Back to Journals » Psychology Research and Behavior Management » Volume 18
The Impact of Physical Activity on Negative Affect and Sleep Quality in Adolescents: Network Analysis
Received 8 January 2025
Accepted for publication 23 April 2025
Published 23 May 2025 Volume 2025:18 Pages 1199—1210
DOI https://doi.org/10.2147/PRBM.S516487
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Professor Mei-Chun Cheung
Bin Zhang,1 Jianwei Gao2
1Beijing Sport University, Beijing, 100084, People’s Republic of China; 2Zhejiang Normal University, Jinhua, 321004, People’s Republic of China
Correspondence: Jianwei Gao, Zhejiang Normal University, No. 688 Yingbin Road, Jinhua, Zhejiang, People’s Republic of China, Email [email protected]
Background: Negative affect may trigger a variety of psychological and behavioral problems, while physical activity has been shown to reduce negative affect. However, the underlying mechanisms remain unclear. The aim of this study was to investigate the relationship between physical activity and negative affect, specially examining the role of sleep quality in the relationship.
Methods: Cross-sectional design was adopted in this study. A total of 557 adolescents participated in the study, completing self-reported questionnaires on physical activity, sleep quality, and negative affect.
Results: Sleep quality mediated the relationship between physical activity and negative affect. There was a positive correlation between “exercise” and “sleep quality” and a negative correlation between “sleep restfulness” and “feeling bored”.
Conclusion: This study uncovered the underlying mechanism of physical activity associated with negative affect, offering significance for the prevention and intervention of depression and anxiety disorders.
Keywords: physical activity, negative affect, sleep quality, network analysis, adolescents
Introduction
Adolescents, who are transitioning from childhood to young adulthood, experience “developmental transitions” such as escalating life pressures.1 At this stage, however, the brain’s functional systems associated with emotional regulation do not develop in synchrony, resulting in a relatively weak top-down regulatory capacity, which leads to significant emotional instability and an increase in negative experiences.2 Negative affect refers to the negative experiences that occur when an individual’s needs are not met.3 Adolescents’ common negative affect primarily include depression and anxiety.4 Evidence from the Global Burden of Disease study has shown that the prevalence of depressive disorders is 3.7% for adolescents aged 10 to 19 years worldwide, and the prevalence of anxiety disorders is 7.7%.5 Previous research has been established that negative affects in adolescents are closely linked to the emergence of problematic behaviors such as academic procrastination.6 And if negative affect remains unmitigated, this may potentially result in self-injurious behavior among adolescents.7 Therefore, it is essential to address the negative affect experienced by adolescents to prevent these negative feelings from escalating into psychological problem or mental illnesses that could impede their physical and mental development.
Physical Activity and Negative Affect
The Guidelines for Physical Activity and Sedentary Behavior recommend that adolescents engage in at least 60 minutes of moderate-to-vigorous physical activity per day.8 Physical activity refers to any bodily movement produced by skeletal muscles resulting in energy expenditure.9 It can be categorized into exercise (purposeful activity) and non-exercise (lifestyle activity). Specifically, exercise refers to the planned and organized activities involving repetitive body movements aimed at improving or maintaining physical health. In contrast, non-exercise activities (eg, walking to work) do not follow a structured exercise regimen but still constitute a significant component of daily physical activity.
The impact of physical activity on adolescents’ negative affect has attracted considerable attention within the field of sports psychology. Regular physical activity can help mitigate sudden anxiety episodes.10 Numerous early studies have found that exercise significantly reduces levels of depression and anxiety,11 along with physiological responses such as muscle tension associated with anxiety.12 Meta-analyses examining exercise interventions for anxiety have demonstrated that such interventions yield beneficial effects.13 A recent meta-analysis to determine the effects of physical activity on anxiety and depression symptoms in overweight/obese children and adolescents found that physical activity significantly improved depression and anxiety symptoms.14 Similarly, a meta-analysis examining exercise interventions for depression indicated that aerobic exercise is effective in alleviating depressive symptoms and treating depression (SMD = −0.946).15 Even in the absence of exercise activity, non-exercise activity (eg, taking the stairs or cycling) can positively influence affect, particularly among adolescents.9 Research has demonstrated that non-exercise activities are associated with an increase in gray matter volume within key brain regions responsible for mood recovery and regulation, thereby enhancing individuals’ positive emotional experiences.16 Currently, numerous studies are dedicated to developing effective exercise intervention programs aimed at alleviating negative affect.17 A study comparing the effects of physical exercise versus sedentary activities on depression and anxiety among adolescents revealed that after a six-week intervention involving aerobic exercise, participants exhibited significantly reduced symptoms of depression and anxiety.18 However, research exploring the mechanisms through which physical activity affects negative affect remains limited.
