Back to Journals » Clinical Ophthalmology » Volume 19
The Prevalence of Corneal Sensitivity Loss in Patients with and without Dry Eye Disease
Authors Stolz M
Received 18 December 2024
Accepted for publication 14 April 2025
Published 18 April 2025 Volume 2025:19 Pages 1323—1330
DOI https://doi.org/10.2147/OPTH.S513005
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
Matthew Stolz
Clemson Eye, Greenville, SC, USA
Correspondence: Matthew Stolz, Clemson Eye, 360 Pelham Road, Greenville, SC, 29615, USA, Tel +1-864-268-1000, Email [email protected]
Purpose: To assess the prevalence of corneal sensitivity loss in consecutive patients presenting to the clinic as well as in those patients with and without dry eye disease (DED).
Methods: Retrospective, single-center study of consecutive patients who presented to the eye clinic and underwent corneal sensitivity testing using a non-contact esthesiometer. Data included demographics, medical history, prior or current treatments, comorbidities, corneal sensitivity measurements, dry eye symptoms (Standard Patient Evaluation of Eye Dryness Questionnaire [SPEED] questionnaire), and corneal staining scores (Oxford scale). The primary outcome was the prevalence of corneal sensitivity loss, defined as ≥ 8 mbar. Secondary outcome measures included the prevalence of corneal sensitivity loss in eyes with DED (Oxford ≥ 2 and SPEED ≥ 5) and without DED (Oxford ≤ 1 and SPEED < 5).
Results: A total of 395 eyes of 198 patients were included for analysis. Average age was 67.7 ± 16.0 years, and the majority of patients (60.6%) were female. Corneal sensitivity loss was observed in 9.4% of all eyes, and 12.6% of patients had reduced corneal sensitivity in at least one eye. When assessing eyes with signs of DED (Oxford ≥ 2), 19.7% (13/66) had corneal sensitivity loss. This prevalence increased to 31.4% (11/35) in eyes with both signs and symptoms of DED. Conversely, the prevalence was 5.5% (12/219) in eyes without DED. Binary logistic regression demonstrated that Oxford staining score was the strongest predictor of reduced corneal sensitivity (OR: 2.0, 95% CI: 1.3– 3.0, p=0.001), with other significant factors including history of DED, stroke, and herpes zoster virus.
Conclusion: Reduced corneal sensation, a sign of corneal nerve damage and precursor to neurotrophic keratitis, affects nearly 10% of all eyes and 30% of eyes with signs and symptoms of DED. Routine clinical testing of corneal sensation should be implemented, particularly in patients with DED, to ensure early diagnosis and prompt treatment to prevent disease progression.
Keywords: corneal nerves, corneal sensation, corneal sensitivity, dry eye, esthesiometer, neurotrophic keratitis
Introduction
The cornea has the highest sensory and autonomic nerve fiber concentration within the body.1,2 These nerve fibers and nociceptors pick up various signals ranging from mechanical pressure, temperature changes, and chemical stimuli (eg inflammation) that induce blinking and tearing.3 In addition, these nerves release neurotrophic factors that support the ocular surface epithelium and influence goblet cell production of mucin.1 On the contrary, the corneal epithelium expresses nerve growth factor and glial cell-derived neurotrophic factor, which have been shown to play an important role in promoting corneal nerve regeneration following injury.4 Thus, corneal nerves and epithelial cells mutually support each other, and damage to one may compromise the function in the other.5 Epitheliopathy, or damage to the corneal epithelium, is a common clinical feature of dry eye disease (DED) and is attributed to an unstable tear film. This disruption of the corneal epithelial barrier can expose corneal sensory receptors and make the corneal nerves more vulnerable to injury. Alternatively, reduced corneal nerve health may result in poor wound healing and breakdown of the corneal epithelium. This is supported by studies that have shown mice with higher corneal nerve density exhibit faster corneal epithelial wound healing.6,7 Over time, prolonged deterioration of the ocular surface due to underlying inflammation can result in reduced corneal sensitivity and dysfunction of corneal innervation, ultimately resulting in neurotrophic keratitis (NK).
