate for the management of non-urgent scenarios and requires further study as a viable tool beyond its preconceived utility of triaging and storing forward patient data.31–33
Overall, patient satisfaction with telemedicine was high (91.9%). However, only 23.0% of survey respondents indicated that they preferred telemedicine to an in-office visit. Additional comments provided an explanation that although many patients preferred this form of physician contact in the setting of the pandemic, they would under normal circumstances still prefer to be seen in-person. Our findings contrast with a previous tele-glaucoma study, where patients stated that they preferred telemedicine follow-up visits, citing convenience, travel time, and cost.34 It is likely that telemedicine preferences vary according to how different institutions schedule and carry out virtual visits. We found that patients whose visits were longer in duration (28.7 vs 21.1 minutes) expressed greater approval, regarding telemedicine as easier to use and being more likely to want to participate in a future telemedicine visit. Since greater patient satisfaction can increase patient retention and lower malpractice rates,35 additional time devoted to telemedicine visits might prove highly worthwhile.
We would note that the mean age of our study population of less than 35 years was relatively young compared to the typical age of patients seen in many ophthalmology practices including our own. While patients who accepted or rejected telemedicine appointments did not differ significantly in age, it is also possible that the patients who were not offered such appointments differed in age from those who were. For example, it would be unlikely that patients with wet age-related macular degeneration requiring monthly injections would have been offered remote teleophthalmology visits. By contrast, strabismus was easily the most common diagnosis among the study patients (Figure 1). This could reinforce the idea that a certain proportion of patients, whether new patients with complex issues, or whether due to age and diagnosis, may not have been considered as appropriate for telemedicine as others. Despite the high precision of telemedicine visits, strabismus patients eventually must be seen in office to measure their ocular alignment; glaucoma patients eventually have to have an IOP taken, and so on. Vongsachang et al recently analyzed responses to an online survey on two national pediatric ophthalmology list-serves. They found that, after using telemedicine during the height of the pandemic, pediatric ophthalmologists were dramatically less likely to continue using telemedicine in the future.20 From the above, we might infer that although telemedicine currently demonstrates situational utility, it requires technological upgrades and improvements before being more widely integrated into future ophthalmologic practice. This may be especially true when the patient evaluation is being conducted while the examinee is at home. The ready availability of additional examination tools, such as devices to measure IOP at home, or ones that could project a slit beam with greater magnification and allow visualization of the fundus over video, would be an important step in that direction.
There are some limitations of our study, one being its retrospective nature. Eighty percent of the patients who had telemedicine visits did not have an in-office follow-up examination, preventing assessment of the telemedicine visit’s precision for a majority of patients. Further, there may have been a difference between patients who chose to follow up or not. For example, routine and non-urgent patients may have been lost to follow-up due to resolution of their condition, which may have biased for patients whose condition worsened. Finally, the survey was completed by only 15.0% of patients who had completed telemedicine visits. Although a Cronbach’s alpha of 0.74 suggests acceptable internal validity, a low response rate may be suggestive of a lack of external validity, generalizability of our results, and may introduce a response bias.
Conclusions
Telehealth has provided a means, using modern telecommunications technology, for physicians to evaluate and manage patients remotely without direct physical interaction. While telemedicine has been effectively utilized to a more limited extent for decades, its need and use have come to the forefront during the COVID-19 pandemic. The high satisfaction and diagnostic precision of teleophthalmology have provided patients a safe alternative to access healthcare remotely. If required, there remains the ability to schedule an in-person follow-up or emergency visit. This flexibility allows telemedicine to act as an effective screening tool, ensuring that the risk of patient exposure to COVID-19 is weighed against the need for urgent ophthalmologic care. Our generally successful experience with virtual medicine during the pandemic has also caused us to envision the possibility of utilizing telemedicine in a hybrid fashion going forward. Limitations in our study include a low survey response rate (15%) and in-person follow-up (20%), which may lower the generalizability of our results and introduce response bias. In future studies, we would want to examine whether teleophthalmology could be used not just as an alternative to in-person eyecare, but also to expedite referrals, consults, and communication between ophthalmologists and other specialists. We have already suggested that technological advances would likely be necessary for telemedicine to increase its capability and utility. With such improvements, telemedicine could potentially become a viable tool for ancillary and even standard ophthalmology practice in the future.
Abbreviations
SBUH, Stony Brook University Hospital; SD, standard deviation; IOP, intraocular pressure.
Data Sharing Statement
Data supporting the results reported in the manuscript are securely stored in Dropbox and may be shared via further inquiry with the corresponding author. There are no additional unpublished study data.
Acknowledgment
Benjamin Hsiao, Ph.D., Distinguished Professor of Chemistry and Director, Center for Integrated Electric Energy Systems, Stony Brook University, provided editorial advice on the paper.
