Back to Journals » International Journal of Women's Health » Volume 17
The Role of Preventive Nursing Interventions in Reducing Treatment-Related Complications in Ovarian Cancer Patients: A Retrospective Cohort Study
Received 12 March 2025
Accepted for publication 27 June 2025
Published 17 July 2025 Volume 2025:17 Pages 2133—2144
DOI https://doi.org/10.2147/IJWH.S527948
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Matteo Frigerio
Jing Zhang,1 Qiugui Liu2
1Department of Gynaecology and Obstetrics, Tangdu Hospital, Fourth Military Medical University, Xi’an, 710038, People’s Republic of China; 2Department of Oncology, Tangdu Hospital, Fourth Military Medical University, Xi’an, 710038, People’s Republic of China
Correspondence: Qiugui Liu, Department of Oncology, Tangdu Hospital, Fourth Military Medical University, Xi’an, 710038, People’s Republic of China, Email [email protected]
Objective: To evaluate the effectiveness of preventive nursing interventions in reducing treatment-related complications among patients with ovarian cancer.
Setting: Retrospective cohort study.
Participants: A total of 251 female patients with ovarian cancer were included. They were assigned to either a control group (n=134), receiving standard nursing care, or an observation group (n=117), receiving additional preventive nursing interventions.
Interventions: The control group received standard nursing care, including routine health education, pharmacological symptom control, and vital sign monitoring.
Primary and Secondary Outcome Measures: The primary outcome was the incidence of treatment-related complications. Secondary outcomes included the severity of nausea and vomiting, quality of life, psychological condition, and nursing satisfaction.
Results: The observation group demonstrated a significantly lower incidence of treatment-related complications compared to the control group (P=0.001). Notable reductions in nausea, vomiting, and neuropathy were observed (P=0.015, P=0.035). Both groups showed improvements in psychological conditions post-intervention (P< 0.001); however, improvements were more significant in the observation group for depression and quality of life (P=0.004, P=0.007). Nursing satisfaction was also significantly higher in the observation group (P< 0.0001). Multivariate logistic regression revealed that preventive nursing interventions significantly reduced complication risks (OR=0.391, 95% CI: 0.228– 0.670, P =0.001), and treatment with carboplatin and paclitaxel was significantly related to increased complication risks.
Conclusion: Preventive nursing interventions effectively reduce treatment-related complications and enhance clinical and psychological outcomes in patients undergoing ovarian cancer chemotherapy. These findings underscore the importance of personalized, proactive nursing care in oncology settings.
Keywords: ovarian cancer, preventive nursing, treatment-related complications, quality of life, retrospective study
Introduction
Ovarian cancer is the seventh most common cancer and the eighth leading cause of cancer-related death among women worldwide. It is characterized by a high recurrence rate and significant morbidity.1 Tumor biomarkers such as BRCA1/2 mutations and homologous recombination deficiency have been increasingly used to predict chemotherapy response and guide personalized treatment strategies.2 Recent advances in molecular profiling have led to the development of targeted inhibitors for specific genetic alterations in ovarian cancer, with several agents currently undergoing evaluation in clinical trials.3 Despite therapeutic advances, the management of ovarian cancer remains complex, largely because it is frequently diagnosed in late stages and accompanied by numerous treatment-related complications. These complications can often adversely affect treatment outcomes and quality of life, underscoring the need for strategies to mitigate treatment-related complications.4
Nausea and vomiting are among the most debilitating complications of chemotherapy, with 58.1% of ovarian cancer patients experiencing nausea and 31.0% experienced vomiting after chemotherapy.5 These symptoms impair patients’ ability to maintain adequate nutrition and hydration, leading to a cascade of negative effects, including dehydration, electrolyte imbalances, and a deterioration in overall health status, ultimately impacting treatment adherence and quality of life.5,6 Chemotherapy-induced mucositis, characterized by painful oral lesions, inflammation, dysphagia, diarrhea, weight loss, rectal bleeding, and infection, can impair nutritional intake and the functionality of the oral and gastrointestinal