NK is believed to be a rare, orphan indication, affecting 0.8–11 cases per 10,000 or less than 200,000 patients in the USA.8 Nevertheless, the literature suggests that the prevalence of reduced corneal sensation (ie neurotrophic state) may be higher than initially believed. This is supported by a number of studies that have shown that patients with DED, which affects 5–35% of individuals, have significantly reduced corneal nerve density compared to healthy eyes.9,10 In fact, as the severity of DED worsens, corneal nerve density also decreases.11,12 Moreover, studies have shown that patients with DED exhibit reduced corneal sensitivity,12–14 which is directly correlated with the severity of epithelial keratopathy as measured by corneal staining.13
Given the high prevalence of DED, the neurotrophic state may be more prevalent than initially believed. While the best opportunity to reverse ocular surface damage and prevent progression of NK is early in the disease course, diagnosis of NK may be delayed as patients may experience only mild signs or symptoms of DED, and corneal sensitivity testing is not widely utilized in routine clinical practice. Thus, we sought to evaluate the prevalence of corneal sensitivity loss in patients presenting to the clinic and assess associated risk factors.
Materials and Methods
A retrospective, single-center chart review was conducted on consecutive patients who presented to the eye clinic and underwent corneal sensitivity testing using a non-contact esthesiometer between January 2024 and December 2024 by a single physician. Corneal sensitivity testing was part of routine clinical work-up and was conducted on all patients presenting to the clinic, regardless of chief complaint or reason for visit. The study was conducted in accordance with the tenets of the Declaration of Helsinki and was exempt under 45 CFR §46.101(b)(4) by Sterling IRB (#12768). As such, the requirement of obtaining patient informed consent to review medical records was waived by the IRB. Patients were included if they were at least 18 years of age and had corneal sensitivity measurements with a non-contact esthesiometer (Brill Engines, Barcelona, Spain). Data retrieved from patients’ medical records included demographics, medical history, ocular comorbidities, prior and concomitant ocular medications, SPEED scores, corneal staining scores, and corneal sensitivity measurements. Primary outcome was the prevalence of corneal sensitivity loss, which was defined as a patient sensation of 8 mbar (level 4) or higher. Secondary outcomes included the prevalence of corneal sensitivity loss in eyes with and without DED as well as risk factors associated with reduced corneal sensitivity. DED was defined as eyes that had both signs and symptoms of DED (Oxford grade ≥2 and SPEED score ≥5). Eyes without DED were defined as those with minimal or no staining (Oxford grade ≤1) in patients who had no symptoms of DED (SPEED <5).
Esthesiometry
Corneal sensitivity was performed as previously described15,16 using a non-contact esthesiometer (Brill Engines, Spain) prior to any anesthetics being applied into the patient’s eye. The device, which was mounted on a slit lamp, emits two LED lights that converge on the subject’s cornea when positioned 4 mm from the corneal surface, which ensures both accurate positioning on the cornea as well as correct distancing for precise measurements. The esthesiometer produces pulses of air at five different intensities, which range in pressure from 2 mbar to 10 mbar. Each pressure range is defined as the average estimated pressure over a 0.4 mm diameter surface. Corneal sensitivity was measured by administering air puffs to the central cornea, starting at the lowest pressure (level 1 or ~2 mbar) and increasing the level/pressure until the patient verbally reported sensing the air puff. The lowest level that the patient could sense the air puff was recorded. The aforementioned steps were repeated for the contralateral eye, producing two corneal sensitivity readings for each patient. Reduced corneal sensation was defined as level 4 (~8 mbar) or higher.17
SPEED Questionnaire
Patients’ subjective dry eye symptoms were assessed using the Standard Patient Evaluation of Eye Dryness (SPEED) questionnaire, which is a validated survey that evaluates both the frequency and severity of dry eye symptoms in eight questions. The patient grades the frequency of symptoms on a scale of 0–3, with 0 being ‘never’ and 3 being “constant”. The severity of symptoms is rated on a scale of 0–4, with 0 being “no problems” and 4 being “intolerable”. The numeric value for each answer is added to give a total score ranging from 0 to 28, with a score ≥ 5 indicative of mild dry eye, ≥ 7 indicating moderate dry eye, and a score ≥ 10 indicating severe dry eye.18
Corneal Staining
Fluorescein sodium ophthalmic strips without topical anesthetics (BioGlo; Hub Pharmaceuticals, Scottsdale, AZ) were used to evaluate ocular surface damage, which was graded using the Oxford grading scale.19 The Oxford scale grades corneal staining according to severity as determined by the number and density of punctate dots: 0 = absent, I = minimal, II = mild, III = moderate, IV = marked, and V = severe. The overall appearance of the patient’s corneal staining was compared with a reference figure and the grade that best represented the state of corneal staining was selected.
