Back to Journals » Journal of Inflammation Research » Volume 17
The Pan-Immune Inflammation Value at Admission Predicts Postoperative in-hospital Mortality in Patients with Acute Type A Aortic Dissection
Authors Yu X, Chen Y, Peng Y, Chen L, Lin Y
Received 8 March 2024
Accepted for publication 25 June 2024
Published 5 August 2024 Volume 2024:17 Pages 5223—5234
DOI https://doi.org/10.2147/JIR.S468017
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Ning Quan
Xijing Yu,1,* Yaqin Chen,1,* Yanchun Peng,2 Liangwan Chen,3,4 Yanjuan Lin2,3
1School of Nursing, Fujian Medical University, Fuzhou, Fujian, People’s Republic of China; 2Department of Nursing, Fujian Medical University Union Hospital, Fuzhou, Fujian, People’s Republic of China; 3Department of Cardiac Surgery, Fujian Medical University Union Hospital, Fuzhou, Fujian, People’s Republic of China; 4Key Laboratory of Cardio-Thoracic Surgery, Fujian Medical University, Fuzhou, Fujian, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yanjuan Lin, Department of Nursing, Union Hospital, Fujian Medical University, No. 29 Xinquan Road, Fuzhou, Fujian Province, 350001, People’s Republic of China, Tel +86059186218336, Fax +86059183344034, Email [email protected] Liangwan Chen, Department of Cardiac Surgery, Union Hospital, Fujian Medical University, No. 29 Xinquan Road, Fuzhou, Fujian Province, 350001, People’s Republic of China, Tel +86059186218336, Fax +86059183301393, Email [email protected]
Purpose: The inflammatory response of the body is intimately linked to the quick onset and high in-hospital mortality of Acute Type A Aortic Dissection (ATAAD). The purpose of the study was to examine the connection between in-hospital mortality in patients with ATAAD upon admission and the Pan-Immune-Inflammation Value (PIV).
Patients and Methods: 308 patients who were diagnosed with ATAAD between September 2018 and October 2021 at Fujian Provincial Center for Cardiovascular Medicine had their clinical data retrospectively examined. PIV was assessed at the time of study population admission, with in-hospital mortality serving as the main outcome measure. Patients were divided into two groups, the high PIV group (PIV > 1807.704) and the low PIV group (PIV < 1807.704), based on the PIV ROC curve and the best threshold of the Youden index. The clinical results of the two groups were then compared.
Results: Among ATAAD patients, postoperative in-hospital mortality was higher in the high PIV group (54.7% vs 10.6%, P < 0.001), and the high PIV group had significantly higher rates of postoperative acute kidney injury, acute liver insufficiency, and gastrointestinal hemorrhage (P < 0.05). Additionally, the high PIV group’s ICU stays lasted longer than the low PIV group’s (P < 0.05). The results of multifactorial logistic regression analysis, which controlled for other variables, indicated that the mechanical ventilation time (OR = 1.860, 95% CI: 1.437, 2.408; P < 0.001), the high PIV group (> 1807.704) (OR = 1.939, 95% CI: 1.257, 2.990; P = 0.003), the cardiopulmonary bypass time (OR = 1.011, 95% CI: 1.004, 1.018; P = 0.002), and the white blood cell count (OR = 1.188, 95% CI: 1.054, 1.340; P = 0.005) were independent risk factors for postoperative in-hospital mortality in ATAAD patients.
Conclusion: Postoperative death in ATAAD patients was independently predicted by high PIV levels at admission. Patients should be informed about their preoperative inflammatory status and actively participate in prompt clinical decision-making and treatment.
Keywords: Acute Type A Aortic Dissection, the Pan-Immune-Inflammation Value, Inflammation, Cardiac surgery, In-hospital mortality
Introduction
Acute Type A Aortic Dissection (ATAAD) is a condition that is associated with a high mortality rate and severe comorbidities, necessitating immediate surgical intervention.1 ATAAD is characterized by a tear in the aortic intima forming a fissure through which blood gushes out, resulting in the separation of the inner and middle layers of the aorta and the formation of a false lumen.2 ATAAD can result in fatality if blood penetrates the aortic wall and leads to hemorrhaging.3 Individuals suffering from ATAAD primarily exhibit neurological symptoms related to reduced blood flow to the brain. Additionally, they frequently encounter abrupt and intense pain in the chest, back, and abdomen.4 Recently, the survival rate of patients with ATAAD has greatly improved due to the use of effective therapeutic options such as Bentall surgery and the frozen elephant trunk approach. However, the prognosis for these patients remains unfavorable, with in-hospital mortality rates ranging from 9% to 30%.4–6 It is clinically significant to predict the risk of postoperative mortality in patients with ATAAD and develop measures to reduce postoperative mortality and decrease the number of deaths in these patients. Owing to the significant variation in the clinical outcomes of patients with ATAAD, precise risk assessment can impact subsequent clinical decisions (such as selecting the surgical procedure type) and the judicious use of healthcare resources (such as medication).4,7 Therefore, prompt identification and immediate intervention can be beneficial. Timely identification of high-risk patients can help improve the overall prognosis of ATAAD patients.