mucosa.7 Chemotherapy-induced peripheral neuropathy, with a prevalence of 30–70%, can lead to significant functional impairments, severely limiting patients’ daily activities and overall quality of life.8 This condition often results in symptoms such as tingling, numbness, and pain, which can hinder mobility and the ability to perform routine tasks.9 Other complications can significantly complicate treatment and recovery in patients with ovarian cancer. Thrombus formation, often associated with prolonged immobility and certain chemotherapeutic agents, can result in life-threatening conditions such as pulmonary embolism.10 Meanwhile, intestinal obstruction frequently arises from tumor growth or adhesions and may necessitate hospitalization for surgical intervention.11 Hydronephrosis can occur due to obstruction in the urinary tract, which is often secondary to external compression from pelvic tumors including ovarian cancer, and may result in increased renal pressure, kidney damage, and potential acute kidney injury.12 The hematological complications (anemia, thrombocytopenia, and neutropenia) can lead to severe clinical consequences, thus effective management of these complications is essential in the care of cancer patients.13–15 Prior research indicates that timely management of treatment-related complications can lead to better clinical outcomes and reduce healthcare costs.16
Given the complex nature of ovarian cancer treatment, which often involves combinations of surgery, chemotherapy, and radiation, there is a substantial burden of treatment-related complications that can be mitigated through effective nursing care.17,18 Preventive nursing refers to nursing interventions where nurses anticipate and address patients’ psychological and physiological needs before problems arise.19 It is a structured set of proactive, nurse-led interventions designed to minimize the risk of predictable treatment-related complications, emphasizing proactive intervention and personalized care,17,18,20–22 providing effective individualized communication for delivering tailored health education,20 offering guidance on patients’ diet, physical health and psychological health,23–27 as well as providing continuous care and monitoring.28 A study has shown that implementing preventive nursing in ovarian cancer patients can improve their coagulation index and reduce the occurrence of deep vein thrombosis.29 Additionally, preventive nursing is highly effective in preventing postoperative urinary tract infections in ovarian cancer patients.30 However, regarding treatment-related complications, the effectiveness of preventive nursing in ovarian cancer remains unknown.
This retrospective study aims to evaluate the effectiveness of preventive nursing interventions in reducing treatment-related complications among ovarian cancer patients. By analyzing historical medical records and patient outcomes, this research seeks to provide empirical evidence for integrating preventive nursing into standard oncology care.
Methods
Study Population
A retrospective analysis was conducted using medical records of ovarian cancer patients who received chemotherapy between January 2020 and December 2021 at our hospital. The inclusion criteria were as follows: (1) pathologically confirmed ovarian cancer; (2) age ≥ 18 years; (3) receipt of chemotherapy; (4) complete medical records available; (5) completion of the questionnaires; (6) receipt of either standard nursing care or preventive nursing care for at least 6 months. Patients were excluded if they had severe comorbidities such as significant hepatic or renal dysfunction and severe cardiovascular or cerebrovascular diseases, had undergone any cancer treatment within the previous five years, or were expected to survive less than six months.
Group
Patients were categorized into the control group and the observation group based on their treatment histories in medical records.
The control group received standard nursing care, which included routine health education, pharmacological management for symptom control, and regular monitoring of vital signs. Specifically, this standard care encompassed:
(1) Health Education: Patients received information about their diagnosis, treatment options, and potential treatment-related complications, including self-monitoring of gastrointestinal and neurologic symptoms.
(2) Pharmacological Management: Appropriate medications were prescribed to manage symptoms such as pain and nausea.
(3) Monitoring: Nurses conducted regular assessments of patients’ vital signs, including blood pressure and heart rate, and carefully tracked any adverse drug reactions.