Statistical Analyses
All statistical analyses were conducted using IBM SPSS Statistics version 30.0 (IBM; Armonk, NY, USA). The study sample is described using summary statistics (n, mean, standard deviation, median, and maximum/ minimum) for continuous data and frequency statistics (counts and percentages) for categorical data. Continuous outcome measures were compared between groups (reduced corneal sensitivity versus normal corneal sensitivity) using the Independent Samples T-test, whereas percentages and frequencies were assessed using Chi-Squared test or Fisher’s Exact Test when one or more cells had an expected cell count less than 5. Binary logistic regression using backwards technique was conducted to determine factors significantly associated with corneal sensitivity loss. Pearson correlation coefficient was used to assess correlations between linear variables. Hypothesis testing was performed at the 5% significance level, and all confidence intervals are two-sided with 95% coverage.
Results
A total of 395 eyes of 198 patients were included for analysis. Average age was 67.7 ± 16.0 years, and the majority of patients (60.6%) were female. Furthermore, 80.3% of patients were Caucasian or White, 18.7% were African American or Black, and 1% were Asian. Medical history and common comorbidities included hypertension (79.3%), cataract (71.2%), diabetes mellitus (31.3%), DED (66.2%), glaucoma (16.2%), herpes zoster virus (3.0%), Parkinson’s disease (2.5%), stroke (10.1%), and ocular infection (4.0%). More than half (55.1%) of patients had undergone prior ocular surgery, with 53.0% of patients having a history of cataract surgery. Current ocular medications included cyclosporine (12.1%), steroids (5.1%), artificial tears (63.1%), and glaucoma drops (13.6%). Average corneal staining score was 0.73 ± 0.82 (median:1, range: 0–3), which was graded as absent in 47.3% of eyes, minimal in 35.9%, mild in 13.2%, and moderate in 3.5% of eyes. Corneal staining scores (OD and OS) were strongly correlated between eyes (r=0.93, p<0.001). Average SPEED score was 4.29 ± 4.91 (median: 3, range: 0–25); the majority of patients (63.1%) were asymptomatic, 12.6% had mild symptoms of DED, 11.6% had moderate symptoms of DED, and 12.6% of patients had severe symptoms of DED.
When assessing the lowest pressure level at which eyes could detect corneal sensation (Figure 1), 38.2% of eyes detected level 1 (2.6 ± 0.2 mbar), 44.6% detected level 2 (4.6 ± 0.2 mbar), 7.8% detected level 3 (6.6 ± 0.3 mbar), 6.3% detected level 4 (8.5 ± 0.2 mbar), and 3.0% detected level 5 (10.3 ± 0.3 mbar). Corneal sensitivity measurements of both eyes (OS and OD) were strongly correlated (r=0.77, p<0.001). A total of 25 patients (12.6%; 95% CI: 8.6–18%) had at least one eye with reduced corneal sensitivity, which was defined as level 4 or higher (≥ 8 mbar), and 9.4% (95% CI: 6.8–12.7%) of all eyes had reduced corneal sensitivity (Figure 1).
