Back to Journals » Clinical Ophthalmology » Volume 19
The Refractive Cataract Surgery Survey (RCSS): A Validated Questionnaire for Quick Clinical Use
Authors Coleman III WT, Martin CR, Davidson CJ , DeNaro BB, Shelby CL, LoBue SA
Received 14 January 2025
Accepted for publication 20 March 2025
Published 2 April 2025 Volume 2025:19 Pages 1191—1202
DOI https://doi.org/10.2147/OPTH.S515694
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Wyche T Coleman III,1 Curtis R Martin,1 Cameron J Davidson,2 Brittany B DeNaro,1 Christopher L Shelby,1 Stephen A LoBue1
1Department of Ophthalmology, Willis-Knighton Medical Center, Shreveport, LA, USA; 2Department of Foundational Medical Studies, Oakland University William Beaumont School of Medicine, Rochester, MI, USA
Correspondence: Stephen A LoBue, Department of Ophthalmology and Director of Research, Willis-Knighton Medical Center, Bert Kouns Industrial Loop, Suite 116, Shreveport, LA, 71118, USA, Tel +1-318-212-5901, Email [email protected]
Purpose: To validate an efficient and reliable instrument for measuring postoperative performance and satisfaction in refractive cataract surgery.
Methods: A 10-question survey was designed to assess patient satisfaction and functional outcomes in refractive cataract surgery. The survey included seven questions rated on a 1– 10 scale and three yes/no questions. Internal consistency was evaluated using Cronbach’s alpha. Correlations between survey responses and objective visual acuity measurements (binocular uncorrected distance visual acuity [BUDVA] and binocular uncorrected near visual acuity [BUNVA]) were analyzed. Factor analysis explored the constructs assessed by the survey.
Results: A total of 477 eyes from 240 patients were included, including 234 AcrySof PanOptix, 53 AcrySof IQ Vivity, 88 TECNIS Eyhance, 102 AcrySof Aspheric Monofocal intraocular lenses (IOLs). Cronbach’s alpha (0.785) indicated acceptable moderate to strong internal consistency. Significant correlations were found between visual acuity and satisfaction ratings for distance (r = 0.256; p < 0.001) and near vision (r = 0.195; p < 0.001). A significant model was found (R² = 0.350, F(7, 474) = 35.86, p < 0.001) with quality of near vision (β = 0.188, p < 0.001), quantity of glasses independence (β = 0.116, p < 0.05), and lens choice (β = 0.434, p < 0.001) being significant predictors for IOL selection.
Conclusion: The Refractive Cataract Surgery Survey (RCSS) is an efficient, reliable tool for assessing patient satisfaction and performance in refractive cataract surgery. The quality of near vision and the level of glasses independence were significant predictors of lens choice satisfaction.
Keywords: refractive cataract surgery, validated survey, presbyopia correcting intraocular lenses, patient satisfaction
Introduction
The accurate assessment of patient satisfaction and visual performance following refractive cataract surgery is essential for the modern-day refractive surgeon. Patient surveys and questionnaires are invaluable in this endeavor.1 Although preoperative surveys, such as the validated National Eye Institute Visual Function Questionnaire (NEI-VQF 25) have been successfully used to assess the health status and visual function of patients with cataracts, more importance is now given to visual performance after cataract surgery.2
Several surveys have been created to measure surgical outcomes and patient performance.3–11 Traditional surveys, such as the Quality of Vision (QoV) questionnaire developed by McAlinden et al, while comprehensive, are often lengthy and designed to address a broad spectrum of ophthalmic conditions, including those associated with various disease processes.6 Surveys such as the Catquest-9SF and the Cataract TyPE surveys are relatively short at 9 and 11 items, respectively, but do not ask questions that specifically address the concerns often associated with presbyopia-correcting intraocular lenses (IOL) including diffractive dysphotopsias.11 For busy clinics focusing on refractive cataract surgery, a shorter, more targeted survey could provide more relevant insights toward overall patient satisfaction and IOL performance.12–14
Thus, we devised a unique refractive cataract surgery survey (RCSS) comprised of 10 concise questions aimed at evaluating key aspects of patient satisfaction and IOL performance. The brevity of the survey is intended to enhance clinic efficiency and survey compliance while analyzing key metrics of IOL performance and patient satisfaction.