The Mediating Role of Sleep Quality
Biological and cognitive theoretical perspectives have been employed to elucidate how physical activity affects emotional regulation.19 The biological perspective posits that physical activity can enhance the production of neurotransmitters such as endorphins and norepinephrine, thus contributing to mood regulation. Some studies have identified a correlation between post-exercise endorphin surges and short-term improvements in mood. However, the relationship between endorphin levels and severity of depression remains unclear. Fluctuation in endorphin secretion level may be a sign for the change in depression level, rather than serving as a precursor to depression.20 The cognitive perspective highlights that physical activity can enhance individuals’ sense of control and self-efficacy, helping them resist negative moods. Research has indicated that emotional regulation, self-efficacy and emotional regulation strategies mediate the relationship between physical activity and depression and anxiety.21 While these theories attempt to elucidate the influence of physical activity on negative affect from physiological and cognitive perspectives, they exhibit certain limitations by overlooking the critical role played by changes in individual behaviors or habits. As a behavioral habit, sleep is crucial for both recovery from stressors and maintenance of overall mental health.22
Physical Activity and Sleep Quality
Sleep quality refers to an individual’s assessment of their sleep condition.23 Engaging in physical activity can help adolescent in enhancing sleep quality and alleviating sleep-related issues. Exercise, recognized as a non-pharmacological intervention for insomnia, has been shown to significantly improve sleep quality in both healthy individuals24 and those with sleep disorders.25 Research indicates that exercise positively influences both sleep efficiency and the severity of insomnia26–28 while also improving self-reported measures of sleep quality.29 A meta-analysis revealed that both single sessions and long-term regular exercise can enhance overall sleep quality and ameliorate insomnia symptoms.30 In addition to exercise, daily activities such as household chores may also lower the risk of developing insomnia and help prevent episodic instances of sleeplessness.31
Physical activity has been shown to ameliorate metabolic diseases linked to circadian rhythm disruptions, including sleep disorders caused by delayed sleep/wake cycles.32 The mechanism by which physical activity contributes to improved sleep can be explained through the circadian rhythm system.33 From a biological theoretical perspective, physical activity stimulates the release of neurotransmitters such as serotonin, which is a precursor to melatonin.34 Thus, physical activity may indirectly support melatonin production and sleep quality. Melatonin, a crucial physiological marker reflecting circadian rhythms, plays an essential role in maintaining a consistent sleep/wake cycle. One study demonstrated that individuals exhibited significantly elevated melatonin levels during moderate-intensity cycling exercise lasting 30 minutes and during the subsequent recovery period, compared to baseline values.35
Sleep Quality and Negative Affect
There exists a close relationship between sleep quality and negative affect, with poor-quality sleep often coexisting with mood disorders. Evidence from both clinical and subclinical populations suggests that poor sleep quality is correlated with elevated levels of negative affect and diminished positive affect.36 A one-month ecological momentary assessment study revealed that variations in sleep quality were significant predictors of changes in negative affect, and improvements in sleep quality led to reductions in negative feelings.37 Early adolescence is a developmental stage marked by an increased prevalence of sleep disturbances and emotional challenges.38 Symptoms associated with depression and anxiety are recognized as some of the most prevalent emotional issues among adolescents.39 Numerous studies have found a significant negative correlation between sleep quality, depression, anxiety and other negative affects.40,41
Based on the findings of previous studies, some scholars have proposed a comprehensive “biopsychosocial” model to explain the potential mechanisms linking adolescent insomnia with anxiety and depression.42 Within this framework, the biological mechanism posits that excessive arousal and insufficient sleep can impair key brain regions, such as the prefrontal cortex, amygdala, and anterior cingulate cortex. This impairment may disrupt emotional responses and regulation.43 The psychological mechanism suggests that individuals suffering from insomnia are prone to experiencing repetitive and intrusive thoughts that reinforce negative cognition, thereby perpetuating negative affect.44 The social mechanisms highlight poor sleep can lead to emotional dysregulation,45 increasing adolescents’ likelihood of peer rejection, thereby diminishing self-worth and amplifying feelings of sadness, hopelessness, and loneliness.
A Network Analysis of the Relationship Between Physical Activity and Negative Affect
Previous studies have primarily employed measurement and intervention methodologies to establish a relationship between physical activity and negative affect18 and utilized latent variable models to describe their relationship. However, specific components contributing to the formation and evolution of this relationship remain unclear. Path analysis can explore the effect of sleep quality on physical activity and negative affect and initially establish the internal mechanism.
Network analysis allows for examination at the level of observed variables (ie, visually representing relationships among specific components),46 thus further enriching existing latent variable models. Network analysis is a methodological approach used to study complex systems by representing them as networks composed of nodes and edges. Nodes are the fundamental units of the network. In psychological research, nodes can represent symptoms (eg, anhedonia). Edges represent the connections or relationships between nodes. Network Structure refers to the overall arrangement of nodes and edges. Additionally, network analysis offers a diverse array of indices for evaluation. For example, the components of a cluster that are most likely to establish connections with other clusters can be identified by calculating the “Bridge Expected Influence”.47 In addition, the network structure comparison test can validate differences among multiple networks and elucidate variations in the node connection patterns within subgroup.48 A recent study used network analysis to explore the relationship between physical activity and affective symptoms during home confinement, and found that higher frequency of physical activity was associated with reduced confinement distress and irritability.49 And through the comparison of network structure between different genders, it was found that physical activity mitigated women’s fatigue and men’s unhappiness.