 |
Figure 1 Lowest pressure level at which eyes could detect corneal sensitivity using a non-contact esthesiometer. Level 4 or higher is indicative of corneal sensitivity loss. |
When assessing the prevalence of reduced corneal sensitivity by corneal staining grade (Figure 2), 2.1% (4/187) of eyes with Oxford grade 0 or no staining had reduced corneal sensitivity, 14.1% (20/142) of eyes with Oxford grade 1 or minimal staining had reduced sensitivity, 19.2% (10/52) of eyes with Oxford grade 2 or mild staining had reduced sensitivity, and 21.4% (3/14) of eyes with Oxford grade 3 or moderate staining had reduced sensitivity (p<0.001). Similarly, when assessing the prevalence of reduced corneal sensitivity by severity of DED symptoms by SPEED score (Figure 3), reduced corneal sensitivity was present in 5.6% (14/250) of asymptomatic eyes, 8.0% (4/50) of eyes with mild symptoms, 19.5% (9/46) of eyes with moderate symptoms, and 20.4% (10/49) of eyes with severe symptoms (p<0.001). When assessing the prevalence of corneal sensitivity loss in patients with both signs (Oxford grade ≥ 2) and symptoms (SPEED score ≥5) of DED, the rate was 31.4% (11/35). The prevalence of corneal sensitivity loss in patients with no signs or symptoms of DED (Oxford grade ≤1 and SPEED score<5) of DED was 5.5% (12/219).
 |
Figure 2 Percentage of eyes with corneal sensitivity loss (level 4 or higher) by severity of punctate staining (Oxford grade). |
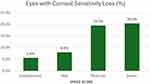 |
Figure 3 Percentage of eyes with corneal sensitivity loss (level 4 or higher) by severity of dry eye symptoms (SPEED Score). |
Eyes with reduced corneal sensitivity had significantly higher SPEED scores (6.8 ± 4.9 vs 4.0 ± 4.8, p=0.005) and corneal staining scores (1.3 ± 0.8 vs 0.7 ± 0.8, p<0.001) compared to eyes with normal corneal sensation (Table 1). In fact, of those eyes with corneal sensitivity loss, 89% had some degree of corneal staining, and 62% had symptoms of DED (SPEED score ≥5). Furthermore, patients who had reduced corneal sensitivity in at least one eye were significantly older and had significantly higher prevalence of comorbidities including DED, stroke, herpes zoster virus, and hypertension (Table 1). Binary logistic regression demonstrated that corneal staining score was the strongest predictor of reduced corneal sensitivity (OR: 2.0, 95% CI: 1.3–3.0, p=0.001), with other significant predictors including prior stroke (OR: 2.6, 95% CI: 1.0–6.4; p=0.042), diagnosis of DED (OR: 10.0, 95% CI: 1.3–76.7; p=0.021), and history of herpes zoster virus (OR: 4.4, 95% CI: 1.2–15.5; p=0.023).
 |
Table 1 Patient Demographics and Characteristics in Eyes with and without Corneal Sensitivity Loss |
Discussion
In this study, we found that 9.3% of all eyes that presented to the clinic had impaired corneal sensitivity. Interestingly, 96% of patients who had reduced corneal sensitivity also had co-existing DED and were using preservative free artificial tears, and eyes with reduced corneal sensitivity loss had significantly worse signs and symptoms of DED. In fact, of those eyes with corneal sensitivity loss, 89% had some degree of corneal staining. DED, which is associated with a reduced tear film and ocular inflammation, has been shown to cause damage to the corneal nerves. Impaired corneal sensitivity and nerve function can dampen the blinking and tearing reflexes, resulting in an abnormal tear film, more ocular exposure, and ultimately a vicious cycle of deterioration of the ocular surface epithelium and progression into stage 1 NK.20 Notably, we found that the risk of corneal sensitivity loss doubled with every increase in corneal staining score based on logistic regression (OR: 2.0, 95% CI: 1.3–3.0). When assessing eyes with mild to moderate superficial punctate keratitis (≥Oxford grade 2), the rate of reduced corneal sensitivity increased to 20% (13/66). Our results are similar to a prospective, multi-center assessment of 409 eyes, which found 26% of eyes with SPK had reduced corneal sensitivity, defined as ≤ 45mm using a Cochet-Bonnet esthesiometer.21 In that study, the rate of impaired corneal sensitivity increased to 86% in eyes with persistent epithelial defects,21 supporting the notion that dysfunction of corneal innervation and sensitivity is associated with increasing damage to the ocular surface epithelium.
