Back to Journals » Clinical Ophthalmology » Volume 18
The Association of Primary Open Angle Glaucoma and Ocular Hypertension with Anti-VEGF Injections
Authors LoBue SA , Albear S, Martin C, Guagliardo A, Chang T
Received 5 September 2024
Accepted for publication 28 November 2024
Published 19 December 2024 Volume 2024:18 Pages 3861—3870
DOI https://doi.org/10.2147/OPTH.S482123
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Stephen A LoBue,1,2 Sinan Albear,1,2 Curtis Martin,1 Alan Guagliardo,1 Tom Chang1
1Department of Ophthalmology, Acuity Eye Group, Pasadena, CA, USA; 2Department of Ophthalmology, SUNY Downstate Medical Center, Brooklyn, NY, USA
Correspondence: Tom Chang, Acuity Eye Group, Vitreoretinal Surgeon, 100 E California Blvd, Pasadena, CA, 91105, USA, Email [email protected]
Purpose: To study the effects of anti–VEGF injections on the prevalence of ocular hypertension (OHT), sustained elevated intraocular pressure (SE-IOP), and primary open-angle glaucoma (POAG) with age-matched controls.
Methods: A retrospective case-control study was performed with neovascular age-related macular degeneration (AMD) or diabetic macular edema (DME) against a control group involving atrophic AMD or diabetic retinopathy (DR) without DME. Bevacizumab, ranibizumab, or a combination of both were used in the treatment group. OHT was defined as IOP> 21 mm Hg while SE-IOP was defined as IOP that increased by > 6 mmHg or was > 25 mm Hg on two or more visits, 30 days apart. Patients with a pre-existing history of glaucoma, vein occlusions, IVI steroids, and pars plana vitrectomy were excluded.
Results: A total of 1312 eyes of 784 patients were included in the study. Using age-matched controls, the treatment and control group was further refined to 394 eyes of 224 patients compared to 340 eyes from 170 patients respectively. The mean age was 58.4 ± 8.7 for the control versus 58.8 ± 8.8 years for the treatment group. The average IOP was higher in the injection group compared to the control with 25.8 ± 9.3 versus 19.5 ± 5.1 mmHg respectively, P< 0.001. Significant increases in POAG (10.7% vs 2.9%, p< 0.01), OHT (67.0% vs 22.4%, p< 0.001), and SE-IOP (41.1% vs 7.6%, p< 0.001) were seen in the injection group compared to the age-matched control group. The rates of POAG and OHT were positively associated with the number of injections, R2=0.856, P< 0.01 and R2=0.749, P< 0.05, respectively.
Conclusion: Compared to age-matched controls, patients treated with anti-VEGF agents demonstrated an increased rate of OHT, SE-IOP, and POAG which correlated with the number of IVIs. However, additional prospective studies are needed to determine if there is a true association between intravitreal anti-VEGF injections and glaucoma.
Keywords: intravitreal injection, IVI, sustained-elevated intraocular pressure, SE-IOP, primary open-angle glaucoma, POAG, age-related macular degeneration, AMD
Introduction
Anti-vascular endothelial growth factor (VEGF) has revolutionized the treatment of certain retinal pathologies. Landmark trials have proven the efficacy of anti-VEGF in improving vision in age-related macular degeneration (AMD) and diabetic macular edema (DME).1–4 Although anti-VEGF has a favorable safety profile in these trials, several studies have documented transient elevation of intraocular pressure (IOP) immediately after intravitreal injection (IVI).5–7
However, it is controversial whether repeated IVI can lead to sustained elevated intraocular pressure (SE-IOP), described as an increase in IOP above baseline by ≥6 mmHg and/or an IOP elevation to >21-24 mmHg on two or more consecutive visits beyond 30 days. Two multicenter clinical trials, ANCHOR and MARINA, evaluating anti-VEGF for the treatment of AMD, did not show SE-IOP with IVI of ranibizumab.8,9 However, further subgroup analysis by Bakri et al on both ANCHOR and MARINA studies demonstrated that 26.1% and 13.6% of patients presented with IOP ≥21 mmHg and ≥6 mmHg above the baseline.10
Patients with persistent ocular hypertension (IOP>21 mmHg) are at increased risk of developing primary open-angle glaucoma (POAG).11 The risk of POAG is significantly associated with regression of the retinal nerve fiber layer (RNFL) and an increase in the vertical cup-to-disk ratio.12–14 Thus, elevated IOP from IVI may increase the risk of OHT or SE-IOP, POAG, and RNFL thinning. To better quantify the possible association between elevated IOP and IVI of anti-VEGF, we performed a retrospective case-control study comparing the rates of OHT, SE-IOP, POAG, and RNFL thinning between patients receiving anti-VEGF for wet AMD or DME and a non-injection group involving atrophic AMD or diabetic retinopathy without DME. The two conditions, OHT and SE-IOP, are sometimes considered a continuum and can be present in the same patient at different times. However, to better understand the fluctuations in IOP, we chose to separate these definitions. As a result, we hypothesized that IVI of anti-VEGF is associated with a sustained increase in IOP along with a higher rate of glaucoma.