To validate our new RCSS, we created a prospective study analyzing various Toric and non-Toric monofocal, enhanced depth of focus (EDOF), and trifocal IOLs to confirm reliability and accuracy among a large number of patients. Refractive accuracy and surgical technique between IOL types were not analyzed in this study but will be the focus of future research.
Methods
Study Design
A prospective clinical study was performed in Shreveport, Louisiana at the Willis-Knighton Eye Institute. Prior to study initiation, the Institutional Review Board (IRB) at Willis-Knighton Medical Center was obtained. The clinical study was conducted according to the tenets of the Declaration of Helsinki. Every patient enrolled was informed about the purpose of the study and provided verbal consent before participating which was approved by the IRB at Willis-Knighton Medical Center.
Patients
All potential patients included in the experiment were adults 18 years of age or older who underwent planned bilateral clear lens exchange or cataract surgery with posterior chamber IOL implantation without complication. The exclusion criteria for all patients included macular pathology (eg, epiretinal membrane or macular edema), glaucoma, corneal disease, or scarring. The exclusion criteria were further defined in patients selected for a trifocal or EDOF IOL involving a high spherical aberration above 0.6.
IOL Description
Monofocal IOLs included in the study involved the TECNIS Eyhance (Johnson and Johnson Vision, New Brunswick, NJ, USA) and AcrySof SA60 IOL (Alcon, Fort Worth, TX, USA) in the Toric and non-Toric type. The EDOF IOL selected was the AcrySof IQ Vivity (Alcon, Fort Worth, TX, USA) in the Toric and non-Toric type. Lastly, the AcrySof IQ PanOptix Trifocal IOL (Alcon, Fort Worth, TX, USA), model TFAT00 vs TFAT30-60 was the primary trifocal lens used in the study.
Procedures and Assessments
Cataract surgery in all patients was assisted with femtosecond laser-assisted cataract surgery (FLACS) technology using the LenSx platform (Alcon, Fort Worth, TX, USA). FLACS was utilized to create a reproducible 5mm anterior capsulotomy and complete fragmentation of the nucleus. The paracentesis and main incision were created manually prior to FLACS. Phacoemulsification was completed with the Centurion system (Alcon, Fort Worth, TX) using topical and intravenous anesthesia. Optiwave refractive analysis (ORA, Alcon Fort Worth, TX) was also used after cataract removal for IOL selection and Toric IOL alignment. A soft polymer irrigation and aspiration tip was used to polish the posterior capsule to mitigate capsule opacification. Overall, cataract extraction was uncomplicated and completed in all patients enrolled in the study.
Visual acuity was obtained using the Snellen chart. The total number of letters read was recorded and converted to logMAR for analyses across all lenses. Distance measurements for binocular and monocular uncorrected distance visual acuity (UDVA) were tested under standardized conditions at 6.1 meters under 100% contrast photopic conditions with adequate room lighting. All binocular and monocular uncorrected near visual acuity (UNVA) was tested between 33 and 40 cm at the patient’s comfortable reading distance with adequate room light with a Rosenbaum near chart.
Patients were examined on postoperative day one, month one, and three months with a final refraction obtained between the first and third months. Manifest refractions were performed using the maximum plus refraction technique in plus cylinder notation.
Questionnaire Design
The RCSS was conducted one month after surgery (Figure 1). The survey was comprised of ten questions. The first seven questions were answered on a 1–10 scale where patients were asked to rate their satisfaction with different aspects of vision and overall lens choice. Additionally, three binary (yes/no) questions assessed post-operative outcomes such as glare and halo perception and their impact on daily activities (Figure 1). Responses to the RCSS questions Q1 to Q7 were analyzed across all four IOLs in our study for the mean, standard deviation, minimum, maximum, and 95% confidence level.