The abstract of this paper was presented at the 2022 ARVO Annual Meeting, held in Denver, CO, May 1–4, 2022, as a poster presentation with interim findings. The poster’s abstract was published in Invest Ophthalmol Vis Sci 2022;63:1382-A0078.
Funding
The authors report no funding or financial support.
Disclosure
The authors declare no competing interests or other conflicts of interest.
References
1. Levin YS, Warshaw EM. Teledermatology: a review of reliability and accuracy of diagnosis and management. Dermatol Clin. 2009;27(2):163–176. doi:10.1016/j.det.2008.11.012
2. Rathi S, Tsui E, Mehta N, et al. The Current State of Teleophthalmology in the United States. Ophthalmology. 2017;124(12):1729–1734. doi:10.1016/j.ophtha.2017.05.026
3. Mueller KJ, Potter AJ, MacKinney AC, et al. Lessons from tele-emergency: improving care quality and health outcomes by expanding support for rural care systems. Health Aff. 2014;33(2):228–234. doi:10.1377/hlthaff.2013.1016
4. Stanimirovic A, Francis T, Shahid N, et al. Tele-retina screening of diabetic retinopathy among at-risk populations: an economic analysis. Can J Ophthalmol. 2020;55(1):8–13. doi:10.1016/j.jcjo.2019.06.008
5. Avidor D, Loewenstein A, Waisbourd M, et al. Cost-effectiveness of diabetic retinopathy screening programs using telemedicine: a systematic review. Cost Eff Resour Alloc. 2020;18(1):16. doi:10.1186/s12962-020-00211-1
6. Brady CJ, Garg S. Telemedicine for Age-Related Macular Degeneration. Telemed J E Health. 2020;26(4):565–568. doi:10.1089/tmj.2020.0011
7. Kiage D, Kherani IN, Gichuhi S, et al. The Muranga Teleophthalmology Study: comparison of Virtual (Teleglaucoma) with in-Person Clinical Assessment to Diagnose Glaucoma. Middle East Afr J Ophthalmol. 2013;20(2):150–157. doi:10.4103/0974-9233.110604
8. Faes L, Maloca PM, Hatz K, et al. Transforming ophthalmology in the digital century—new care models with added value for patients. Eye. 2023;37(11):2172–2175. doi:10.1038/s41433-022-02313-x
9. Kirkizlar E, Serban N, Sisson JA, et al. Evaluation of telemedicine for screening of diabetic retinopathy in the Veterans Health Administration. Ophthalmology. 2013;120(12):2604–2610. doi:10.1016/j.ophtha.2013.06.029
10. Sanchez CR, Silva PS, Cavallerano JD, et al. Ocular telemedicine for diabetic retinopathy and the Joslin Vision Network. Semin Ophthalmol. 2010;25(5–6):218–224. doi:10.3109/08820538.2010.518893
11. Lelli GJ, Luo S, Liu Y, et al. Telemedicine Use by Oculoplastic Surgeons During the COVID-19 Pandemic. Telemed J E Health. 2022;28(6):878–887. doi:10.1089/tmj.2021.0307
12. Haimi M, Goren U, Grossman Z. Barriers and challenges to telemedicine usage among the elderly population in Israel in light of the COVID-19 era: a qualitative study. Digit Health. 2024;10:20552076241240235. doi:10.1177/20552076241240235