Material and Methods
A retrospective case-control study was conducted at the Acuity Eye Group medical centers in Southern California, United States. The study was approved by the Advarra Institutional Review Board (IRB) and was conducted according to the tenets of the Declaration of Helsinki. All patients provided verbal and written informed consent before participating in the study. The study population included consecutive eligible patients with neovascular AMD, diabetic retinopathy (DR) with or without DME, or atrophic AMD who had received treatment for at least one year at the center.
Patients who were actively treated from July 1, 2018, to October 1, 2019, were consecutively selected for the study to avoid selection bias. A chart review examined up to four years of data for each patient being reviewed in this time period with a mean of 3.1 ± 0.5 years. IVI of anti-VEGF agents, either bevacizumab, ranibizumab, or a combination of the two, were administered by a single clinician. Patients with neovascular AMD or DR with DME were included in the treatment group and received anti-VEGF IVIs. Patients with atrophic AMD or DR without DME served as the control group and did not receive any anti-VEGF agents. Patients were consecutively included in this study. As a result, the time points for anti-VEGF treatment were random and not identical between patients.
IOP was measured using a handheld tonometer (Tono-Pen XL, Haag-Streit, Köniz, Switzerland) before every IVI of anti-VEGF or clinic visit in the treatment and non-treatment groups, respectively. IOP was compared with a chart review of patients followed up in the clinic for at least 1 year with a maximum duration of 5 years. Data from serial IOP were used to create an average for each patient. All IOP measurements involve patients without treatment of glaucoma medication. OHT was defined as an elevation of IOP>21 on two or more office visits 30 days apart. SE-IOP was classified as an increase in average IOP> 6 mmHg or a maximum IOP>25 mmHg on two or more office visits 30 days apart.
Patients were seen by glaucoma specialists for full glaucoma screening, including a Humphrey visual field 24–2 (HVF), optic nerve optical coherence tomography (OCT) via Stratus OCT (Carl Zeiss Meditec Inc)., gonioscopy, IOP measurement with Goldmann applanation tonometry, and full anterior and posterior examination.
POAG was defined as RNFL defects with corresponding visual field (VF) loss, without other known secondary causes of glaucoma. A glaucoma suspect was defined as a patient with or without OHT who had either RNFL defects or VF loss (not both) without any known secondary cause. RNFL progression was defined as a decrease of at least 8 µm at any clock hour on reliable testing (eg, good signal strength, no artifacts, and repeatability).
Inclusion Criteria
Patients eligible for the study included men and women aged > 18 years who were treatment-naïve and eligible for anti-VEGF injections (bevacizumab, ranibizumab, or a combination of both) in one or both eyes. All patients were evaluated by an ophthalmologist using baseline optic nerve OCT and HVF.
Exclusion Criteria
Patients excluded from the study involved a pre-existing history of glaucoma, ocular pathology that limited the patient’s visual acuity to perform HVF, insufficient data secondary to unreliable HVF or OCT, patients with inadequate media clarity, patients eligible for anti-VEGF injections but who had prior treatment with panretinal photocoagulation or IVI triamcinolone (steroid), history of central retinal vein occlusion (CRVO), and patients with a history of vitrectomy.
The primary study aimed to compare the differences in average IOP, OHT, SE-IOP, and POAG between the control and IVI groups. The secondary study aimed to identify the relationship between POAG, OHT, and RNFL thinning and the number of injections.
Descriptive statistics with a two-tailed Student’s t-test were used to compare age and mean IOP between the study and control groups (± standard deviation). The chi-square test was used to determine the significance of the association between OHT, SE-IOP, POAG, and glaucoma suspects between the control and injection groups. ANOVA and regression analysis were used to determine the association between the number of injections with POAG and OHT.