Therefore, this study integrates path analysis with network analysis to comprehensively and meticulously explore the internal mechanisms that underlying the relationship between physical activity and negative affect. Simultaneously, it aims to provide a theoretical foundation and guidance for the policies aimed at promoting the physical and mental health of adolescents. In summary, the purpose of this study is as follows: (1) to explore the role of sleep quality in the relationship between physical activity and negative affect; (2) from a network analysis perspective, to examine detailed relationships among physical activity, sleep quality, and specific components of negative affect; (3) to ascertain the central position of the nodes within the network by evaluating their expected influence; (4) to identify nodes that serve as bridges connecting different clusters in the network by evaluating the bridge expected influence; (5) to explore structural differences in networks across different genders.
Materials and Methods
Participants
This study employed a cross-sectional design, recruiting 557 students from five classes each in two middle schools located in Zhejiang and Hubei Provinces. A two-stage sampling approach was implemented: convenience sampling at the school level and random sampling at the class level. The sample size was determined based on a factor of twenty times the total number of items in the scales used, which was subsequently doubled to ensure adequate power for gender-based comparisons. Participants met the following inclusion criteria: (1) aged 12–18 years; (2) no psychiatric diagnosis; (3) proficiency in Chinese.
Data Collection
Data collection occurred over a ten-day period from November 11 to 20, 2019, using self-reported questionnaires administered by teachers trained in psychological assessment protocols. To ensure both validity and reliability of the questionnaire, we implemented the following measures: (1) the questionnaire was developed following a comprehensive review of existing literature and previously validated instruments within this field; (2) content validity was established through consultations with a panel of experts who evaluated its relevance, clarity, and comprehensiveness. The questionnaires underwent pre-testing during a pilot study involving 30 participants from a similar demographic group. This process enabled us to identify and rectify any ambiguities or issues within the questionnaire items. The study received ethical approval from the researcher’s institution, and written informed consent was obtained from parents or legal guardians of all participants prior to data collection. Demographic information regarding participants was presented in Table 1.
 |
Table 1 Demographic Information |
Measures
Negative Affect
Negative affect was assessed using the simplified depression scale (PHQ-2)50 and the simplified anxiety scale (GAD-2).51 Both scales consist of two items each (eg, low mood, depression, or hopelessness; feeling uneasy, anxious, or highly stressed) rated on a 4-point scale (0 = never, 3 = nearly every day). The negative affect score is calculated as the average of the two scales, and higher score indicates a greater degree of negative affect.
Sleep Quality
The DSM-5 Level 2 Sleep Disturbance Scale (PROMIS Sleep Disturbance)52 comprises eight items (eg, I had difficulty falling asleep). Less sleep disturbance corresponds to higher sleep quality, so we reverse all the scores. Therefore, higher scores indicate better sleep quality. A five-point scale is employed (1 = none at all to 5 = very much), with higher scores indicating better sleep quality. Since the description of item 1,4,5,6 is sleep disturbance (eg, sleep difficulty), in order to ensure that all items are scored in the same direction, reverse scoring is used.
Physical Activity
Physical activity was measured through two components: exercise and non-exercise activities. The exercise item53 assessed “the number of days within the last seven days during which more than sixty minutes of exercise occurred (excluding physical education classes)”, while the non-exercise item54 assessed “the number of days in the past week that an individual rode a bicycle or walked to and from school”. Both components utilized a five-point scale (1 = no days to 5 = seven days), with the physical activity score being derived from the average of these two items. And higher scores indicated more physical activity.
Statistical Analyses
Initially, SPSS 22.0 was utilized for descriptive statistics and correlation analysis. Furthermore, a mediation analysis was conducted using Model 4 of PROCESS macro.55 The standard error and 95% confidence interval of the parameter estimation were obtained by bootstrapping method (repeated sampling 5000 times).
Subsequently, network analysis was performed on the data. The EBICglasso model was calculated using JASP to estimate the regularized Gaussian graphical model (GGM).56 Specifically, the minimum absolute convergence and selection algorithm (GLASSO)57 was employed with an adjustment parameter set to 0.5. This setting facilitated the removal of relatively weak connections within the network, thereby yielding a structure that enhances predictive accuracy and interpretability. Furthermore, the extended Bayesian Information Criterion (EBIC)58 was utilized for selecting the best-fitting model. In this network, items in the scale were presented as nodes. The Expected Influence (EI) of a node reflected its importance within the network, and higher EI values indicated greater importance. Additionally, the Bridge Expected Influence (BEI) of a node reflected its impact on other clusters in the network, and higher BEI values indicated a more substantial influence on these clusters.59 The correlation between nodes was presented in the form of edges. The thickness of the edge indicated correlation strength. The thicker an edge, the stronger the correlation it indicated. A blue line indicated a positive correlation between two nodes, while a red line indicates a negative correlation between two nodes.