While patients with NK, particularly those with advanced stage disease, are often asymptomatic due to the nature of the condition, several studies suggest that patients with less progressive forms of NK (stage 1) suffer from symptoms similar to DED.22–24 This is supported by recent studies, which found that patients with DED had significantly worse symptoms as well as significantly reduced corneal sensitivity compared to healthy controls.16 Similarly, we found that symptoms of DED were significantly worse in eyes with impaired corneal sensitivity, and as severity of symptoms increased, so did the prevalence of corneal sensitivity loss (Figure 3). In fact, corneal sensitivity loss was observed in 31.4% (11/35) of eyes with both signs and symptoms of DED (Oxford score ≥2 and SPEED score ≥5). For this reason, screening of both signs and symptoms of DED may play a crucial role in identifying patients who are at increased risk for reduced corneal sensitivity.
It should be noted that a recently published study found that 58% (18/31) of patients who presented for cataract surgery with DED (Oxford staining ≥ 1 and TBUT ≤ 10 seconds) had stage 1 NK, which was defined as ≤ 40mm using a Cochet-Bonnet esthesiometer.24 In contrast to the present study, Hovanesian found that corneal sensitivity did not correlate with severity of either corneal staining or SPEED scores. Furthermore, the reported prevalence rate of 58% is much higher than what was observed in the present study in eyes with Oxford grade ≥ 1 (16%). Nevertheless, the aforementioned study only assessed 31 eyes, making it difficult to draw generalizable conclusions due to the small sample size.24
Aside from DED and corneal staining severity, other significant risk factors associated with reduced corneal sensation in this study included a history of stroke and herpes zoster virus. NK is a relatively common complication of herpes zoster ophthalmicus.25 Compared to healthy eyes, eyes with herpes zoster ophthalmicus have a significant decrease in total nerve length, number of nerves, and number of nerve branches, which was found to be significantly correlated with corneal sensation.26 Similarly, patients with history of ischemic stroke have been shown to have significantly greater corneal nerve damage, including reduced corneal nerve density and fiber length.27,28 Thus, these risk factors should be screened for, as they are known to incite corneal nerve damage and increase the risk of developing NK.
There are several ways to assess corneal sensitivity, including a cotton wisp, Cochet-bonnet esthesiometer, and non-contact esthesiometer.29 While the former is more readily available and inexpensive, assessments are highly subjective and not quantifiable. Cochet-bonnet esthesiometers have been widely used, particularly in the clinical and research setting, and are considered the gold standard for obtaining quantitative measurements of corneal sensitivity. This device has a nylon monofilament whose length can be adjusted between 5 and 60 mm to exert different pressures that range from 5 to 180 mm/S.29 However, limitations include risk of injury to the corneal epithelium and non-linear delivered forces. The Brill esthesiometer, which was approved by the FDA in 2023, is a portable, non-contact esthesiometer that delivers pulses of ambient air across five levels (1–10 mbar) as a stimulus.29 A recent study demonstrated that the Brill esthesiometer is effective and safe with operator-independent repeatability and has comparable range and good agreement with the Cochet-Bonnet esthesiometer in both healthy and dry eyes.15,30 Advantages include its non-invasive measurements and the linear increase in pressure with increasing level. Nevertheless, because this a newer device, there is no universally accepted definition as to which level constitutes “reduced corneal sensitivity”. A number of studies have shown that sensitivity commonly ranges from 3 ± 1 mbar in healthy eyes, whereas eyes with OSD, including DED, have a range of 6 ± 3 mbar.16,31,32 As a result, we chose level 4 or higher (≥8 mbar) as our cutoff as a safeguard to prevent overinflating results.