Results
A total of 1516 eyes from 928 consecutive patients eligible for anti-VEGF injections were analyzed. Patients treated for vein occlusions (93), prior vitrectomy (2), prior history of IVI triamcinolone (29), prior history of anti-VEGF injections in the control group (36), or insufficient or poor data quality (44) were excluded from this study. Thus, 1312 eyes of 784 consecutive patients (411 females and 373 males) with DR and AMD were included in the study (Table 1).
 |
Table 1 Demographic Data Between the Control and Study (Anti-VEGF) Group with and Without Age-Match Controls |
The mean age of the patients in the study was 70.6 ±14.7 years of age. In the control group, the mean age was 65.7 ± 12.5 compared to 73.2 ± 15.1 years of age in the injection group, P<0.05. The injection group had a bimodal distribution of patients aged 60–65 and 85–90 years of age (Figure 1). Female gender were equally divided between the study and control groups at 51% and 53%, respectively P>0.05 (Table 1). The mean average ocular pressure for all combined patients was 23 ± 8.2 mmHg.
The anti-VEGF group included 772 eyes of 514 patients (272 females, 242 males).
A total of 452 patients had neovascular AMD versus 320 with DR and DME. In the anti-VEGF group, 405 eyes received bevacizumab only, 125 received bevacizumab plus ranibizumab, and 242 received ranibizumab only with a total mean IVI of 10.2 ± 8.3 for the entire study (Table 1). Thus the average interval dosing was approximately every 3 months. In the injection group, 76.3% were phakic (Table 1). The average ocular pressure in the anti-VEGF group was 24.9 ± 8.8 mmHg (Figure 2).
 |
Figure 2 Mean IOP changes between all groups. All IOPs were treatment naïve patients, not on glaucoma medication. Notes: ‡ P < 0.001. |
The control group included 540 eyes of 270 patients (139 females and 131 males). A total of 500 eyes had DR without DME, and 40 had atrophic AMD. In the control group, 81.1% of patients were phakic (Table 1). The average ocular pressure in the control group was 19.4 ± 5.3 mmHg (Figure 2).
The average IOP was significantly greater in the treatment group compared to the control, 24.9 ± 8.8 versus 19.4 ± 5.3 mmHg respectively, p<0.001 (Figure 2). The anti-VEGF group had significantly more patients with OHT and SE-IOP than the control group 65.9% vs 21.5% and 37.6% versus 5.9%, respectively; (P<0.001, Table 2). Compared to the control group, more patients in the anti-VEGF group had POAG, 3.7% versus 12.3%, respectively (P<0.001, Table 2). In addition, more patients were categorized as glaucoma suspects in the treatment group than in the control, 18.7% versus 13.3%, respectively (P<0.05, Table 2).
Among the glaucoma suspects in the anti-VEGF IVI group, 69.8% had OHT, 62.5% had RNFL thinning, and 17.7% had RNFL thinning without OHT. Among glaucoma suspects who had RNFL thinning without OHT, 17.2% had an optic nerve cup/disc ratio (C/D) of <0.4, 41.4% had a C/D of ≤0.5, and 37.9% had a C/D ≥0.6.
The number of IVIs was grouped as 1–5, 6–10, 11–15, 16–20, and 21+. Regression analysis was used to determine whether repeat IVI was associated with increased rates of OHT and POAG. The regression model showed that POAG (R2=0.857, ANOVA P<0.01) and OHT (R2=0.749, ANOVA P<0.05) were correlated positively with the number of IVI (Figures 3 and 4).
 |
Figure 3 The number of IVIs were grouped from 1–5, 6–10, 11–15, 16–20, and 21+. Regression analysis demonstrated a positive correlation with the number of injections and POAG, R2=0.857, P<0.01. |
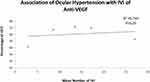 |
Figure 4 The number of IVIs were grouped from 1–5, 6–10, 11–15, 16–20, and 21+. Regression analysis demonstrated a positive correlation with the number of injections and OHT, R2=0.749, P<0.05. |
Owing to the bimodal distribution of the injection group, a statistical difference in the mean population was found between the study and control group (P<0.05, Figure 1). To equalize the mean ages between the groups, a cut-off in max-age was set at 70 years of age to reflect the first bimodal peak of the injection group (Figure 1). Means with this new cut-off were 58.4 ± 8.7 for the control versus 58.8 ± 8.8 years of age for the injection group (P>0.05, Table 1). In addition, 58% of the patients in the control group were female, compared to 46% in the injection group (Table 1). The total number of control patients was 340 eyes from 170 patients, comprising 155 patients with DR without DME and 15 with atrophic AMD. Within the control group, 90% of the patients were phakic compared with 84.4% in the injection group (Table 1).
The total number of patients in the age-matched injection group were 394 eyes of 224 patients, consisting of 123 with neovascular AMD and 271 with DME (Table 1). The average IOP was still significantly higher in the injection group compared to the control with 25.8 ± 9.3 versus 19.5 ± 5.1 mmHg respectively, p<0.001 (Figure 2). Significant increases in POAG (10.7% versus 2.9%), OHT (67% versus 22.4%), and SE-IOP (41.1% versus 7.6%) were seen in the injection compared to the control group (P<0.01, P<0.001, and P<0.001, respectively, Table 3). The rate of glaucoma suspects was similar between the injection and control groups (P>0.05, Table 3). The mean number of injections was 9.4 ± 7.8 for the duration of the study (Table 1).