Recently, numerous scholars have utilized biomarkers as precise and measurable indicators for diagnosing and predicting outcomes, such as the OPG/TRAIL ratio and α-2-MG. These biomarkers are crucial in developing risk prediction models and stratifying high-risk patients.8,9 Nevertheless, attaining the intended prediction using the evaluation instruments offered by a solitary biomarker is challenging.10 Simultaneously, healthcare providers do not prioritize using this test due to its drawbacks, including its expensive nature and the difficulty in obtaining specimens. While the exact cause of ATAAD is not yet understood, research has shown that inflammatory factors play varying roles in the medial degeneration of different sections of the aortic wall.11 The increase in systemic inflammation serves as an additional indicator of the seriousness of ATAAD. Several readily identifiable blood immuno-inflammatory biomarkers, including neutrophils, platelets, and monocytes, have been discovered in patients with ATAAD. These biomarkers hold significant value in predicting the clinical outcome of patients with ATAAD.12–15 Therefore, it is necessary to identify appropriate prognostic indicators to better predict the prognosis of patients and to improve the survival of ATAAD patients.
Research has demonstrated that hematologic characteristics, particularly the quantities of lymphocytes and monocytes, can serve as reliable biomarkers for assessing inflammation.16 Recently, there has been notable progress in the research of immune-inflammatory biomarkers that are pertinent to cardiovascular well-being. These biomarkers have exceeded the traditional biomarkers linked to cardiovascular health.17 A novel indicator called the Pan-Immune-Inflammation Value (PIV) has been developed to assess the extent of inflammation. It can serve as a biomarker to forecast the prognosis of various malignancies, such as colorectal, breast, and prostate cancers.17–19 Platelets, neutrophils, monocytes, and lymphocytes are all quantitatively assessed during the PIV technique. Compared with other single inflammation indicators or commonly used inflammation indices such as SII, PLR, and NLR, PIV integrates blood cell populations that are more comprehensively assessed in routine evaluations and can reflect the overall state of systemic inflammation.17,19–21 Among the several measures of inflammation, the SII bears the closest resemblance to the PIV. Research has indicated that the PIV exhibits superior prediction accuracy compared to the SII, potentially because it incorporates monocytes. Monocytes possess significant prognostic significance in predicting the prognosis of ATAAD. Based on our current understanding, it is important to explore the complex pathological pathways that connect the body’s immune response, inflammation, and the development of ATAAD. Hence, it is imperative to establish more inclusive immune-inflammatory markers to accurately forecast patient prognosis and enhance survival rates among individuals with ATAAD.
Currently, there is no documented correlation between PIV readings upon admission and surgical mortality in patients with ATAAD. This study retrospectively reviewed the clinical data from 308 patients who received surgical treatment for ATAAD. The aim was to investigate the correlation between admission PIV and postoperative mortality in ATAAD patients. The findings of this study can provide a valuable basis for making clinical decisions.
Methods
Participants
The study comprised a retrospective analysis of 308 patients diagnosed with ATAAD between September 2018 and October 2021 at Union Hospital of Fujian Medical University. The diagnostic criteria for ATAAD were established based on the findings of computed tomography angiography (CTA) and magnetic resonance imaging (MRI) exams. In the case of patients identified with ATAAD using CTA, the most common surgical approach is the implantation of a modified triple-branched stent graft for descending aorta replacement. This operation is often performed in 90% of ATAAD patients, along with the Bentall procedure.
The inclusion criteria encompassed adult patients, aged 18 years or older, who were undergoing surgery for ATAAD. The exclusion criteria for this study are as follows: (1) patients with diseases that impact the initial counts of blood cell populations and/or in-hospital mortality, such as malignancies, hematologic diseases, and infectious diseases; (2) patients with severe dysfunction of organs, such as hepatic or renal failure; (3) patients taking medications that may influence the parameters of the complete blood count; (4) patients with suspected sub-clinical involvement of the myocardium (such as chronic inflammatory conditions or a history of acute infections); (5) patients utilizing IABP; (6) patients with incomplete clinical data.