While a number of DED treatments exist, the majority of these therapies do not target or treat the underlying corneal nerves. In the present study, 96% of patients who had reduced corneal sensitivity were currently being treated with artificial tears for DED. This is further supported by a study in which escalation of treatment for one year following diagnosis of NK resulted in worsening of visual acuity by an average of one line in patients with stage 1 NK. Most common treatments in this study included autologous serum tears (46%), anti-infective ointments and drops (75%), anti-inflammatory drops (54%), oral anti-virals (44%), bandage contact lens (41%), and punctal occlusion (42%). Thus, treatments that address the corneal nerves should be promptly utilized to prevent worsening of NK and visual function. There are currently few treatments that have been shown to promote regeneration of the corneal nerves and improve corneal sensitivity, which include recombinant human nerve growth factor (Cenegermin) and cryopreserved amniotic membrane (AM). Cenegermin, which is FDA approved for NK, has recently been shown to improve signs, symptoms, and corneal sensitivity in patients with stage 1 NK.23 Nevertheless, the long-term durability of improvement in corneal sensation remains unclear, and its high cost (>$90,000) may prevent widespread and repetitive use. Self-retained cryopreserved AM (Prokera) has been shown to promote corneal nerve regeneration, significantly improve corneal sensitivity, and improve both signs and symptoms in patients with severe DED at 3 months.33 Thus, AM may prove a fruitful treatment option for patients with stage 1 NK, eg those with reduced corneal sensitivity as well as signs and symptoms of DED.
There are several limitations to this study. First, this study was conducted retrospectively. Nevertheless, corneal sensitivity testing was conducted on every patient who entered the clinic as part of routine clinical work-up, regardless of chief complaint or reason for office visit. Furthermore, the other assessments, including the SPEED questionnaire and corneal staining, were conducted on the same day, which helps to ensure that the collected data were accurate. Second, corneal sensitivity testing is a subjective test. Future studies may like to assess how corneal sensitivity measurements using the Brill esthesiometer correlate with corneal nerve density to substantiate these findings through objective measures. Nevertheless, corneal sensitivity testing is the gold standard in diagnosing NK, as in vivo confocal microscopy is timely, expensive, and not widely available to both optometrists and ophthalmologists. Lastly, while the literature widely reports NK being defined as ≤ 40mm using the Cochet-Bonnet esthesiometer,23,24 there is no universally accepted definition as to which level of the Brill esthesiometer constitutes “reduced corneal sensitivity”. As stated above, a level 4 or higher (≥8 mbar) was used in this study as a safeguard based off the literature.16,31,32
In summary, the prevalence of corneal sensitivity loss and ultimately corneal nerve damage is higher than previously thought. Routine clinical testing is imperative, particularly in those patients with higher risk factors, to ensure timely diagnosis and treatment and ultimately preserve vision.
Conclusion
Reduced corneal sensation, a sign of corneal nerve damage and precursor to neurotrophic keratitis, affects nearly 10% of all eyes and 30% of eyes with signs and symptoms of DED. Routine clinical testing of corneal sensation should be implemented, particularly in patients with DED, to ensure early diagnosis and prompt treatment to prevent disease progression.
Funding
There is no funding to report.
Disclosure
Dr Matthew Stolz reports personal fees from Biotissue, outside the submitted work.