Discussion
Landmark trials have reported that IVI of anti-VEGF is effective in treating neovascular AMD and DME.15,16 However, anti-VEGF treatment is associated with a range of sequelae including an acute rise in IOP, intraocular inflammation, endophthalmitis, ocular hemorrhage, and rarely, ischemic optic neuropathy (ION).17 Among these sequelae, ocular inflammation and acute rise in IOP are the most frequent.18
Although transient OHT, occurring 0 to 60 min after IVI of anti-VEGF, has been abundantly reported in the literature,19–23 controversy exists as to whether patients can develop SE-IOP or increased rates of OHT. In our study, the mean IOP was significantly greater in the injection group than in the age-matched and non-matched controls (P<0.001). In addition, the anti-VEGF group had significantly more patients with OHT and SE-IOP than both age-matched and non-matched controls (p<0.01, Tables 2 and 3).
In a large study by Freund et al24 involving analyses from two Phase III randomized clinical trials, IOP >21 mmHg was observed in 10% of patients at 52 weeks and in 15% of patients at 96 weeks. A meta-analysis of five randomized controlled trials (RCTs, N=1428) and 17 non-RCTs (N=8358) in patients with wet AMD or DME reported a two-fold increase in the risk of SE-IOP after multiple anti-VEGF IVIs.25 The analysis of the RCTs showed an increased risk of SE-IOP in the anti-VEGF IVI group compared with the laser or sham injection group (risk ratio (RR)) = 3.00, 95% confidence interval ((CI):1.63–5.53). The increased SE-IOP risk correlated with the follow-up duration. The relative risk (RR) of SE-IOP was 2.14 (95% CI 0.69–6.57) at six months, 3.15 (95% CI 0.99–10.09) at 12 months, and 3.48 (95% CI 1.38–8.78) at 23 months. Pooled analysis of the data from non-RCTs showed that the prevalence of SE-IOP was 4.7% (95% CI 3.7–5.8), irrespective of the diagnostic criteria.25 The RR of SE-IOP was higher when pre-existing glaucoma patients were included in the analysis (RR (excluding glaucoma patients)=2.6 (CI, 1.16–5.81; p=0.02) vs RR (including glaucoma patients)=3.48 (CI, 1.38–8.78; p=0.008).25
Similarly, the study by Good et al showed that the rate of elevated IOP was significantly higher in patients with pre-existing glaucoma than in those without (33% versus 3.1%, respectively, p < 0.001).26 In our study, patients with a prior diagnosis of glaucoma or vein occlusion were excluded from the analysis due to their increased risk of OHT.
However, some reports in the literature do not find a significant association between IVI of anti-VEGF and sustained OHT.27–30 Compared to the above studies, the studies that found no association contained a smaller sample size, ranging from 40 to 302 eyes receiving IVI. The largest study by Wehrli et al31 (N= 302 injected vs 226 control eye) showed that the per eye-year incidence of developing SE-IOP in injected vs control eyes was low and not statistically significant between groups (0.51% vs 1.00%; hazard ratio = 0.48; 95% CI:0.11–2.23). Boyer et al documented equal rates of OHT between patients treated with IVI of anti-VEGF and untreated patients.27 In their study, 24.5% of the treated group compared to 21.5% of the untreated group had at least one measurement of IOP above 22 mmHg over a mean follow-up period of 38.5 weeks, p=0.63. Among subjects with SE-IOP, 10.7% had a history of glaucoma.
Contrasting data is also seen regarding the association between IVI of anti-VEGF with glaucoma and RNFL thinning. In a recent study, Filek et al,12 reported a significant increase in cup volume and vertical C/D (P<0.001) after 24 months in DME patients receiving anti-VEGF IVI (N=30) versus controls not receiving anti-VEGF (N=21). However, another study (N=21) found that the mean change in C/D between the anti-VEGF and control group was not statistically significant, P=0.90.32 The mean change in C/D also did not correlate significantly with the number of injections (P=0.33 for ≤5 injections and P=0.70 for >5 injections).32 Another prospective observational cohort study (N=30) found no correlation between pre- and post-anti-VEGF RNFL thickness.33
However, our study documented a higher rate of POAG (12.26% versus 3.70%) and glaucoma suspects (18.68% versus 13.33%) in patients receiving anti-VEGF than in controls, P<0.001 and p<0.05 respectively. Initially, in the first review, the higher rate of POAG in the injection group may have been associated with the significantly older mean age of individuals in the treatment group, as age has been documented as a risk factor for glaucoma.34 However, after analysis with age-matched controls, the rate of POAG (10.7% vs 2.9%) was still significantly higher in the injection group compared to the control group (P<0.001). Discrepancies in age between the groups were likely due to the higher proportion of AMD patients in the injection group than in the control group. Nevertheless, the mean age difference between the treatment and control groups poses a problem in that the prevalence of glaucoma is associated with age. As a result, the age difference between groups is a limitation and weakness of this study, which we attempted to resolve with age-matched groups.