And then, the R-package bootnet60 was utilized to evaluate both accuracy and stability of the network. The stability of the network included both the expected influence stability and the bridge expected influence stability of each node. The accuracy of the edge weights was assessed by calculating bootstrapped 95% confidence interval (1000 repeated samples). Less overlap among confidence intervals of different edge weights corresponded to higher accuracy of the edge weights. The Correlation Stability coefficient (CS coefficient) was calculated to evaluate the EI stability for nodes and bridges. CS coefficient should not fall below 0.25, and values exceeding 0.5 were preferable.60
Finally, the Network Comparison Test package was employed to conduct a network structure invariance test aimed at examining gender differences. The network invariance test was assessed by the differences in the strength of the maximum edge of the network.48
Results
Common Method Biases
Harman’s one-way test was performed to examine common method biases,61 and the result showed that there were four factors with eigenvalues exceeding 1. The first factor accounted for 33.51% of the variance (below 40%), indicating that common method biases were not significant in this study.
Descriptive Statistics and Correlation Analysis
See Table 2.
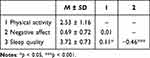 |
Table 2 Means, Standard Deviations and Partial Correlations Among Variables |
Mediation Analysis
The mediation model was evaluated using Model 4 in PROCESS (see Figure 1). Physical activity significantly and positively predicted sleep quality (B = 0.07, SE = 0.03, 95% CI = 0.01–0.12), while sleep quality significantly and negatively predicted negative affect (B = −0.46, SE = 0.04, 95% CI = −0.53–0.38). The relationship between physical activity and negative affect was completely mediated by sleep quality. And the indirect effect size of sleep quality was −0.03 (95% CI = −0.05–0.01).
 |
Figure 1 Mediation model. *p < .05, ***p < .001. |
Network Analysis
The network illustrating how physical activity influences negative affect was presented in Figure 2. The network comprised fourteen nodes and fifty-three (58%) non-zero edges. Notably, both the network of sleep quality and the network of negative affect formed a relatively concentrated cluster, and the internal components were closely connected. The abbreviation for each variable selected in the item-level network were shown in Table S1.
 |
Figure 2 EBICglasso model based on the item-level network analysis. |
Characteristics of Edges
As shown in Table S2, among the clusters, node PA1 (exercise) was positively related to node SQ8 (sleep quality; r = 0.22), followed by the connection between node SQ1 (sleep restfulness) and node NA1 (anhedonia; r = −0.13). In addition, the results from the bootstrap network analysis indicated that the edge weights were relatively accurate and reliable (see Figure S1). For the bootstrap difference test of edge weights, see Figure S2.
Characteristics of Nodes
The expected influence of nodes was shown in Figure 3a. The expected influence of SQ6 (sleep problems), SQ8 (sleep quality), and SQ2 (sleep satisfaction) was higher than that of other nodes, indicating that these three nodes had a higher number of connections to other nodes within the current network. The CS coefficient of expected influence was 0.75 (>0.25), indicating that the expected influence of the nodes was stable (see Figure S3). For the bootstrap difference test of the expected influence, see Figure S4.
 |
Figure 3 Node expected influence (A) and node bridge expected influence (B). |
The bridge expected influence of nodes was shown in Figure 3b. PA1 (exercise) showed a strong association with both negative affect and sleep quality clusters, followed by SQ8 (sleep quality) with both physical activity and negative affect clusters. The CS coefficient of the bridge expected influence was 0.75(>0.25), indicating that the bridge expected influence on the nodes was stable (see Figure S5). For the bootstrap difference test of the bridge expected influence, see Figure S6.
Network Differences Between Genders
There was no significant differences observed in the overall network structure between genders (p = 0.64). The similarity in network structures between boys and girls indicated that the mechanism of physical activity on negative affect might not influence by gender.
Discussion
In this study, mediation analysis and network analysis were employed to investigate the relationship between physical activity and negative affect, as well as the underlying mechanisms involved. The findings indicated that physical activity significantly predicted negative affect, with sleep quality serving as a mediating factor in this relationship. Network analysis further identified key connections, such as the edge between node “exercise” and node “sleep quality” and the edge between node “sleep restfulness” and node “anhedonia”.
The Mechanism of Physical Activity on Negative Affect
This study found that physical activity can alleviate negative affect, which was consistent with the findings from numerous prior studies. Previous studies have established that exercise serves as an effective intervention for depression and anxiety.13,15 Furthermore, non-exercise activities have been shown to alter brain regions associated with emotional processing and enhance individuals’ positive emotional experiences.16
In addition, through mediating analysis, this study revealed that sleep quality played a full mediating role between physical activity and negative affect. A substantial body of research has identified correlations between physical activity and sleep quality as well as sleep quality and negative affect.26 The full mediating effect of sleep quality could be explained as follows.
Emerging evidence suggests that REM sleep disturbances are commonly observed in individuals with depression, including adolescents.44 Previous polysomnographic studies involving depressed patients indicated shortened REM latency, prolonged early-night REM sleep duration, and increased REM density in these individuals.62 Antidepressants were known to decrease REM sleep while increasing REM latency.63 Similar to the effects of antidepressants, physical activity effectively reduced the duration of an individual’s latent sleep period,64 enhanced slow-wave sleep during the sleep cycle,65 and increased total sleep duration.66
In adolescents, whose brains are still undergoing significant developmental changes, these mechanisms may be particularly relevant, as sleep and emotional regulation are closely intertwined during this critical period. The alterations in sleep structure induced by physical activity might represent a potential mechanism for its antidepressant effects. By improving the structure of sleep, physical activity might contribute significantly to mitigating negative affect.