Endpoint
The primary endpoint involves validating the reliability and accuracy of the RCSS through internal consistency. The study employed descriptive statistics to evaluate the spread and normality of individual items on the RCSS. To assess the internal consistency of the survey, Cronbach’s alpha was calculated to validate the reliability of the survey. An analysis was also conducted to determine whether removing any items would enhance internal consistency.
The secondary endpoints involved examining the relationship between objective visual acuity measurements (eg, binocular uncorrected near visual acuity [BUNVA] and binocular uncorrected distance visual acuity [BUDVA]) and specific survey questions to determine outcomes that improve overall patient satisfaction and performance. This was done to provide face and criterion validity via regression analysis using the predicted value for each participant calculated from the survey with the objective values found by postoperative ocular examination.
Statistical Analysis
Statistical comparisons were calculated using SPSS analysis version 30 (IBM, Armonk, New York, USA). Data groups are presented as mean ± standard deviation when applicable. Independent t-tests were used for numeric variables. Chi-square tests were utilized for categorical variables. In all cases, statistical significance was set at p < 0.05.
Results
The validation process included a sample of 477 eyes from 240 patients, comprising 137 females and 103 males. The average patient age was 66.2, ranging from 31 to 83 years old. Four types of intraocular lenses (IOLs) were included in the study, with both Toric and non-Toric options (Table 1). A total of 477 intraocular lenses (IOLs) were included in the study, divided into 225 non-Toric and 242 Toric lenses. The Alcon AcrySof® PanOptix® Trifocal IOL was the most commonly used IOL, accounting for 234 implants, of which 128 were non-Toric (TFAT00) and 106 were Toric (TFAT30-60). The Alcon AcrySof® IQ Vivity™ Enhanced Depth of Focus (EDOF) IOL was used in 53 cases, with 24 non-Toric (DAT015) and 29 Toric (DAT315, DAT415). The Johnson & Johnson TECNIS Eyhance™ EDOF IOL was used in 88 cases, comprising 37 non-Toric (DIB00) and 51 Toric (DIU150-375). Lastly, the Alcon AcrySof® Aspheric Monofocal IOL was implanted in 102 cases, with 36 non-Toric (SA60WF) and 66 Toric (SA6AT3-7).
 |
Table 1 Breakdown of IOLs |
Binocular Uncorrected Distance Visual Acuity (BUDVA)
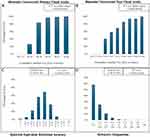
Combined across all IOLs, the 1-month postoperative data shows that 84% of eyes achieved 20/20 or better, with 99% achieving 20/32 or better BUDVA (Figure 2A). For the PanOptix IOL, 89% of eyes achieved 20/20 or better, with 99% achieving 20/32 or better at 1 month postoperatively. With the Eyhance IOL, 81% of eyes achieved 20/20 or better, with 100% achieving 20/32 or better. The Vivity IOL had 63% of eyes achieving 20/20 or better, with 96% achieving 20/32 or better. For the SA60 IOL, 88% of eyes achieved 20/20 or better, with 100% achieving 20/25 or better at 1 month.
Binocular Uncorrected Near Visual Acuity (BUNVA)
Jaeger values were converted to Snellen for consistency and readability. Combined across all IOLs, 41% of eyes achieved 20/20 or better, and 86% achieved 20/40 or better at 1 month postoperatively (Figure 2B). For the PanOptix IOL, 81% of eyes achieved 20/20 or better, and 99% achieved 20/40 or better. With the Eyhance IOL, 4% of eyes achieved 20/20 or better, and 81% achieved 20/40 or better. The Vivity IOL had 41% of eyes achieving 20/20 or better, and 96% achieving 20/40 or better at 2 months postoperatively. For the SA60 IOL, 10% of eyes achieved 20/20 or better, and 64% achieved 20/40 or better.