References
1. Muller LJ, Marfurt CF, Kruse F. et al. Corneal nerves: structure, contents and function. Exp Eye Res. 2003;76(5):521–542. doi:10.1016/s0014-4835(03)00050-2
2. Shaheen BS, Bakir M, Jain S. Corneal nerves in health and disease. Surv Ophthalmol. 2014;59:263–285. doi:10.1016/j.survophthal.2013.09.002
3. Belmonte C, Aracil A, Acosta MC, et al. Nerves and sensations from the eye surface. Ocul Surf. 2004;2(4):248–253. doi:10.1016/S1542-0124(12)70112-X
4. Di G, Qi X, Zhao X, et al. Corneal Epithelium-Derived Neurotrophic Factors Promote Nerve Regeneration. Invest Ophthalmol Vis Sci. 2017;58(11):4695–4702. doi:10.1167/iovs.16-21372
5. Vereertbrugghen A, Galletti JG. Corneal nerves and their role in dry eye pathophysiology. Exp Eye Res. 2022;222:109191. doi:10.1016/j.exer.2022.109191
6. Pham TL, Kakazu A, He J, et al. Mouse strains and sexual divergence in corneal innervation and nerve regeneration. THE FASEB Journal. 2019;33(3):4598–4609. doi:10.1096/fj.201801957R
7. He J, Pham TL, Kakazu A, et al. Recovery of Corneal Sensitivity and Increase in Nerve Density and Wound Healing in Diabetic Mice After PEDF Plus DHA Treatment. Diabetes. 2017;66(9):2511–2520. doi:10.2337/db17-0249
8. Choi CJ, Liu L, Qian Y, et al. Neurotrophic keratopathy: clinical presentation and outcomes in 354 eyes in a community-based population. Eur J Ophthalmol. 2024;34(4):1085–1094. doi:10.1177/11206721231222949
9. Giannaccare G, Pellegrini M, Sebastiani S, et al. In vivo confocal microscopy morphometric analysis of corneal subbasal nerve plexus in dry eye disease using newly developed fully automated system. Graefes Arch Clin Exp Ophthalmol. 2019;257(3):583–589. doi:10.1007/s00417-018-04225-7
10. Kheirkhah A, Dohlman TH, Amparo F, et al. Effects of corneal nerve density on the response to treatment in dry eye disease. Ophthalmol. 2015;122(4):662–668. doi:10.1016/j.ophtha.2014.11.006
11. Nepp J, Wirth M. Fluctuations of Corneal Sensitivity in Dry Eye Syndromes--A Longitudinal Pilot Study. Cornea. 2015;34(10):1221–1226. doi:10.1097/ICO.0000000000000566
12. Benítez-Del-Castillo JM, Acosta MC, Wassfi MA, et al. Relation between corneal innervation with confocal microscopy and corneal sensitivity with noncontact esthesiometry in patients with dry eye. Invest Ophthalmol Vis Sci. 2007;48(1):173–181. doi:10.1167/iovs.06-0127
13. Bourcier T, Acosta MC, Borderie V, et al. Decreased corneal sensitivity in patients with dry eye. Invest Ophthalmol Vis Sci. 2005;46(7):2341–2345. doi:10.1167/iovs.04-1426
14. Xu K-P, Yagi Y, Tsubota K. Decrease in corneal sensitivity and change in tear function in dry eye. Cornea. 1996;15(3):235–239. doi:10.1097/00003226-199605000-00002
15. Merayo-Lloves J, Gómez Martín C, Lozano-Sanroma J, et al. Assessment and safety of the new esthesiometer BRILL: comparison with the Cochet-Bonnet Esthesiometer. Eur J Ophthalmol. 2024;34(4):1036–1045. doi:10.1177/11206721231210754
16. Villalba M, Sabates V, Orgul S, et al. Detection of Subclinical Neurotrophic Keratopathy by Noncontact Esthesiometry. Ophthalmol Ther. 2024;13(9):2393–2404. doi:10.1007/s40123-024-00998-9
17. Sabater AL, Gonzalez MV. Tools can detect corneal nerve damage early. Ophthalmol Times. 2023;48:1.
18. Asiedu K, Kyei S, Mensah SN, et al. Ocular Surface Disease Index (OSDI) Versus the Standard Patient Evaluation of Eye Dryness (SPEED): a Study of a Nonclinical Sample. Cornea. 2016;35(2):175–180. doi:10.1097/ICO.0000000000000712
19. Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003;22(7):640–650. doi:10.1097/00003226-200310000-00008
20. Mead OG, Tighe S, Tseng SC. Amniotic Membrane Transplantation for Managing Dry Eye and Neurotrophic Keratitis. Taiwan J Ophthalmol. 2020;10:1.