Ultimately, a total of 308 patients were included in the study. The medical records were used to gather the fundamental clinical features, imaging findings, surgery data, and clinical outcomes of the subjects. The study was approved by the Ethics Committee of Fujian Medical University Union Hospital (No. 2020KY082). Consent was gained from all subjects and their legal guardians after providing them with relevant information. This study was a retrospective observational analysis of informed consent according to the principles outlined in the Declaration of Helsinki. We guaranteed the confidentiality and anonymity of all patient data, which were exclusively utilized for data analysis purposes. Figure 1 illustrates the procedure of including patients.
 |
Figure 1 Study design and groups. |
Procedures
During the surgical procedure, patients underwent a median sternotomy, and a cardiopulmonary bypass (CPB) was established by inserting two venous cannulas into the right atrium and two arterial return cannulas in the femoral and right axillary arteries. After establishing access to extracorporeal circulation, cold blooded cardioplegia fluid is injected directly into the coronary orifices for cardiac arrest and myocardial protection. When the temperature in the nasopharynx reached 25–28°C, the circulation was halted and blood flow to the brain was redirected by a cannula implanted in the right axillary artery (flow rate, 10 mL·kg−1·min−1, temperature 20°C). While inserting and securing the altered three-branch stent graft, the retrograde cerebral perfusion was temporarily stopped. The perfusion cannula was inserted into the left common carotid artery through its lateral stent to provide bilateral retrograde brain perfusion. Through the transverse incision of the aorta, the main tube graft is implanted into the true lumen of the arch and proximal descending aorta, and then each lateral brachiocephalic tube graft is placed correspondingly into the corresponding arch vessel. Finally, the arch stent graft is placed proximal to the main tube graft and sutured to complete the total aortic arch replacement. After the surgery, the patient’s systemic circulation was restored and they were rewarmed. All patients included in the study underwent identical surgical therapy, and there were no significant differences in the parameters related to total aortic arch replacement, cerebral protection methods, and aortic cannulation type.
Data Collection
Examine electronic medical records to collect and record clinical information about patients in a retrospective manner. The pertinent patient information, such as age, gender, hypertension, coronary artery disease, and smoking status, was recorded. In addition, venous blood samples were obtained to evaluate lactate levels, hemoglobin levels, neutrophil count, and lymphocyte count. The demographic, medical, and laboratory data were acquired from the hospital database.
Variables
PIV was calculated using the following formula: PIV = neutrophil count (109/L) × monocyte count (109/L) × platelet count (109/L) / lymphocyte count (109/L).19 The aforementioned blood cell population counts were acquired from the initial blood test conducted upon admission to the hospital. The main objective of this study was to determine the rate of death occurring within the hospital. Other outcomes of interest included various complications that occurred after surgery while the patient was still in the hospital, such as gastrointestinal hemorrhage, acute kidney injury, acute liver failure, MODS, stroke, and neurological complications. Additionally, the length of stay in the intensive care unit (ICU) and the duration of mechanical ventilation were also documented. Acute kidney injury is characterized by a rise in Serum Creatinine (SCr) of at least 0.3 mg/dL within 48 hours after surgery or an increase in creatinine to at least 1.5 times the baseline level within 7 days after surgery.22 Acute liver failure was characterized as having a MELD score greater than 12 after surgery. The MELD score was computed with the subsequent standardized formula: The MELD score can be calculated using the following formula: MELD score = 11.2 multiplied by the natural logarithm of the international normalized ratio (INR), plus 3.78 multiplied by the natural logarithm of the serum total bilirubin in milligrams per deciliter (mg/dL), plus 9.57 multiplied by the natural logarithm of SCr in mg/dL, and finally adding 6.43. During the initial 24-hour period after surgery, postoperative liver failure was defined using the highest MELD score.23 MODS is characterized by the simultaneous dysfunction of two or more organs, including the respiratory, cardiovascular, cerebrovascular, renal, hepatic, gastrointestinal, hematologic, and central neurological systems. This dysfunction can occur either after surgery or at the time of hospital discharge.24,25
Statistical Analysis
The statistical analysis was conducted using IBM SPSS® 26.0. Continuous variables that followed a normal distribution were represented as mean ± standard deviation (Mean ± SD), while non-normally distributed data were represented as median (P25, P75). Count variables are represented as either frequencies or percentages. The Student’s t-test was used to compare regularly distributed continuous variables between groups, whereas the Mann–Whitney U-test was employed to examine information on continuous variables that did not adhere to normal distribution. The chi-square test or Fisher exact test was used to compare count data between different groups. The Youden index and optimal threshold for PIV for all-cause mortality were determined by computing the Receiver Operating Characteristic Curve (ROC) and selecting the threshold that maximizes the sum of sensitivity and specificity. Initially, univariate logistic regression analysis was used to determine the potential risk factors for in-hospital mortality (P < 0.1), and then multivariate logistic regression analysis was used to confirm that the previously significant variables were independent factors (P < 0.05).
Results
Baseline Characterization
This study included a cohort of 355 patients diagnosed with ATAAD between September 2018 and October 2021. After eliminating 2 patients with incomplete data and 45 patients who did not have surgery, a total of 308 patients were included in the analysis. Among these patients, 255 survived while 53 died. According to the data presented in Figure 1, the death rate among patients with ATAAD was 18.1%. The population consisted of 238 individuals (77.3%) who were male and 70 individuals (22.7%) who were female. The median age of the population was 54 years, with a range of 45 to 62 years.