The Mechanism Network of Physical Activity on Negative Affect
Through network analysis, this study identified that the most central node within the network of physical activity and negative affect was SQ6 (sleep problem) in sleep quality. This indicated that “sleep problem” was pivotal in the network and was likely to exert a significant influence on its overall dynamics. Within the network, node PA1 (“exercise”) was most strongly associated with node SQ8 (sleep quality). Furthermore, node SQ1 (sleep restfulness) was closely linked to node NA1 (anhedonia).
Firstly, this study differentiated between various types of physical activities and found that both exercise and non-exercise activities could improve an individual’s subjective sleep quality. However, the impact of exercise was notably more pronounced. These findings are similar to those from ecological momentary assessment studies, indicating that 60 minutes of moderate to vigorous physical activity can significantly improve various indicators of sleep, including subjective assessment of sleep quality and sleep restfulness.67 In addition, these results are consistent with findings related to circadian rhythms,33 as increased levels of melatonin due to physical activity contribute positively towards improved overall sleep quality.
These results suggest that while exercise and non-exercise activities exert independent or additive effects on health outcomes, the positive effect of exercise is greater. Previous studies have indicated that exercise contributes positively to health perception, whereas non-exercise activities related to housework, work, and commuting do not yield similar benefits.68 This underscores that exercise offers unique advantages for health that cannot be substituted by non-exercise activities.
Secondly, restful sleep may reduce the level of anhedonia. The findings are similar to those of previous studies. A network analysis study identified a strong correlation between the core symptom of sleep, “subjective sleep quality”, and the core symptom of depression, “anhedonia”, thereby elucidating the connection between the sleep network and the depression network.69 By incorporating various indicators of sleep quality, this study further found that the improvements in “sleep quality” would promote enhancements in the specific index of “sleep restfulness”, which subsequently reduces levels of “feeling bored”. Previous studies have also established a negative correlation between sleep restfulness and depression, and a higher frequency of restful sleep can mitigate the risk of developing depressive symptoms.22 These results of this study prove that sleep disorders represent a significant risk factor for depression while revealing a potential mechanism through which restful sleep may diminish this risk—specifically by reducing degrees of anhedonia.
Network Differences Between Genders
In this study, the mechanism of physical activity on negative affect did not show statistically significant differences by gender in the current sample. However, the possibility of small effect sizes or gender-related differences that were not detectable in this study cannot be ruled out, and further research with larger samples might be needed to explore this possibility more thoroughly.
Implications
Through conducting mediation analysis and network analysis, this study further explores the potential mechanisms by which physical activity influences negative affect, offering both theoretical value and practical significance. From a theoretical perspective, this study includes sleep quality, and further reveals the relationship between physical activity and negative affect. It is found that exercise can enhance overall sleep quality, and restful sleep can alleviate symptoms associated with anhedonia. These results contribute to our understanding of how physical activity influences negative affect while complementing existing theoretical frameworks (eg “biopsychosocial” model).
In practice, these results hold guiding significance for preventing and intervening in cases of depression and anxiety disorders among adolescents. Firstly, it is necessary to develop scientifically grounded exercise programs tailored specifically for adolescents.17 Adolescents need to increase physical activity, especially purposeful and organized exercise, as a means to mitigate negative affect. At the school and family levels, it is essential to promote the “physical activity for sleep quality” strategy. Additionally, at the policy level, encouraging increased time allocated for physical activities should be prioritized to mitigate negative affect among adolescents. Secondly, ensuring the overall quality of sleep among adolescents is crucial. Enhancing sleep quality serves as an important strategy for preventing depression and other adverse emotional states.69 Therefore, in order to assist teenagers in addressing sleep issues, it is essential to focus on “sleep restfulness” and provide them with a quiet and comfortable sleep environment.
Limitations
Several limitations are present in this study. Firstly, the main limitation is that this study employs a cross-sectional design that does not elucidate the causal relationship between physical activity and negative affect. Longitudinal experimental designs should be utilized in future studies to further investigate how different levels and types of physical activities influence negative affect by using experimental methodologies. Secondly, data were collected via self-reports from students, which may introduce bias due to social desirability effects. Future studies should incorporate additional data collection methods such as electrophysiological techniques—including electroencephalography, event-related potentials, and polysomnography52—as well as ecological momentary assessment67 to capture real-time dynamic changes in data. Finally, this study only considered gender as a demographic variable while neglecting the potential impacts of environmental and cognitive factors on negative affect. Future research could benefit from integrating psychological and environmental factors into a unified framework to further explore the effect of physical activity on negative affect.
Conclusions
This study investigated the relationship between physical activity and negative affect, emphasizing the mediating role of sleep quality. Through network analysis, we also explored the mechanistic pathways by which physical activity influences negative affect. The following conclusions were drawn from this study:
(1) Physical activity may alleviate negative affect through enhancements in sleep quality. Participation in physical activities, whether exercise or non-exercise activities, can lead to better sleep quality, which subsequently mitigates negative affect.