Martinez-de-la-Casa et al documented the effects of intravitreal ranibizumab on RNFL thickness in patients with no prior history of OHT or POAG.35 Compared with baseline, thickness reductions were 5.6 ± 9.1 μm in the injection group (P<0.001) and 1.3 ± 9.6 μm in the control group (P=0.477), amounting to 5.2% loss of RNFL in the study group over the course of a year.
Another more recent study supporting our findings was a retrospective study by Wingard et al, which analyzed the association between unilateral POAG and OHT in patients receiving unilateral IVI of anti-VEGF for AMD. Unilateral glaucoma or sustained OHT developed in 42 patients over the course of follow-up, with 40 events in the injected eye only.36 Statistical modeling predicted elevated risk for onset of POAG with a higher maximum frequency of injections (P<0.0001, odds ratio (OR) 2.18) and with phakic lens status (P=0.0009, OR 0.33 for pseudophakia).36 However, we found no association for developing glaucoma in phakic compared to pseudophakic patients in the injection group. A pharmacoepidemiologic study suggested that the risk of glaucoma surgery was higher in patients who received seven or more bevacizumab IVI annually (RR 2.48; 95% CI, 1.25–4.93).37 However, four to six IVI annually correlated non-significantly with the risk of glaucoma surgery. Both of these studies reinforce our findings regarding a positive association between the number of injections of POAG and OHT.
Nevertheless, there are several hypotheses regarding the mechanism by which repeat IVI leads to SE-IOP, RNFL loss, and glaucoma. A plausible hypothesis for acute RNFL loss leading to glaucoma may be transient IOP spikes after IVI. In an alternative study, we analyzed a series of 617 patients and noted significant changes in IOP ten minutes after IVI. The average pre-injection IOP was 16 ±5 mmHg which increased to 25 ± 10 mmHg at 10 minutes, P<0.0001.23 However, 2.8% of patients had a clinically significant elevation of IOP >35 mmHg at 30 minutes after the initial injection. Patients receiving a smaller 31-gauge IVI, history of glaucoma, and a pre-injection IOP ≥ 25 mmHg had a greater association of developing a significant pressure spike > 35 mmHg after 30 minutes.23 Thus, repeated pressure spikes in susceptible patients after IVI may increase the association of RNFL loss and glaucoma.
A positive correlation with SE-IOP may be explained by decreased aqueous outflow through the obstruction of the trabecular meshwork (TM). Several possible mechanisms of IVI can cause obstruction of the TM, including large protein aggregates within bevacizumab,38 silicone oil contamination from needles and syringes used for injections,39 decrease in aqueous outflow from reduced levels of nitric oxide in the anterior chamber,40 and disruption of VEGF signaling in the TM, impairing endothelial function and outflow.41
However, RNFL loss may be due to other possible mechanisms besides transient spikes in IOP or SE-IOP. For example, in our anti-VEGF group, 17.7% of glaucoma suspects showed RNFL thinning without OHT. Of the glaucoma suspects with documented RNFL thinning without OHT, 37.9% had cupping progression with a C/D of ≥ 0.6. It is important to note that these patients were individually reviewed and did not have systemic findings consistent with chronic low vascular perfusion such as Raynaud’s, migraines, or cold intolerance. Although VEGF plays a significant role in the pathophysiology of neovascularization, it has been discovered in animal models to be a neurotrophic factor responsible for cell viability, repair, and function in the RNFL.42–44 Inhibition of the VEGF pathway accelerated loss of the RNFL in a glaucoma model of rats.45 The reduction of neurotrophic cytokines responsible for retinal ganglion cell survivability may be a contributing factor for glaucomatous progression outside of elevated IOP.