Spherical Equivalent Refraction Accuracy
Across all IOLs, 82% of eyes achieved a postoperative spherical equivalent refraction (SEQ) within ±0.50 D of target, with 96% within ±1.00 D (Figure 2C). PanOptix IOL patients achieved 90% within ±0.50 D and 100% within ±1.00 D. Eyhance IOL patients reached 80% within ±0.50 D and 98% within ±1.00 D. Vivity IOL patients had 68% within ±0.50 D and 84% within ±1.00 D. SA60 IOL patients achieved 74% within ±0.50 D and 95% within ±1.00 D at 1 month postoperatively.
Refractive Astigmatism
Combined refractive astigmatism results showed 85% of eyes achieving ≤0.50 D of refractive astigmatism, and 98% of eyes achieving ≤1.00 D (Figure 2D). PanOptix IOL results showed 82% of eyes were ≤0.50 D, with 99% within ≤1.00 D. Eyhance IOL achieved 86% within ≤0.50 D and 98% within ≤1.00 D. Vivity IOL showed 84% within ≤0.50 D and 98% within ≤1.00 D. SA60 IOL had 85% of eyes within ≤0.50 D and 97% within ≤1.00 D at 1 month postoperatively.
Survey Results
Overall, the PanOptix and Vivity demonstrated higher satisfaction ratings for questions 1–7 with mean scores at 9.38 ± 1.23 and 9.06 ± 1.63 respectively. The SA60 and Eyhance had lower overall mean scores for questions 1–7 at 8.74 ± 1.38 and 8.27 ± 2.01 respectively (Figure 3A). Questions 8–10 involved yes/no questions regarding additional aspects of patient satisfaction, including lens choice and visual disturbances such as glare and halo. Patients desiring to select the same lens again (question 8) were highest in the PanOptix IOL at 95%. The presence of glare (question 9) which limited activities (question 10) was also highest in the PanOptix group at 43% and 10% respectively (Figure 3B).
 |
Figure 3 RCSS Survey Results: The individual scores for the AcrySof PanOptix, AcrySof IQ Vivity, TECNIS Eyhance, and AcrySof Aspheric Monofocal IOL for (A) Questions 1–7 and (B) questions 8–10. |
Questionnaire Evaluation
Statistical analysis was conducted to assess the normality of the individual questions. All items except one exhibited significant negative skew and positive kurtosis, with respondents more likely to endorse favorable ratings (>50% of respondents answered 9 or above). The exception was Question 10 (“Does glare and halo at night limit your activities?”), which was significantly positively skewed (75% answered “no”). All subjects were retained, and no corrections were included in the subsequent reliability and validity analysis for reasons described in the discussion.
Instrument Performance
Cronbach’s alpha for all 10 items was calculated to determine internal consistency among the survey items. The survey demonstrated an acceptable moderate to strong internal consistency with all items included (Cronbach’s Alpha = 0.785). An iterative item assessment showed only marginal improvement if items were dropped from the survey. Dropping Question 9 (“Does glare and halo at night limit your activities?”) would only improve Cronbach’s alpha from 0.785 to 0.805 (Table 2).
 |
Table 2 Item Total Statistics Description |
Beyond internal consistency measures, specific subjective measures intended to assess the quality of vision were analyzed. Satisfaction with distance vision without glasses (question 1) and satisfaction with near vision without glasses (question 3) were correlated with objective measures of visual acuity including BUDVA and BUNVA obtained during postoperative examinations (Figure 4). This was done to assess the validity (face and criterion) of the subjective measure.
To assess construct validity, an exploratory factor analysis (EFA) was conducted on the seven 1–10 scale items. KMO and Bartlett’s test demonstrated an average strength of partial correlation (KMO = 0.736) and an appropriate correlations matrix (X² = 1173.461; p < 0.001), indicating sufficient confidence to perform an EFA (Table 3). The EFA resulted in two components with Eigenvalues above 1, representing 43.76% and 18.74% of the total variance explained. The pattern matrix indicated that question 1 (distance vision: factor loading = 0.871), question 5 (meets expectations: 0.800), and question 6 (lens choice: 0.775) significantly contributed to component 1. Questions 2 (intermediate vision: 0.642), question 3 (near vision: 0.926), and question 4 (quantity of glasses independence: 0.825) significantly contributed to component 2. These findings suggest that the survey likely has two components, with a low inter-component correlation (r = 0.238).