21. Nishida T, Chikama T, Sawa M, et al. Differential contributions of impaired corneal sensitivity and reduced tear secretion to corneal epithelial disorders. Jpn J Ophthalmol. 2012;56(1):20–25. doi:10.1007/s10384-011-0105-4
22. Ruiz-Lozano RE, Hernandez-Camarena JC, Loya-Garcia D, et al. The molecular basis of neurotrophic keratopathy: diagnostic and therapeutic implications. A review. Ocul Surf. 2021;19:224–240. doi:10.1016/j.jtos.2020.09.007
23. Hamrah P, Massaro-Giordano M, Schanzlin D, et al. Phase IV Multicenter, Prospective, Open-Label Clinical Trial of Cenegermin (rhNGF) for Stage 1 Neurotrophic Keratopathy (DEFENDO). Ophthalmol Ther. 2024;13(2):553–570. doi:10.1007/s40123-023-00866-y
24. Hovanesian JA. The THINK Study: testing Hypoesthesia and the Incidence of Neurotrophic Keratopathy in Cataract Patients with Dry Eye. Clin Ophthalmol. 2024;18:3627–3633. doi:10.2147/OPTH.S501452
25. Meyer JJ, Liu K, McGhee CNJ, et al. Neurotrophic Keratopathy After Herpes Zoster Ophthalmicus. Cornea. 2022;41:1433–1436. doi:10.1097/ICO.0000000000003003
26. Hamrah P, Cruzat A, Dastjerdi MH, et al. Unilateral herpes zoster ophthalmicus results in bilateral corneal nerve alteration: an in vivo confocal microscopy study. Ophthalmol. 2013;120(1):40–47. doi:10.1016/j.ophtha.2012.07.036
27. Khan A, Akhtar N, Kamran S, et al. Corneal confocal microscopy detects corneal nerve damage in patients admitted with acute ischemic stroke. Stroke. 2017;48(11):3012–3018. doi:10.1161/STROKEAHA.117.018289
28. Gad H, Khan A, Akhtar N, et al. Corneal nerve and endothelial cell damage in patients with transient ischemic attack and minor ischemic stroke. PLoS One. 2019;14(3):e0213319. doi:10.1371/journal.pone.0213319
29. Crabtree JR, Tannir S, Tran K, et al. Corneal Nerve Assessment by Aesthesiometry: history, Advancements, and Future Directions. Vision. 2024;8(2):34. doi:10.3390/vision8020034
30. Mattes R, Sabatés V, Gomez-Bedoya A, et al. Comparison study between Brill’s non-contact and Cochet-Bonnet esthesiometers to determine corneal sensitivity in dry eye disease patients. Invest Ophthalmol Vis Sci. 2024;65:2938.
31. Vera-Duarte GR, Ramirez-Miranda AJ, Manuel-Garcia A, et al. Corneal Mechanical Sensitivity By Non-Contact Brill Engines Esthesiometer In A Healthy Mexican Population. Invest Ophthalmol Vis Sci. 2024;65:2654.
32. Quiroga Garza ME, Ruiz-Lozano RE, Komai S, et al. Characterization of Sensation in Patients with Accepted Corneal Penetrating Keratoplasty Using a Non-Contact Esthesiometer. Invest Ophthalmol Vis Sci. 2024;65:2649.
33. John T, Tighe S, Sheha H, et al. Corneal Nerve Regeneration after Self-Retained Cryopreserved Amniotic Membrane in Dry Eye Disease. J Ophthalmol. 2017;2017:6404918. doi:10.1155/2017/6404918
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
The THINK Study: Testing Hypoesthesia and the Incidence of Neurotrophic Keratopathy in Cataract Patients with Dry Eye
Hovanesian JA
Clinical Ophthalmology 2024, 18:3627-3633
Published Date: 6 December 2024