Nevertheless, our study had several limitations. First, multiple glaucoma specialists within the clinical setting were involved; therefore, there could be judgment bias in various assessments and POAG diagnosis. In addition, IOP measurements were not standardized by Goldmann applanation tonometry by a single provider at a similar time of day. As a result, there is potential for increased levels of intra-patient variability in IOP measurements, possibly clouding the association between IVI and IOP. Finally, a retrospective study may be limited in determining our hypotheses. Although we used strict inclusion and exclusion criteria, it is possible that other factors influenced the rates of OHT and POAG between the groups including axial length and anterior chamber depth. Although we found a strong association between IVI and subsequent OHT, SE-IOP, or POAG, we recommend caution as the correlation does not equal causation. Discrepancies in age as well as other underlying factors not addressed may have biased our data. Overall, additional larger prospective randomized studies are needed to determine if there is a true association exists between intravitreal anti-VEGF, OHT, SE-IOP, or POAG.
Conclusions
We present a consecutive series of patients treated with anti-VEGF agents compared to age-matched controls, noting an increased rate of mean IOP, OHT, SE-IOP, and POAG in the IVI group. The rates of POAG and OHT strongly correlated with the number of IVIs. We hypothesize that repeated pressure spikes occurring immediately after IVI may be associated with long-term RNFL loss and elevated IOP in susceptible patients. However, this study had several limitations. More understanding is needed regarding the mechanism of POAG with IVI as well as the effect of anti-VEGF on the RNFL thickness.
Data Sharing Statement
The data that support the findings of this study are not publicly available due to the files containing information that could compromise the privacy of research participants but are available from the corresponding author TC upon reasonable request.
Ethics Compliance
Ethical approval for the study was obtained from the Advarra Institutional Review Board before the start of the study from Advarra Institutional Review Board (IRB). All participants provided written informed consent, in accordance with the Declaration of Helsinki.
Acknowledgment
The authors acknowledge Dr. Kokil Mathur and Dr. Natasha Das from Hazlo Consultancy for providing preliminary writing, editing, and formatting assistance in this project.
The abstract of this paper was presented at The Association for Research in Vision and Ophthalmology (ARVO) with interim findings. The poster’s abstract was published in ARVO Annual Meeting Abstract in Investigative Ophthalmology and Visual Science (IOVS): https://iovs.arvojournals.org/article.aspx?articleid=2768430
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The work was supported by the Acuity Eye Group. No outside funding or grants were necessary for this project.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Sun JK, Glassman AR, Beaulieu WT, et al. Rationale and application of the protocol S anti-vascular endothelial growth factor algorithm for proliferative diabetic retinopathy. Ophthalmology. 2019;126(1):87–95. doi:10.1016/j.ophtha.2018.08.001
2. Mitchell P, Bandello F, Schmidt-Erfurth U, et al. The restore study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118(4):615–625. doi:10.1016/j.ophtha.2011.01.031
3. Ishibashi T, Li X, Koh A, et al. The reveal study: ranibizumab monotherapy or combined with laser versus laser monotherapy in asian patients with diabetic macular edema. Ophthalmology. 2015;122(7):1402–1415. doi:10.1016/j.ophtha.2015.02.006
4. Gross JG, Glassman AR, Jampol LM, et al.; Writing Committee for the Diabetic Retinopathy Clinical Research Network. Panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA. 2015;314(20):2137–2146. doi:10.1001/jama.2015.15217
5. Kim KS, Jee D. Effect of the Honan intraocular pressure reducer on intraocular pressure increase following intravitreal injection using the tunneled scleral technique. Jpn J Ophthalmol. 2011;55(6):632–637. doi:10.1007/s10384-011-0088-1
6. Pang CE, Mrejen S, Hoang QV, Sorenson JA, Freund KB. Association between needle size, postinjection reflux, and intraocular pressure spikes after intravitreal injections. Retina. 2015;35(7):1401–1406. doi:10.1097/IAE.0000000000000476