 |
Table 3 Inter-Item Correlation Matrix |
Regression analyses were conducted to predict responses to Questions 8 (“Would you choose the same lenses again?”) and 9 (“Are you bothered by glare and halo at night?”) using the seven previous items. A significant model was found (R² = 0.350, F(7, 474) = 35.86, p < 0.001), with quality of near vision (β = 0.188, p < 0.001), quantity of glasses independence (β = 0.116, p < 0.05), and lens choice (β = 0.434, p < 0.001) being significant predictors of choosing the same lenses again. The prediction of being bothered by glare and halo at night was also significant (R² = 0.133, F(7, 472) = 10.23, p < 0.001), with quality of near vision (β = 0.279, p < 0.001) and quantity of glasses independence (β = 0.112, p < 0.05) being significant predictors.
Discussion
Due to the continual development of new advanced technology IOLs, it is important to have a reliable tool to track patient outcomes and performance. The primary objective of this study was to validate the RCSS as an objective method for evaluating patient satisfaction and visual outcomes following refractive cataract surgery. Our data affirms the survey’s reliability and validity, exhibiting moderate to strong internal consistency which could be marginally improved by excluding Question 9. However, Question 9 was retained due to its critical role in assessing IOL dysphotopsia, which is vital for evaluating lens performance.15–19
Overall, statistical analysis revealed a significant negative skew and positive kurtosis across most survey items, suggesting high levels of patient satisfaction. Overall, high patient satisfaction is likely due to achieving good refractive outcomes with minimal refractive error (Figure 2). The one exception is Question 10 (“Does glare and halo at night limit your activities”), where the desirable answer is “No”. As 75% of patients responded “No”, this positively skewed the results. Consequently, all subjects were retained, and no corrections were included in the reliability and validity analysis. While these factors slightly impact the follow-up analyses, this distribution likely represents the true variability in this specific group and accurately reflects the variability following cataract extraction with specific presbyopia-correcting IOLs.
Interestingly, the analysis identified key factors correlating with high patient satisfaction (Question 8: “Would you choose the same lenses again?”). The quality of near vision and the level of glasses independence were significant predictors of lens choice satisfaction. Thus patients who had better near and intermediate vision were overall happier with their IOL choice. These factors are pivotal for clinicians in guiding treatment plans and IOL selection during presurgical consultations. Patients’ perceptions of technical quality strongly translate to patient satisfaction.20
On the other hand, significant predictors for patient dissatisfaction involved the severity of dysphotopsias. Patients who had dysphotopsias which limited their daily activities (eg, night driving) were associated with worse overall visual satisfaction, including the quality of their near vision and spectacle independence. This underscores the importance of thorough preoperative discussions to manage expectations about potential visual disturbances.21,22 In our experience, diffractive dysphotopsia can be minimized by reduced residual refractive error with laser vision enhancement, aggressively treating any dry eye disease, or miotic agents. We have also shown that early intervention (one to three months) with YAG capsulotomies in select patients with any degree of capsular opacities or wrinkles has decreased the level and severity of dysphotopsias.15 Even subtle capsular wrinkles have been documented to decrease contrast and induce a greater level of dysphotopsia compared to post-YAG patients.15
The RCSS offers multiple advantages for widespread clinical use. For one it is very efficient, requiring on average 3 minutes to complete. Secondly, it enables early identification of potentially dissatisfied patients which is crucial in highly comanaged clinics. It is not uncommon for some patients to have very good objective visual acuity yet be very dissatisfied with the quality of their vision. Thus the RCSS will allow comanaging providers to find these unhappy patients sooner in order to start the appropriate intervention which may involve dry eye treatment, early YAG capsulotomy, or laser vision enhancement for significant refractive error. On the other hand, it also allows clinicians to find the extremely happy patients who can be targeted for good online reviews.