(2) Both exercise and non-exercise activities contribute to enhanced sleep quality and a reduction in anhedonia. Within the proposed mechanistic framework, these activities promote improved sleep restfulness and lower levels of anhedonia, a core symptom of depression.
(3) Exercise exerts a more pronounced positive effect compared to non-exercise activities. In contrast to non-exercise activities, exercise demonstrates a significantly greater impact on improving sleep quality and reducing negative affect. This finding highlights the importance of tailored exercise programs and organized physical activity initiatives for adolescents. By promoting physical activity, particularly structured exercise, we can potentially alleviate mental health challenges within this demographic.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Ethics Statements
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institute of Psychological and Brain Sciences, Zhejiang Normal University.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Arnett JJ. Adolescent storm and stress, reconsidered. Am Psychol. 1999;54(5):317–326. doi:10.1037/0003-066X.54.5.317
2. Lei Y, Mei Y, Wang J, Yuan Z. Identifying the impact of unconscious fear on adolescent anxiety: cognitive neural mechanisms and interventions. Adv Psychol Sci. 2024;32(8):1221–1232. doi:10.3724/SP.J.1042.2024.01221
3. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Personal Soc Psychol. 1988;54(6):1063–1070. doi:10.1037/0022-3514.54.6.1063
4. Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta‐analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psych. 2015;56(3):345–365. doi:10.1111/jcpp.12381
5. Kieling C, Buchweitz C, Caye A, et al. Worldwide prevalence and disability from mental disorders across childhood and adolescence: evidence from the global burden of disease study. JAMA Psychiatry. 2024;81(4):347–356. doi:10.1001/jamapsychiatry.2023.5051
6. Yeo SN, Zainal H, Tang CS, Tong EM, Ho CS, Ho RC. Success/failure condition influences attribution of control, negative affect, and shame among patients with depression in Singapore. BMC Psychiatry. 2017;17(1):285. doi:10.1186/s12888-017-1451-7
7. Bresin K, Gordon KH, Bender TW, Gordon LJ, Joiner TE. No pain, no change: reductions in prior negative affect following physical pain. Motivation Emotion. 2010;34(3):280–287. doi:10.1007/s11031-010-9168-7
8. WHO Guidelines on Physical Activity and Sedentary Behaviour. Geneva: World Health Organization; 2020.
9. Bouça-Machado R, Rosário A, Caldeira D, et al. Physical activity, exercise, and physiotherapy in parkinson’s disease: defining the concepts. Mov Disord Clin Pract. 2019;7(1):7–15. doi:10.1002/mdc3.12849
10. Schuch FB, Stubbs B, Meyer J, et al. Physical activity protects from incident anxiety: a meta‐analysis of prospective cohort studies. Depression Anxiety. 2019;36(9):846–858. doi:10.1002/da.22915
11. Sexton H, Mære A, Dahl NH. Exercise intensity and reduction in neurotic symptoms: a controlled follow-up study. Acta Psychiatrica Scandinavica. 1989;80(3):231–235. doi:10.1111/j.1600-0447.1989.tb01332.x
12. Petruzzello SJ, Landers DM, Hatfield BD, Kubitz KA, Salazar W. A meta-analysis on the anxiety-reducing effects of acute and chronic exercise. Outcomes and mechanisms. Sports Med. 1991;11(3):143–182. doi:10.2165/00007256-199111030-00002
13. Wipfli BM, Rethorst CD, Landers DM. The anxiolytic effects of exercise: a meta-analysis of randomized trials and dose-response analysis. J Sport Exercise Psychol. 2008;30(4):392–410. doi:10.1123/jsep.30.4.392
14. Chen L, Liu Q, Xu F, et al. Effect of physical activity on anxiety, depression and obesity index in children and adolescents with obesity: a meta-analysis. J Affective Disorders. 2024;354:275–285. doi:10.1016/j.jad.2024.02.092
15. Heissel A, Heinen D, Brokmeier LL, et al. Exercise as medicine for depressive symptoms? A systematic review and meta-analysis with meta-regression. Br J Sports Med. 2023;57(16):1049–1057. doi:10.1136/bjsports-2022-106282
16. Reichert M, Braun U, Gan G, et al. A neural mechanism for affective well-being: subgenual cingulate cortex mediates real-life effects of nonexercise activity on energy. Sci Adv. 2020;6(45):eaaz8934. doi:10.1126/sciadv.aaz8934
17. Hill MD, Gibson A-M, Wagerman SA, Flores ED, Kelly LA. The effects of aerobic and resistance exercise on state anxiety and cognitive function. Sci Sports. 2019;34:216–221. doi:10.1016/j.scispo.2018.09.004
18. Philippot A, Dubois V, Lambrechts K, et al. Impact of physical exercise on depression and anxiety in adolescent inpatients: a randomized controlled trial. J Affective Disorders. 2022;301:145–153. doi:10.1016/j.jad.2022.01.011
19. Chen Z, Ji L. A Review of the mechanisms of the effects of physical exercise on emotion regulation. Psychol Sci. 2003;26(04):737–740.