7. Gregori NZ, Weiss MJ, Goldhardt R, et al. Ocular decompression with cotton swabs lowers intraocular pressure elevation following intravitreal injection. J Glaucoma. 2014;23(8):508–512. doi:10.1097/IJG.0b013e318294865c
8. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–1431. doi:10.1056/NEJMoa054481
9. Brown DM, Kaiser PK, Michels M, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1432–1444. doi:10.1056/NEJMoa062655
10. Bakri SJ, Moshfeghi DM, Francom S, et al. Intraocular pressure in eyes receiving monthly ranibizumab in 2 pivotal age-related macular degeneration clinical trials. Ophthalmology. 2014;121(5):1102–1108. doi:10.1016/j.ophtha.2013.11.029
11. Kass MA, Heuer DK, Higginbotham EJ, et al. The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701–713. doi:10.1001/archopht.120.6.701
12. Filek R, Hooper P, Sheidow TG, Gonder J, Chakrabarti S, Hutnik CM. Two-year analysis of changes in the optic nerve and retina following anti-VEGF treatments in diabetic macular edema patients. Clin Ophthalmol. 2019;13:1087–1096. doi:10.2147/OPTH.S199758
13. Enders P, Sitnilska V, Altay L, Schaub F, Muether PS, Fauser S. Retinal nerve fiber loss in anti-VEGF therapy for age-related macular degeneration can be decreased by anterior chamber paracentesis. OPH. 2017;237(2):111–118. doi:10.1159/000457907
14. Yang HS, Woo JE, Kim MH, Kim DY, Yoon YH. Co-evaluation of peripapillary rnfl thickness and retinal thickness in patients with diabetic macular edema: rnfl misinterpretation and its adjustment. PLoS One. 2017;12(1). doi:10.1371/journal.pone.0170341
15. Sharma T. Evolving role of anti-VEGF for diabetic macular oedema: from clinical trials to real life. Eye. 2020;34(3):415–417. doi:10.1038/s41433-019-0590-0
16. Clearkin L, Ramasamy B, Wason J, Tiew S. Anti-VEGF intervention in neovascular AMD: benefits and risks restated as natural frequencies. BMJ Open Ophthalmol. 2019;4(1):e000257. doi:10.1136/bmjophth-2018-000257
17. Ghasemi Falavarjani K, Nguyen QD. Adverse events and complications associated with intravitreal injection of anti-VEGF agents: a review of literature. Eye. 2013;27(7):787–794. doi:10.1038/eye.2013.107
18. Solomon SD, Lindsley K, Vedula SS, Krzystolik MG, Hawkins BS. Anti‐vascular endothelial growth factor for neovascular age‐related macular degeneration. Cochrane Database Syst Rev. 2019;2019(3). doi:10.1002/14651858.CD005139.pub4
19. Moraru A, Pînzaru G, Moţoc A, Costin D, Brănişteanu D. Incidence of ocular hypertension after intravitreal injection of anti-VEGF agents in the treatment of neovascular AMD. Rom J Ophthalmol. 2017;61(3):207–211. doi:10.22336/rjo.2017.38
20. Kiddee W, Montriwet M. Intraocular pressure changes in non-glaucomatous patients receiving intravitreal anti-vascular endothelial growth factor agents. PLoS One. 2015;10(9). doi:10.1371/journal.pone.0137833
21. Hoguet A, Chen PP, Junk AK, et al. The effect of anti-vascular endothelial growth factor agents on intraocular pressure and glaucoma: a report by the american academy of ophthalmology. Ophthalmology. 2019;126(4):611–622. doi:10.1016/j.ophtha.2018.11.019
22. Silva R, Axer-Siegel R, Eldem B, et al. The SECURE study: long-term safety of ranibizumab 0.5 mg in neovascular age-related macular degeneration. Ophthalmology. 2013;120(1):130–139. doi:10.1016/j.ophtha.2012.07.026
23. LoBue SA, Gindina S, Saba NJ, Chang T, Davis MJ, Fish S. Clinical features associated with acute elevated intraocular pressure after intravitreal anti-VEGF injections. Clin Ophthalmol. 2023;17:1683–1690. doi:10.2147/OPTH.S414212
24. Freund KB, Hoang QV, Saroj N, Thompson D. Intraocular pressure in patients with neovascular age-related macular degeneration receiving intravitreal aflibercept or ranibizumab. Ophthalmology. 2015;122(9):1802–1810. doi:10.1016/j.ophtha.2015.04.018
25. Zhou Y, Zhou M, Xia S, Jing Q, Gao L. Sustained elevation of intraocular pressure associated with intravitreal administration of anti-vascular endothelial growth factor: a systematic review and meta-analysis. Sci Rep. 2016;6(1). doi:10.1038/srep39301
26. Good TJ, Kimura AE, Mandava N, Kahook MY. Sustained elevation of intraocular pressure after intravitreal injections of anti-VEGF agents. Br J Ophthalmol. 2011;95(8):1111–1114. doi:10.1136/bjo.2010.180729