There are many surveys that assess visual quality after cataract surgery and some that specifically target refractive outcomes.11,12 Table 4 summarizes the strengths and limitations of our survey and others.3,4,23–25 Our survey is concise, simple, and efficient, eliminating the challenge of lower response rates and accuracy that can accompany longer and less relevant counterparts.13,26,27 We administer this survey verbally when patients return for their 30-day post-surgical follow-ups, additionally reducing the noncompliance. Other studies have shown that while surveys are integral tools for patient assessments, the need for change indicated by the survey might be overlooked.28 RCSS directs administrators to schedule patients for a follow-up with the surgeon if any value falls below 6. Additionally, for such a short survey, the RCSS thoroughly addresses visual performance, patient satisfaction, and customer service.
 |
Table 4 Refractive Surveys |
Limitations and Future Studies
We recognize the RCSS has serval limitations and opportunities for future studies. We recommend that the RCSS should be cross-validated with other clinicians and clinics that may be geographically or demographically distinct. This will help to ensure broader applicability and reliability of the survey. Further research should also focus on assessing the test-retest reliability and repeatability of the RCSS to confirm the stability of patient responses over time and ensure consistent survey performance across different time points. Despite these limitations, the RCSS serves as a valuable tool in clinical settings due to its brevity and comprehensive capture of essential patient satisfaction and visual outcome data.
In conclusion, the RCSS is validated as a robust, reliable tool for assessing patient satisfaction and performance in refractive cataract surgery. The quality of near vision and the level of glasses independence were significant predictors of lens choice satisfaction while the severity of dysphotopsia was a significant negative predictor. The efficient nature of the RCSS allows for early identification and treatment of dissatisfied patients, making it indispensable in heavily comanaged clinical practices.
Funding
No public or private support for all authors.
Disclosure
Dr Wyche Coleman III reports personal fees from Alcon, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Slattery EL, Voelker CCJ, Nussenbaum B, et al. A practical guide to surveys and questionnaires. Otolaryngol-Head Neck Surg. 2011;144(6):831–837. doi:10.1177/0194599811399724
2. Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-item national eye institute visual function questionnaire. Arch Ophthalmol. 2001;119(7):1050–1058. doi:10.1001/archopht.119.7.1050
3. Kandel H, Khadka J, Lundström M, et al. Questionnaires for measuring refractive surgery outcomes. J Refract Surg. 2017;33(6):416–424. doi:10.3928/1081597x-20170310-01
4. Pesudovs K, Garamendi E, Elliott DB. The quality of life impact of refractive correction (QIRC) questionnaire: development and validation. Optometry Vision Sci. 2004;81(10):769. doi:10.1097/00006324-200410000-00009
5. Cacho-Martínez P, Cantó-Cerdán M, Lara-Lacárcel F, García-Muñoz Á. Validation of the symptom questionnaire for visual dysfunctions (SQVD): a questionnaire to evaluate symptoms of any type of visual dysfunctions. Trans Vision Sci Technol. 2022;11(2):7. doi:10.1167/tvst.11.2.7
6. McAlinden C, Pesudovs K, Moore JE. The development of an instrument to measure quality of vision: the quality of vision (QoV) questionnaire. Invest Ophthalmol Visual Sci. 2010;51(11):5537–5545. doi:10.1167/iovs.10-5341
7. Pérez-Mañá L, Cardona G, Pardo-Cladellas Y, et al. Validation of the Spanish version of the low vision quality of life questionnaire. J Optometry. 2022;15(3):199–209. doi:10.1016/j.optom.2021.01.004