20. Brosse AL, Sheets ES, Lett HS, Blumenthal JA. Exercise and the treatment of clinical depression in adults: recent findings and future directions. Sports Med. 2002;32(12):741–760. doi:10.2165/00007256-200232120-00001
21. Jiang Y, Zhang L, Mao J. Physical exercise and mental health: the effect of emotion regulation self-efficacy and emotion regulation strategy. Study Psychol Behav. 2018;16(04):570–576.
22. Rosso AC, Wilson OWA, Papalia Z, Duffey M, Kline CE, Bopp M. Frequent restful sleep is associated with the absence of depressive symptoms and higher grade point average among college students. Sleep Health. 2020;6(5):618–622. doi:10.1016/j.sleh.2020.01.018
23. Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9–17. doi:10.5665/sleep.3298
24. Kovacevic A, Mavros Y, Heisz JJ, Singh MAF. The effect of resistance exercise on sleep: a systematic review of randomized controlled trials. Sleep Med Rev. 2018;39:52–68. doi:10.1016/j.smrv.2017.07.002
25. Fan B, Song W, Zhang J, et al. The efficacy of mind-body (Baduanjin) exercise on self-reported sleep quality and quality of life in elderly subjects with sleep disturbances: a randomized controlled trial. Sleep Breathing. 2020;24(2):695–701. doi:10.1007/s11325-019-01999-w
26. Passos GS, Poyares D, Santana MG, Garbuio SA, Tufik S, Mello MT. Effect of acute physical exercise on patients with chronic primary insomnia. J Clin Sleep Med. 2010;6(3):270–275.
27. Reid KJ, Baron KG, Lu B, Naylor E, Wolfe L, Zee PC. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med. 2010;11(9):934–940. doi:10.1016/j.sleep.2010.04.014
28. Hartescu I, Morgan K, Stevinson CD. Increased physical activity improves sleep and mood outcomes in inactive people with insomnia: a randomized controlled trial. J Sleep Res. 2015;24(5):526–534. doi:10.1111/jsr.12297
29. Park H, Suh B. Association between sleep quality and physical activity according to gender and shift work. J Sleep Res. 2020;29(6):e12924. doi:10.1111/jsr.12924
30. Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38(3):427–449. doi:10.1007/s10865-015-9617-6
31. Morgan K. Daytime activity and risk factors for late-life insomnia. J Sleep Res. 2003;12(3):231–238. doi:10.1046/j.1365-2869.2003.00355.x
32. Gabriel BM, Zierath JR. Circadian rhythms and exercise - re-setting the clock in metabolic disease. Nat Rev Endocrinol. 2019;15(4):197–206. doi:10.1038/s41574-018-0150-x
33. Zhou Z, Liu F, Sun L, Ren Z, Li R. The effect of physical activity on sleep quality in children with ADHD. China Sport Sci Technol. 2023;59(9):26–32.
34. Basso JC, Suzuki WA. The effects of acute exercise on mood, cognition, neurophysiology, and neurochemical pathways: a review. Brain Plast. 2017;2(2):127–152. doi:10.3233/BPL-160040
35. Marrin K, Drust B, Gregson W, Morris CJ, Chester N, Atkinson G. Diurnal variation in the salivary melatonin responses to exercise: relation to exercise-mediated tachycardia. Eur J Appl Physiol. 2011;111(11):2707–2714. doi:10.1007/s00421-011-1890-7
36. Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: a focus on insomnia. Sleep Med Rev. 2010;14(4):227–238. doi:10.1016/j.smrv.2009.10.007
37. Bouwmans MEJ, Bos EH, Hoenders HJR, Oldehinkel AJ, de Jonge P. Sleep quality predicts positive and negative affect but not vice versa. An electronic diary study in depressed and healthy individuals. J Affective Disorders. 2017;207:260–267. doi:10.1016/j.jad.2016.09.046
38. Kelly RJ, El-Sheikh M. Reciprocal relations between children’s sleep and their adjustment over time. Dev psychol. 2014;50(4):1137–1147. doi:10.1037/a0034501
39. Rapee RM, Oar EL, Johnco CJ, et al. Adolescent development and risk for the onset of social-emotional disorders: a review and conceptual model. Behav Res Ther. 2019:123. doi:10.1016/j.brat.2019.103501.