Sensitivity and Specificity of PIV at Admission
PIV is a reliable indicator of in-hospital death in patients with ATAAD. The area under the receiver operating characteristic curve (AUC) was 0.732 (95% CI: 0.651, 0.813; P < 0.001). The best cutoff value was determined to be 1807.704, with a sensitivity of 51.8% and a specificity of 90.5%. Figure 2 displays the ROC curve.
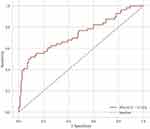 |
Figure 2 Cut-off of PIV for all caused mortality. PIV, the Pan-Immune-Inflammation Value. |
Relationship Between Various PIV Groups and Preoperative Clinical Features
The fundamental attributes of PIV, categorized according to the ROC threshold, are presented in Table 1 and Table 2. The PIV cutoff value was 1807.704. Statistical analysis of neutrophil counts, leukocyte counts, platelet counts, lactate levels, urea levels, serum creatinine levels, and PIV showed a significant difference (P < 0.05) between the two groups. There was no statistically significant difference seen in the comparison of hemoglobin and albumin levels between the two groups.
 |
Table 1 Preoperative Baseline Data of Patients Grouped Between the Survivors and Non-Survivors (n = 308) |
 |
Table 2 Preoperative Laboratory Test Data of the Patients Grouped by PIV (n = 308) |
Relationship Between Various PIV Groups and Intraoperative Clinical Features
Table 3 demonstrates that there was a statistically significant difference (P = 0.009) in operative time, aortic block time, and mechanical ventilation time between the high and low PIV groups. However, there was no statistically significant difference (P > 0.05) in cardiopulmonary bypass (CPB) time between the high and low PIV groups.
 |
Table 3 The Clinical Data of Intraoperative Patients Were Grouped by PIV (n = 308) |
Relationship Between Various PIV Groups and Postoperative Clinical Features
Table 4 demonstrates that the high PIV group had a larger in-hospital mortality rate compared to the low PIV group (54.7% vs 10.6%, P < 0.001). Additionally, the high PIV group had a greater likelihood of experiencing acute kidney injury, acute liver failure, and gastrointestinal hemorrhage following surgery (P < 0.001). The duration of ICU stays for patients in the high PIV group was considerably longer compared to the low PIV group, and this difference was statistically significant (P < 0.05). There was no statistically significant difference in the occurrence of cerebral infarction and MODS between the two groups (P > 0.05).
 |
Table 4 In-Hospital Outcomes After ATAAD Surgery Were Grouped by PIV (N= 308) |
Results of Multivariate Logistic Regression Analysis
Table 5 demonstrates the utilization of logistic regression to further examine the independent risk factors associated with postoperative in-hospital mortality in patients with ATAAD. Univariate logistic regression analysis revealed that several factors, including PIV on admission, hypertension, CPB time, duration of mechanical ventilation, white blood cell (WBC) count, albumin, and urea, were significantly associated with in-hospital mortality (P < 0.1). These findings suggest that these factors may serve as risk factors for postoperative in-hospital mortality in patients with ATAAD. Following a multivariate logistic regression analysis, the findings indicated that several factors were independently associated with an increased risk of postoperative in-hospital mortality in patients with ATAAD. These factors included a high PIV (> 1807.704) at admission (OR = 1.939; 95% CI: 1.257, 2.990; P = 0.003), prolonged mechanical ventilation (OR = 1.860; 95% CI: 1.437, 2.408; P < 0.001), extended duration of cardiopulmonary bypass (OR = 1.011; 95% CI: 1.004, 1.018; P = 0.002), and elevated white blood cell count (OR = 1.194; 95% CI: 1.058, 1.348; P = 0.004).
 |
Table 5 Determine the Risk Factors of in-Hospital Mortality by Logistic Regression Analysis (n = 308) |
Discussion
ATAAD is a life-threatening cardiac condition. The preferred approach for treating ATAAD is immediate surgical intervention.26 Timely detection of risk factors in individuals with ATAAD has the potential to significantly decrease their mortality risk. This study examines the potential correlation between the presence of PIV during admission and the mortality rate in patients with ATAAD undergoing surgical procedures. It is the first study to investigate this relationship. The results of the multivariate logistic regression analysis indicate that patients diagnosed with ATAAD who had a high PIV at the time of admission were more likely to experience postoperative death in the hospital. Upon considering additional variables, it was discovered that a high PIV maintained a substantial association with patient mortality following surgery for ATAAD (P < 0.05).
The study found that the mortality rate of postoperative patients following ATAAD was 18.1%, which aligns with the findings of earlier studies.4,27 At present, several risk factors, including older age, acute renal failure, prolonged extracorporeal circulation, pericardial tamponade, and shock, have been identified as independent factors that increase the risk of in-hospital mortality after surgery in patients with ATAAD, but these factors still do not meet the needs of clinical practice.4,28 Efforts are underway to identify uncomplicated, economical, and effective biomarkers that can better forecast unfavorable outcomes in patients with ATAAD, while also reducing the financial burden of diagnostic testing for patients. Research has indicated that certain immuno-inflammatory indicators, such as high-sensitivity CRP and D-dimer, might predict mortality in patients with ATAAD. These markers are frequently linked to a negative prognosis and their levels stay high even after entrapment correction.29 The prognostic value of prognosis is necessarily limited by the intricate interactions between ATAAD and the immune-inflammatory response, which are not adequately captured by metrics based on simple calculations.