13. Telemedicine During the COVID-19 Public Health Emergency. Eyenet. 2020;1:1.
14. Richter GM, Sun G, Lee TC, et al. Speed of telemedicine vs ophthalmoscopy for retinopathy of prematurity diagnosis. Am J Ophthalmol. 2009;148(1):136–142.e132. doi:10.1016/j.ajo.2009.02.002
15. Nikolaidou A, Tsaousis KT. Teleophthalmology and Artificial Intelligence As Game Changers in Ophthalmic Care After the COVID-19 Pandemic. Cureus. 2021;13(7):e16392. doi:10.7759/cureus.16392
16. Mohammadpour M, Heidari Z, Mirghorbani M, et al. Smartphones, tele-ophthalmology, and VISION 2020. Int J Ophthalmol. 2017;10(12):1909–1918. doi:10.18240/ijo.2017.12.19
17. Than J, Sim PY, Muttuvelu D, et al. Teleophthalmology and retina: a review of current tools, pathways and services. Int J Retina Vitreous. 2023;9(1):76. doi:10.1186/s40942-023-00502-8
18. Shah YS, Fliotsos MJ, Alaqeel A, et al. Use of Teleophthalmology for Evaluation of Ophthalmic Emergencies by Ophthalmology Residents in the Emergency Department. Telemed J E Health. 2022;28(6):858–864. doi:10.1089/tmj.2021.0334
19. Chen DA, Tran AQ, Dinkin MJ, et al. Ophthalmic Virtual Visit Utilization and Patient Satisfaction During the COVID-19 Pandemic. Telemed J E Health. 2022;28(6):798–805. doi:10.1089/tmj.2021.0392
20. Vongsachang H, Lagstein O, Boland MV, et al. Telemedicine utilization by pediatric ophthalmologists during the COVID-19 pandemic. J Aapos. 2021;25(5):293–295.e291. doi:10.1016/j.jaapos.2021.05.018
21. Ramakrishnan MS, Gilbert AL. Telemedicine in neuro-ophthalmology. Curr Opin Ophthalmol. 2021;32(6):499–503. doi:10.1097/icu.0000000000000800
22. Kalra G, Williams AM, Commiskey PW, et al. Incorporating Video Visits into Ophthalmology Practice: a Retrospective Analysis and Patient Survey to Assess Initial Experiences and Patient Acceptability at an Academic Eye Center. Ophthalmol Ther. 2020;9(3):549–562. doi:10.1007/s40123-020-00269-3
23. Fydanaki O, Kanwar T, Bhalla M, et al. Video consultations in oculoplastic service: a continuing role post-pandemic? Eye. 2023;37(13):2826–2827. doi:10.1038/s41433-023-02385-3
24. Trattler W, Karpecki P, Rapoport Y, et al. The Prevalence of Demodex Blepharitis in US Eye Care Clinic Patients as Determined by Collarettes: a Pathognomonic Sign. Clin Ophthalmol. 2022;16:1153–1164. doi:10.2147/opth.S354692
25. Galvis-Ramírez V, Tello-Hernández A, Álvarez-Osorio L, et al. The prevalence of Demodex folliculorum infection in patients attending a general ophthalmological consultation. Rev Salud Publica. 2011;13(6):990–997. doi:10.1590/s0124-00642011000600011
26. Ayres BD, Donnenfeld E, Farid M, et al. Clinical diagnosis and management of Demodex blepharitis: the Demodex Expert Panel on Treatment and Eyelid Health (DEPTH). Eye. 2023;37(15):3249–3255. doi:10.1038/s41433-023-02500-4
27. Diener-Kudisch S, Ramírez-Barajas L, Perezpeña-Diazconti JM, et al. Correlation between Demodex species in primary and recurrent chalazia. Arch Soc Esp Oftalmol. 2024;99(2):49–55. doi:10.1016/j.oftale.2023.11.009
28. Forton F, De Maertelaer V. Rosacea-like demodicosis and papulopustular rosacea may be two phenotypes of the same disease, and pityriasis folliculorum may be their precursor: response to the comment of Tatu. J Eur Acad Dermatol Venereol. 2019;33(1):e47–e48. doi:10.1111/jdv.15162
29. Tatu AL, Clatici VG, Nwabudike LC. Rosacea-like demodicosis (but not primary demodicosis) and papulopustular rosacea may be two phenotypes of the same disease – a microbioma, therapeutic and diagnostic tools perspective. J Eur Acad Dermatol Venereol. 2019;33(1):e46–e47. doi:10.1111/jdv.15166
30. Tatu AL, Ionescu MA, Cristea VC. Demodex folliculorum associated Bacillus pumilus in lesional areas in rosacea. Indian J Dermatol Venereol Leprol. 2017;83(5):610–611. doi:10.4103/ijdvl.IJDVL_921_16
31. De Arrigunaga S, Aziz K, Lorch AC, et al. A Review of Ophthalmic Telemedicine for Emergency Department Settings. Semin Ophthalmol. 2022;37(1):83–90. doi:10.1080/08820538.2021.1922712
32. Parikh AA, Liebman DL, Armstrong GW. A Novel Ophthalmic Telemedicine Program for Follow-Up of Minor Ophthalmic Emergencies. Telemed J E Health. 2024;30(3):835–840. doi:10.1089/tmj.2023.0129
33. Meshkin RS, Armstrong GW, Hall NE, et al. Effectiveness of a telemedicine program for triage and diagnosis of emergent ophthalmic conditions. Eye. 2023;37(2):325–331. doi:10.1038/s41433-022-01940-8
34. Alhumud A, Al Adel F, Alwazae M, et al. Patient Satisfaction Toward a Tele-Retinal Screening Program in Endocrinology Clinics at a Tertiary Hospital in Riyadh, Saudi Arabia. Cureus. 2020;12(5):e7986. doi:10.7759/cureus.7986
35. Prakash B. Patient satisfaction. J Cutan Aesthet Surg. 2010;3(3):151–155. doi:10.4103/0974-2077.74491
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