40. Amaral AP, Soares MJ, Pinto AM, et al. Sleep difficulties in college students: the role of stress, affect and cognitive processes. Psychiatry Res. 2018;260:331–337. doi:10.1016/j.psychres.2017.11.072
41. Seun-Fadipe CT, Mosaku KS. Sleep quality and psychological distress among undergraduate students of a Nigerian university. Sleep Health. 2017;3(3):190–194. doi:10.1016/j.sleh.2017.02.004
42. Blake MJ, Trinder JA, Allen NB. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: implications for behavioral sleep interventions. Clinic Psychol Rev. 2018;63:25–40. doi:10.1016/j.cpr.2018.05.006
43. Chuah LYM, Dolcos F, Chen AK, Zheng H, Parimal S, Chee MWL. Sleep deprivation and interference by emotional distracters. Sleep. 2010;33(10):1305–1313. doi:10.1093/sleep/33.10.1305
44. Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev. 2014;18(6):521–529. doi:10.1016/j.smrv.2014.03.006
45. Palmer CA, Alfano CA. Sleep and emotion regulation: an organizing, integrative review. Sleep Med Rev. 2017;31:6–16. doi:10.1016/j.smrv.2015.12.006
46. Cai Y, Dong S, Yuan S, Hu C. Network analysis and its applications in psychology. Adv Psychol Sci. 2020;28(1):178–190. doi:10.3724/SP.J.1042.2020.00178
47. Robinaugh DJ, Hoekstra RHA, Toner ER, Borsboom D. The network approach to psychopathology: a review of the literature 2008–2018 and an agenda for future research. Psychol Med. 2020;50(3):353–366. doi:10.1017/S0033291719003404
48. van Borkulo C, Boschloo L, Borsboom D, Bwjh P, Waldorp LJ, Schoevers RA. Association of symptom network structure with the course of longitudinal depression. JAMA Psychiatry. 2015;72(12):1219–1226. doi:10.1001/jamapsychiatry.2015.2079
49. Cecchini JA, Carriedo A, Méndez-Giménez A, Fernández-Río J, Carriedo A. Network analysis of physical activity and depressive and affective symptoms during COVID-19 home confinement. Global Mental Health. 2023;10. doi:10.1017/gmh.2023.57
50. Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosomatic Res. 2005;58(2):163–171. doi:10.1016/j.jpsychores.2004.09.006
51. Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Internal Med. 2007;146(5):317–325. doi:10.7326/0003-4819-146-5-200703060-00004
52. Buysse DJ, Yu L, Moul DE, et al. Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep. 2010;33(6):781–792. doi:10.1093/sleep/33.6.781
53. Zhao X, Lai X, Huang S, et al. Long-term protective effects of physical activity and self-control on problematic smartphone use in adolescents: a longitudinal mediation analysis. Mental Health Phys Act. 2024;26:1–9. doi:10.1016/j.mhpa.2024.100585
54. Donnelly JE, Blair SN, Jakicic JM, et al. American college of sports medicine position stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exercise. 2009;41(2):459–471. doi:10.1249/MSS.0b013e3181949333
55. Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. 2018.
56. Costantini G, Epskamp S, Borsboom D, et al. State of the aRt personality research: a tutorial on network analysis of personality data in R. J Res Personality. 2015;54:13–29. doi:10.1016/j.jrp.2014.07.003
57. Friedman J, Hastie T, Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9(3):432–441. doi:10.1093/biostatistics/kxm045
58. Chen J, Chen Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. 2008;95(3):759–771. doi:10.1093/biomet/asn034
59. Jones PJ, Ma R, McNally RJ. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav Res. 2021;56(2):353–367. doi:10.1080/00273171.2019.1614898
60. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Meth. 2018;50(1):195–212. doi:10.3758/s13428-017-0862-1
61. Podsakoff PM, MacKenzie SB, Lee J-Y, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88(5):879–903. doi:10.1037/0021-9010.88.5.879
62. Riemann D, Berger M, Voderholzer U. Sleep and depression—Results from psychobiological studies: an overview. Biol psychol. 2001;57(1–3):67–103. doi:10.1016/S0301-0511(01)00090-4
63. Wilson S, Argyropoulos S. Antidepressants and sleep: a qualitative review of the literature. Drugs. 2005;65(7):927–947. doi:10.2165/00003495-200565070-00003
64. Arias P, Madinabeitia-Mancebo E, Santiago M, Corral-Bergantinos Y, Robles-Garcia V. Effects of early or late-evening fatiguing physical activity on sleep quality in non-professional sportsmen. J Sports Med Phys Fitness. 2016;56(5):597–605.
65. Bulckaert A, Exadaktylos V, Haex B, De Valck E, Verbraecken J, Berckmans D. Elevated variance in heart rate during slow-wave sleep after late-night physical activity. Chronobiol Int. 2011;28(3):282–284. doi:10.3109/07420528.2011.552820
66. Pinniger R, Thorsteinsson EB, Brown RF, McKinley P. “Tango dance can reduce distress and insomnia in people with self-referred affective symptoms”: correction. Am J Dance Ther. 2020;42(1):143–144. doi:10.1007/s10465-019-09319-1
67. Zapalac K, Miller M, Champagne FA, Schnyer DM, Baird B. The effects of physical activity on sleep architecture and mood in naturalistic environments. Sci Rep. 2024;14(1):5637. doi:10.1038/s41598-024-56332-7
68. Lera-López F, Ollo-López A, Sánchez-Santos JM. How does physical activity make you feel better? The mediational role of perceived health. Appl Res Qual Life. 2017;12(3):511–531. doi:10.1007/s11482-016-9473-8
69. Zhang X, Yang Y, Lei H, Dong D, Feng Z. Network analysis of the relationship between sleep problems and depressive symptoms in adolescents. Chin J Clin Psychol. 2024;32(4):824–830.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