Research has indicated that ATAAD is a condition characterized by inflammation and abnormalities in the coagulation system, resulting from multiple variables. The inflammatory response and the formation of blood clots are significant contributors to the progression of ATAAD.30 The presence of inflammation in the body is strongly linked to the occurrence of ATAAD. The use of CPB, surgical procedures, and anesthetic drugs also stimulate and release pro-inflammatory substances, which worsen the inflammatory response of the epithelium following ATAAD episodes. This can increase the risk of aorta entrapment and rupture, leading to systemic inflammatory response syndrome (SIRS) or even MODS.12,30 Studies have shown that platelet counts are associated with poor cardiovascular prognosis.31,32 ATAAD can trigger SIRS, leading to a condition characterized by extensive inflammation throughout the body. This response can immediately initiate platelet activation, leading to a subsequent elevation in platelet count. Platelets aggregate and cling to the damaged cells lining the arteries, leading to the secretion of various chemicals and the recruitment of inflammatory cells such as monocytes. This procedure exacerbates the inflammatory response and leads to the onset of acute cardiovascular events.10 Platelets cause inflammation through eosinophil recruitment and activation, activate neutrophils and monocytes, and promote lymphocyte migration to peripheral lymph nodes.33,34 This series of inflammatory responses accelerate the degradation of the extracellular matrix, leading to programmed cell death and a decrease in vascular smooth muscle cells. The infiltration and activation of immune cells within the aorta wall intensify this process. The complex interaction between leukocytes and platelets leads to the production of reactive oxygen species (ROI), which in turn causes damage to the endothelial cells due to reduced blood flow, potentially increasing the risk of aortic dissection.14 The persistent inflammatory response results in a substantial augmentation in platelet synthesis. Therefore, an elevated platelet count serves as an indicator of the present state and magnitude of inflammation. In summary, relying solely on the presence of inflammation or coagulation signs is insufficient for appropriately evaluating the advancement of ATAAD. In contrast, the combination of biochemical signals between inflammation and coagulation markers may be able to better reflect the complete pathophysiological process of ATAAD.
PIV is a recently established indicator that measures inflammation and coagulation-related factors, including the levels of neutrophils, lymphocytes, monocytes, and platelets. PIV, in contrast to prior indices such as PLR, includes a greater number of regularly evaluated blood cell types that can indicate systemic inflammatory and immunological conditions.12,35,36 Therefore, it provides a more comprehensive representation of the host’s condition and possesses a more dependable predictive significance for ATAAD. PIV serves as an early prognostic indication for various diseases, including metastatic colorectal cancer, breast cancer, prostate cancer, and ST-segment elevation myocardial infarction.18,19,21,37 The PIV was markedly elevated in the bad clinical result group compared to the excellent prognosis group in these disorders, indicating a strong correlation between high PIV and unfavorable clinical outcomes. This additionally presents compelling evidence for our investigation into the correlation between PIV and ATAAD.
Our investigation revealed that elevated PIV levels (>1807.704) were a reliable indicator of in-hospital mortality following surgery in patients with ATAAD. This association remained statistically significant even after accounting for factors such as hypertension, albumin levels, and urea levels (P < 0.05). The findings align with the research conducted by Giovanni, Lee et al.19,38 Furthermore, the researchers discovered that individuals with elevated PIV levels experienced notably reduced survival durations and increased mortality rates, maybe due to the makeup of PIV.19,38 The SII, comprising neutrophils, platelets, and lymphocytes, closely resembles PIV. However, it is worth noting that monocytes are not included in the compositional index of SII. Monocytes are widely recognized as one of the most significant subpopulations of leukocytes. In their study, Pamukcu et al39 discovered a strong correlation between monocytes and the onset of acute coronary syndrome. They also observed that a high monocyte count upon admission was strongly linked to a negative outcome in acute coronary syndrome. Li et al29 discovered that the introduction of monocytes into the ATAAD mice model led to a rise in aortic dissection. Shota et al40 discovered that by inhibiting the concentration of monocytes and their ability to migrate through endothelial cells, they were able to greatly decrease the occurrence of ATAAD in an animal model that involved the infusion of β-aminopropionitrile and angiotensin II. Therefore, the control of monocyte phenotype has become a distinct therapeutic focus for preventing and treating cardiovascular diseases.19 Thus, PIV demonstrates a higher level of consistency and reliability in predicting unfavorable prognosis compared to measures that have been previously examined. PIV on admission is a clinically relevant determinant in the development of ATAAD and serves as an early prognostic indicator for postoperative in-hospital mortality in patients with ATAAD. Implementing proactive management of inflammation and coagulation upon admission could potentially enhance the in-hospital survival of patients with ATAAD in the future. Another discovery from this study is that we examined the disparities in hospitalization outcomes among groups with varying levels of PIV. We observed a notably greater occurrence of postoperative renal insufficiency in patients with high PIV levels compared to those with low PIV levels. Extracorporeal circulation frequently causes a reduction in blood flow during surgery and low blood pressure, which increases the likelihood of inadequate blood supply to the kidneys during the operation. Upon the termination of extracorporeal circulation, the kidneys receive sufficient blood flow again. However, this restoration of blood flow leads to ischemia-reperfusion injury (IRI), which triggers the production of reactive oxygen species. These reactive oxygen species then encourage the release of many types of inflammatory proteins, including proinflammatory transcription factors.41,42 Furthermore, cytokines and chemokines will stimulate the activation and recruitment of inflammatory cells, including neutrophils, lymphocytes, and macrophages, to the renal parenchyma. This process causes inflammation in the kidney, ultimately resulting in acute kidney injury.43,44 This demonstrates the presence of clinical deleterious effects of high PIV on acute kidney injury.