8. Thayaparan AJ, Mahdi E. The patient satisfaction questionnaire short form (PSQ-18) as an adaptable, reliable, and validated tool for use in various settings. Med Educ Online. 2013;18(1):21747. doi:10.3402/meo.v18i0.21747
9. Seth I, Bulloch G, Thornell E, Lundström M, Agarwal S. Catquest-9SF questionnaire shows greater visual functioning in bilateral cataract populations: a prospective study. Indian J Ophthalmol. 2022;70(11):3820–3826. doi:10.4103/ijo.IJO_736_22
10. Pesudovs K, Garamendi E, Elliott DB. The contact lens impact on quality of life (CLIQ) questionnaire: development and validation. Invest Ophthalmol Visual Sci. 2006;47(7):2789–2796. doi:10.1167/iovs.05-0933
11. Lundström M, Pesudovs K. Questionnaires for measuring cataract surgery outcomes. J Cataract Refract Surg. 2011;37(5):945–959. doi:10.1016/j.jcrs.2011.03.010
12. Khoramnia R, Auffarth G, Łabuz G, Pettit G, Suryakumar R. Refractive outcomes after cataract surgery. Diagnostics. 2022;12(2):243. doi:10.3390/diagnostics12020243
13. Rolstad S, Adler J, Rydén A. Response burden and questionnaire length: is shorter better? A review and meta-analysis. Value Health. 2011;14(8):1101–1108. doi:10.1016/j.jval.2011.06.003
14. Kost RG, Correa da Rosa J. Impact of survey length and compensation on validity, reliability, and sample characteristics for ultrashort-, short-, and long-research participant perception surveys. J Clin Transl Sci. 2018;2(1):31–37. doi:10.1017/cts.2018.18
15. LoBue S, Martin C, Benson K, Trosclair K, Shelby C, Coleman W. The role of early Nd:YAG laser capsulotomy in improving visual performance in mild to moderately symptomatic trifocal patients. Clin Ophthalmol. 2023;17:3991–4000. doi:10.2147/opth.s448784
16. Welch N, Gregori N, Zabriskie N, Olson R. Satisfaction and dysphotopsia in the pseudophakic patient. Canadian J Ophthalmol. 2010;45(2):140–143. doi:10.3129/i09-266
17. Kim JA, Ha A, Kwon J, Wee W, Han Y. Clinical characteristics and patient’s satisfaction in pseudophakic ne gative dysphotopsia. J Korean Ophthalmol Soc. 2014;55(5):669–678.
18. Kinard KI, Jarstad A, Olson R. Correlation of visual quality with satisfaction and function in a norm al cohort of pseudophakic patients. J Cataract Refract Surg. 2013;39(4):590–597.
19. Jenny Q. H, Sella R, Afshari N. Dysphotopsia: a multifaceted optic phenomenon. Curr Opin Ophthalmol. 2018;29(1):61–68.
20. Ziaei H, Katibeh M, Eskandari A, et al. Determinants of patient satisfaction with ophthalmic services. BMC Res Notes. 2011;4(1):7. doi:10.1186/1756-0500-4-7
21. Salvin KA. The influence of preoperative counselling on the incidence and the ada ptation of postoperative dysphotopsia. J Coll Ophthal SL. 2022;28(2):83–85. doi:10.4038/jcosl.v28i2.64
22. Bhalla JS, Gupta S. Dysphotopsia-unraveling the enigma. DJO. 2016;27(2):97–101. doi:10.7869/djo.217
23. Nichols JJ. Reliability and validity of refractive error–specific quality-of-life instruments. Arch Ophthalmol. 2003;121(9):1289. doi:10.1001/archopht.121.9.1289
24. Schein OD. The measurement of patient-reported outcomes of refractive surgery: the refractive status and vision profile. Trans Am Ophthalmol Soc. 2000;98:439–469.
25. Buckhurst PJ, Wolffsohn JS, Gupta N, Naroo SA, Davies LN, Shah S. Development of a questionnaire to assess the relative subjective benefits of presbyopia correction. J Cataract Refract Surg. 2012;38(1):74–79. doi:10.1016/j.jcrs.2011.07.032
26. Roszkowski MJ, Bean AG. Believe it or not! Longer questionnaires have lower response rates. J Bus Psychol. 1990;4(4):495–509. doi:10.1007/BF01013611
27. Burchell B, Marsh C. The effect of questionnaire length on survey response. Qual Quant. 1992;26(3):233–244. doi:10.1007/BF00172427
28. Eckerlund I, Jönsson B, Tambour M, Westlund AH. Change-oriented patient questionnaires--testing a new method at three departments of ophthalmology. Int J Health Care Qual Assur. 1997;10(7):254–259. doi:10.1108/09526869710191754
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.