27. Boyer DS, Goldbaum M, Leys AM, Starita C; V.I.S.I.O.N. Study Group. Effect of pegaptanib sodium 0.3 mg intravitreal injections (Macugen) in intraocular pressure: posthoc analysis from V.I.S.I.O.N. study. Br J Ophthalmol. 2014;98(11):1543–1546. doi:10.1136/bjophthalmol-2013-304075
28. Gado AS, Macky TA. Dexamethasone intravitreous implant versus bevacizumab for central retinal vein occlusion-related macular oedema: a prospective randomized comparison. Clin Experiment Ophthalmol. 2014;42(7):650–655. doi:10.1111/ceo.12311
29. Güler M, Capkın M, Simşek A, et al. Short-term effects of intravitreal bevacizumab on cornea and anterior chamber. Curr Eye Res. 2014;39(10):989–993. doi:10.3109/02713683.2014.888452
30. Rusu IM, Deobhakta A, Yoon D, et al. Intraocular pressure in patients with neovascular age-related macular degeneration switched to aflibercept injection after previous anti-vascular endothelial growth factor treatments. Retina. 2014;34(11):2161–2166. doi:10.1097/IAE.0000000000000264
31. Wehrli SJ, Tawse K, Levin MH, Zaidi A, Pistilli M, Brucker AJ. A lack of delayed intraocular pressure elevation in patients treated with intravitreal injection of bevacizumab and ranibizumab. Retina. 2012;32(7):1295–1301. doi:10.1097/IAE.0b013e31823f0c95
32. Seth RK, Salim S, Shields MB, Adelman RA. Assessment of optic nerve cup-to-disk ratio changes in patients receiving multiple intravitreal injections of antivascular endothelial growth factor agents. Retina. 2009;29(7):956–959. doi:10.1097/IAE.0b013e3181a91dfd
33. El-Ashry MF, Lascaratos G, Dhillon B. Evaluation of the effect of intravitreal ranibizumab injections in patients with neovascular age related macular degeneration on retinal nerve fiber layer thickness using optical coherence tomography. Clin Ophthalmol. 2015;9:1269–1274. doi:10.2147/OPTH.S80704
34. Suzuki Y, Iwase A, Araie M, et al. Risk factors for open-angle glaucoma in a Japanese population: the Tajimi Study. Ophthalmology. 2006;113(9):1613–1617. doi:10.1016/j.ophtha.2006.03.059
35. Martinez-de-la-Casa JM, Ruiz-Calvo A, Saenz-Frances F, et al. Retinal nerve fiber layer thickness changes in patients with age-related macular degeneration treated with intravitreal ranibizumab. Invest Ophthalmol Vis Sci. 2012;53(10):6214–6218. doi:10.1167/iovs.12-9875
36. Wingard JB, Delzell DA, Houlihan NV, Lin J, Gieser JP. Incidence of glaucoma or ocular hypertension after repeated anti-vascular endothelial growth factor injections for macular degeneration. Clin Ophthalmol. 2019;13:2563–2572. doi:10.2147/OPTH.S232548
37. Eadie BD, Etminan M, Carleton BC, Maberley DA, Mikelberg FS. Association of repeated intravitreous bevacizumab injections with risk for glaucoma surgery. JAMA Ophthalmol. 2017;135(4):363–368. doi:10.1001/jamaophthalmol.2017.0059
38. Kahook MY, Liu L, Ruzycki P, et al. High-molecular-weight aggregates in repackaged bevacizumab. Retina. 2010;30(6):887–892. doi:10.1097/IAE.0b013e3181d50cea
39. Bakri SJ, Ekdawi NS. Intravitreal silicone oil droplets after intravitreal drug injections. Retina. 2008;28(7):996–1001. doi:10.1097/IAE.0b013e31816c6868
40. Ricca AM, Morshedi RG, Wirostko BM. High intraocular pressure following anti-vascular endothelial growth factor therapy: proposed pathophysiology due to altered nitric oxide metabolism. J Ocul Pharmacol Ther. 2015;31(1):2–10. doi:10.1089/jop.2014.0062
41. Reina-Torres E, Wen JC, Liu KC, et al. VEGF as a paracrine regulator of conventional outflow facility. Invest Ophthalmol Visual Sci. 2017;58(3):1899. doi:10.1167/iovs.16-20779
42. Sondell M, Lundborg G, Kanje M. Vascular endothelial growth factor has neurotrophic activity and stimulates axonal outgrowth, enhancing cell survival and Schwann cell proliferation in the peripheral nervous system. J Neurosci. 1999;19(14):5731–5740. doi:10.1523/JNEUROSCI.19-14-05731.1999
43. Böcker-Meffert S, Rosenstiel P, Röhl C, et al. Erythropoietin and VEGF promote neural outgrowth from retinal explants in postnatal rats. Invest Ophthalmol Vis Sci. 2002;43(6):2021–2026.
44. Nishijima K, Ng YS, Zhong L, et al. Vascular endothelial growth factor-A is a survival factor for retinal neurons and a critical neuroprotectant during the adaptive response to ischemic injury. Am J Pathol. 2007;171(1):53–67. doi:10.2353/ajpath.2007.061237
45. Foxton RH, Finkelstein A, Vijay S, et al. VEGF-A is necessary and sufficient for retinal neuroprotection in models of experimental glaucoma. Am J Pathol. 2013;182(4):1379–1390. doi:10.1016/j.ajpath.2012.12.032
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