The four blood cells in PIV are obtained from standard blood samples that are frequently evaluated in clinical settings. These samples are easily obtained and analyzed, without incurring any additional costs for the patient or the healthcare system. This economic advantage would be particularly significant if implemented in impoverished regions. PIV, a novel biomarker parameter, surpasses prior inflammatory indicators in its comprehensiveness and can aid in the early prognosis prediction of ATAAD hospitalized patients following surgery. Identifying indicators that indicate changes in the inflammatory and coagulation status of patients might be crucial in optimizing their therapy in clinical practice. These indicators serve as an important addition to prognostic indicators.
Limitations
There are several limitations to this study. Given the small number of participants and the fact that this study looked back at past data, it is possible that biases and confounding factors could have influenced the results. For example, differences in the treatment methods used after surgery among patients could affect the outcomes. Thus, it is imperative to improve oversight of confounding variables to bolster the dependability of the results. Moreover, the precise mechanisms that elucidate the relationship between increased levels of PIV and more unfavorable clinical results are still unidentified. Engaging in future prospective studies may provide further insight into this matter. Future research should prioritize the development and enhancement of prediction models that incorporate admission of PIV in patients with ATAAD. Moreover, carrying out multi-center research will serve to validate the feasibility of implementing these models in a clinical environment.
Conclusion
This study establishes that elevated levels of PIV pose a distinct risk for mortality within the hospital setting among patients who have ATAAD surgery. Biochemical tests provide the benefits of being fast, uncomplicated, and cost-effective, and show potential for use in clinical settings. We are certain that PIV holds significant promise as a straightforward and expeditious indicator of postoperative in-hospital mortality in patients having ATAAD.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Institutional Review Board Statement
Ethical approval for this study was obtained from the Ethics Committee of Fujian Medical University Union Hospital (No. 2020KY082).
Informed Consent Statement
Written informed consent was obtained from the patients for their anonymized information to be published in this article.
Acknowledgments
The authors thank all participants who were involved with this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The research was funded by the Fujian Provincial Finance Special Project (Grant number: 2023CZ005), the Fifth Batch of Hospital Key Discipline Construction Projects (Grant number: 2022YYZDXK01), Fujian Province Center for Cardiovascular Medicine Construction Project (Grant number: NO.2021-76) and Key Laboratory of Cardio-Thoracic Surgery (Fujian Medical University), Fujian Province University.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Chiappini B, Schepens M, Tan E, et al. Early and late outcomes of acute type A aortic dissection: analysis of risk factors in 487 consecutive patients. Eur Heart J. 2005;26(2):180–186. doi:10.1093/eurheartj/ehi024
2. Czerny M, Schmidli J, Adler S, et al. Current options and recommendations for the treatment of thoracic aortic pathologies involving the aortic arch: an expert consensus document of the European Association for Cardio-Thoracic surgery (EACTS) and the European Society for Vascular Surgery (ESVS). Eur J Cardiothorac Surg. 2019;55(1):133–162. doi:10.1093/ejcts/ezy313
3. Zhu Y, Lingala B, Baiocchi M, et al. Type A aortic dissection—experience over 5 decades. J Am Coll Cardiol. 2020;76(14):1703–1713. doi:10.1016/j.jacc.2020.07.061
4. Evangelista A, Isselbacher EM, Bossone E, et al. Insights from the international registry of acute aortic dissection: a 20-year experience of collaborative clinical research. Circulation. 2018;137(17):1846–1860. doi:10.1161/CIRCULATIONAHA.117.031264
5. Apaydin AZ, Buket S, Posacioglu H, et al. Perioperative risk factors for mortality in patients with acute type a aortic dissection. Ann Thorac Surg. 2002;74(6):2034–2039. doi:10.1016/S0003-4975(02)04096-1
6. Vento V, Multon S, Ramadan R, et al. Outcomes of urgent aortic wrapping for acute type A aortic dissection. J Thorac Cardiovasc Surg. 2022;164(5):1412–1420. doi:10.1016/j.jtcvs.2020.10.136
7. Di Marco L, Leone A, Murana G, et al. Acute type A aortic dissection: rationale and outcomes of extensive repair of the arch and distal aorta. Int J Cardiol. 2018;267:145–149. doi:10.1016/j.ijcard.2018.05.111
8. Shimomura R, Nezu T, Hosomi N, et al. Alpha-2-macroglobulin as a promising biological marker of endothelial function. J Atheroscler Thromb. 2018;25(4):350–358. doi:10.5551/jat.41335
9. Lu J, Li P, Ma K, et al. OPG/TRAIL ratio as a predictive biomarker of mortality in patients with type A acute aortic dissection. Nat Commun. 2021;12(1):3401. doi:10.1038/s41467-021-23787-5
10. Liu H, Li H, Han L, et al. Inflammatory risk stratification individualizes anti-inflammatory pharmacotherapy for acute type A aortic dissection. Innovation. 2023;4(4):100448. doi:10.1016/j.xinn.2023.100448
11. Pinard A, Jones GT, Milewicz DM. Genetics of thoracic and abdominal aortic diseases: aneurysms, dissections, and ruptures. Circ Res. 2019;124(4):588–606. doi:10.1161/CIRCRESAHA.118.312436
12. Chen Y, Dong K, Fang C, et al. The predictive values of monocyte–lymphocyte ratio in postoperative acute kidney injury and prognosis of patients with Stanford type A aortic dissection. Front Immunol. 2023;14:1195421. doi:10.3389/fimmu.2023.1195421
13. Gao H, Sun X, Liu Y, et al. Analysis of hub genes and the mechanism of immune infiltration in Stanford type A aortic dissection. Front Cardiovasc Med. 2021;8:680065. doi:10.3389/fcvm.2021.680065
14. Totani L, Evangelista V. Platelet–Leukocyte interactions in cardiovascular disease and beyond. Arterioscler Thromb Vasc Biol. 2010;30(12):2357–2361. doi:10.1161/ATVBAHA.110.207480
15. Zhang B, Zeng K, Guan RC, et al. Single-cell RNA-seq analysis reveals macrophages are involved in the pathogenesis of human sporadic acute type a aortic dissection. Biomolecules. 2023;13(2):399. doi:10.3390/biom13020399
16. Ma X, Jia C, Fu D, et al. Analysis of hematological traits in polled yak by genome-wide association studies using individual SNPs and haplotypes. Genes. 2019;10(6):463. doi:10.3390/genes10060463
17. Lin F, Zhang LP, Xie SY, et al. Pan-immune-inflammation value: a new prognostic index in operative breast cancer. Front Oncol. 2022;12:830138. doi:10.3389/fonc.2022.830138
18. Qi X, Qiao B, Song T, et al. Clinical utility of the pan-immune-inflammation value in breast cancer patients. Front Oncol. 2023;13:1223786. doi:10.3389/fonc.2023.1223786
19. Fucà G, Guarini V, Antoniotti C, et al. The pan-immune-inflammation value is a new prognostic biomarker in metastatic colorectal cancer: results from a pooled-analysis of the valentino and TRIBE first-line trials. Br J Cancer. 2020;123(3):403–409. doi:10.1038/s41416-020-0894-7
20. Kazan DE, Kazan S. Systemic immune inflammation index and pan-immune inflammation value as prognostic markers in patients with idiopathic low and moderate risk membranous nephropathy. Eur Rev Med Pharmacol Sci. 2023;27(2):642–648. doi:10.26355/eurrev_202301_31065
21. Zhu M, Zhou Y, Liu Z, et al. Diagnostic efficiency of pan-immune-inflammation value to predict prostate cancer in patients with prostate-specific antigen between 4 and 20 ng/mL. J Clin Med. 2023;12(3):820. doi:10.3390/jcm12030820
22. Kato A, Ito E, Kamegai N, et al. Risk factors for acute kidney injury after initial acute aortic dissection and their effect on long-term mortality. Ren Replace Ther. 2016;2(1):53. doi:10.1186/s41100-016-0061-z
23. Morisaki A, Hosono M, Sasaki Y, et al. Risk factor analysis in patients with liver cirrhosis undergoing cardiovascular operations. Ann Thorac Surg. 2010;89(3):811–817. doi:10.1016/j.athoracsur.2009.12.021
24. Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101(6):1644–1655. doi:10.1378/chest.101.6.1644
25. Muckart DJJ, Bhagwanjee S. American college of chest physicians/society of critical care medicine consensus conference definitions of the systemic inflammatory response syndrome and allied disorders in relation to critically injured patients. Crit Care Med. 1997;25(11):1789–1795. doi:10.1097/00003246-199711000-00014
26. Pagni S, Ganzel BL, Trivedi JR, et al. Early and midterm outcomes following surgery for acute type a aortic dissection. J Card Surg. 2013;28(5):543–549. doi:10.1111/jocs.12170
27. Pape LA, Awais M, Woznicki EM, et al. Presentation, diagnosis, and outcomes of acute aortic dissection. J Am Coll Cardiol. 2015;66(4):350–358. doi:10.1016/j.jacc.2015.05.029
28. Ke C, Wu H, Xi M, Shi W, Huang Q, Lu G. Clinical features and risk factors of postoperative in-hospital mortality following surgical repair of Stanford type A acute aortic dissection. BMC Cardiovasc Disord. 2021;21(1):392. doi:10.1186/s12872-021-02107-1
29. Li DZ, Chen QJ, Sun HP, et al. Mean platelet volume to platelet count ratio predicts in-hospital complications and long-term mortality in type A acute aortic dissection. Blood Coagul Fibrinolysis. 2016;27(6):653–659. doi:10.1097/MBC.0000000000000449
30. Nagareddy P, Smyth SS. Inflammation and thrombosis in cardiovascular disease. Curr Opin Hematol. 2013;20(5):457–463. doi:10.1097/MOH.0b013e328364219d
31. Ibrahim H, Schutt RC, Hannawi B, DeLao T, Barker CM, Kleiman NS. Association of immature platelets with adverse cardiovascular outcomes. J Am Coll Cardiol. 2014;64(20):2122–2129. doi:10.1016/j.jacc.2014.06.1210
32. Angiolillo DJ, Bernardo E, Sabaté M, et al. Impact of platelet reactivity on cardiovascular outcomes in patients with type 2 diabetes mellitus and coronary artery disease. J Am Coll Cardiol. 2007;50(16):1541–1547. doi:10.1016/j.jacc.2007.05.049
33. Luo MH, Luo JC, Zhang YJ, et al. Early postoperative organ dysfunction is highly associated with the mortality risk of patients with type A aortic dissection. Interact Cardiovasc Thorac Surg. 2022;35(6):ivac266. doi:10.1093/icvts/ivac266
34. Del Porto F, Proietta M, Tritapepe L, et al. Inflammation and immune response in acute aortic dissection. Ann Med. 2010;42(8):622–629. doi:10.3109/07853890.2010.518156
35. Lin Y, Peng Y, Chen Y, et al. Association of lymphocyte to monocyte ratio and risk of in-hospital mortality in patients with acute type A aortic dissection. Biomarker Med. 2019;13(15):1263–1272. doi:10.2217/bmm-2018-0423
36. Du X, Zhang S, Xu J, et al. Diagnostic value of monocyte to high-density lipoprotein ratio in acute aortic dissection in a Chinese han population. Expert Rev Mol Diagn. 2020;20(12):1243–1252. doi:10.1080/14737159.2020.1847647
37. Murat B, Murat S, Ozgeyik M, Bilgin M. Comparison of pan‐immune‐inflammation value with other inflammation markers of long‐term survival after ST‐segment elevation myocardial infarction. Eur J Clin Invest. 2023;53(1):e13872. doi:10.1111/eci.13872
38. Lee LE, Ahn SS, Pyo JY, Song JJ, Park YB, Lee SW. Pan-immune-inflammation value at diagnosis independently predicts all-cause mortality in patients with antineutrophil cytoplasmic antibody-associated vasculitis. Clin Exp Rheumatol. 2021;39(2):88–93. doi:10.55563/clinexprheumatol/m46d0v
39. Pamukcu B, Lip GYH, Devitt A, Griffiths H, Shantsila E. The role of monocytes in atherosclerotic coronary artery disease. Ann Med. 2010;42(6):394–403. doi:10.3109/07853890.2010.497767
40. Tomida S, Aizawa K, Nishida N, et al. Indomethacin reduces rates of aortic dissection and rupture of the abdominal aorta by inhibiting monocyte/macrophage accumulation in a murine model. Sci Rep. 2019;9(1):10751. doi:10.1038/s41598-019-46673-z
41. Crompton M. The mitochondrial permeability transition pore and its role in cell death. Biochem Soc. 1999;341(Pt 2):233–249. doi:10.1042/bj3410233
42. Bishopric N. Molecular mechanisms of apoptosis in the cardiac myocyte. Curr Opin Pharmacol. 2001;1(2):141–150. doi:10.1016/S1471-4892(01)00032-7
43. Wei C, Li L, Kim IK, Sun P, Gupta S. NF-κB mediated miR-21 regulation in cardiomyocytes apoptosis under oxidative stress. Free Radic Res. 2014;48(3):282–291. doi:10.3109/10715762.2013.865839
44. Stoner JD, Clanton TL, Aune SE, Angelos MG. O2 delivery and redox state are determinants of compartment-specific reactive O2 species in myocardial reperfusion. Am J Physiol-Heart Circ Physiol. 2007;292(1):H109–H116. doi:10.1152/ajpheart.00925.2006
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