The observation group received preventive nursing interventions in addition to standard care. All oncology nurses completed a two-hour training workshop, followed by monthly fidelity audits. The preventive nursing interventions included:
(1) Pre-treatment profiling: Establish comprehensive patient profiles before initiating treatment to fully understand their medical history and lifestyle, identify risk factors, and evaluate probable adverse reactions. This information provides a foundation for tailored health education and follow-up care, as emphasized in prior studies which highlight the importance of individualized patient profiles in cancer care.20–22
(2) Individualized communication: Nurses proactively engaged in one-on-one conversations with patients to design personalized health education plans based on their specific age, medical condition, cultural background, and comprehension abilities. Detailed explanations were provided about the disease, potential complications of chemotherapy, and measures to prevent complications, enhancing the patients’ understanding of their health.20
(3) Dietary guidance: Patients were advised to consume small, nutritionally rich, and well-balanced meals frequently, incorporating fresh vegetables and fruits, and consciously supplementing with iron and folic acid. Antiemetic drugs were prescribed preemptively for patients at high risk of nausea and vomiting, consistent with reviews that recommend proactive dietary management in cancer care.23,31
(4) Physical activity education: Patients and their family were educated on the benefits of physical activity in preventing complications during chemotherapy. They were encouraged to engage in suitable exercises regularly to aid in mental relaxation and emotional stability, including walking, climbing stairs, jogging, yoga, and Tai Chi.24–26
(5) Psychological health guidance: Active and positive communication with patients before treatment to assess their psychological state, alleviate negative emotions, and present successful cases to boost their confidence. Throughout the treatment, medical staff closely monitored the patients’ psychological health using the Self-Rating Depression Scale (SDS) and the Self-Rating Anxiety Scale (SAS), patiently soothing their emotional states, and helping them avoid the severe consequences of negative emotions such as fear and stress, as outlined in studies on the significance of psychological support in cancer care.27,32
(6) Ongoing care and monitoring: Biweekly follow-ups were conducted through various methods, including WeChat, phone calls, and home visits. Regular assessments of patients were conducted, and preventive and management strategies were tailored to their current conditions. Patients were instructed to regularly visit the hospital for routine blood tests and checks of liver and kidney functions; any abnormalities were addressed promptly, reflecting the necessity for comprehensive follow-up and monitoring of cancer patients during and after treatment to ensure timely interventions and support for their evolving healthcare needs.33,34
Outcome Measures
Demographic data were collected, including age, BMI, pathological stage, smoking history, histology, and chemotherapy regimen. The primary outcome, the incidence of treatment-related complications, was assessed through direct observation and reporting by nursing staff during routine follow-ups. Specifically, the study monitored complications such as nausea, vomiting, neuropathy, thrombosis, intestinal obstruction, hydronephrosis, and anemia. Secondary outcomes included the severity of nausea and vomiting, quality of life, psychological condition, and nursing satisfaction. Severity of nausea and vomiting was assessed using the Multinational Association of Supportive Care in Cancer (MASCC) antiemesis tool. The MASCC antiemesis tool is designed to evaluate the severity of nausea and vomiting with 8 items rated on a Likert-10 scale, where a higher score indicates more severe symptoms.35 Quality of life was measured using the 36-item short-form (SF-36) health survey, which evaluates eight dimensions of health.36 Higher scores indicate better quality of life. Patient anxiety and depression were assessed using SDS and SAS, with higher scores indicating more severe symptoms.37,38 Nursing satisfaction was evaluated using a hospital- designed Nursing Satisfaction Scale. This scale ranges from 0 to 10, where a score of 0–3 indicates dissatisfaction, 4–7 indicates moderate satisfaction, and 8–10 signifies high satisfaction.
Statistical Analysis
Statistical analysis was performed using SPSS 26.0 (IBM Corp., Armonk, NY, USA). Normality of continuous variables was assessed using the Shapiro–Wilk test. Non-normality distributed variables were expressed as median and interquartile range (IQR) and compared using the Mann–Whitney U-test for between-group comparisons and Wilcoxon signed-rank test for within-group comparisons. Categorical variables were presented as frequencies (percentages) and analyzed using the Chi-square test or Fisher’s exact test. Factors potentially influencing the development of complications were first identified using univariate logistic regression. Variables with a P-value less than 0.10 were considered for multivariate analysis and the results were presented as odds ratios (ORs) with 95% confidence intervals (CIs). Two-tailed P-value of less than 0.05 was considered statistically significant.
A retrospective post hoc power analysis was conducted based on the primary outcome. The observed incidence was 35.9% in the intervention group and 57.5% in the control group. With an α level of 0.05 and a total sample size of 212 patients, the calculated statistical power exceeded 0.90, indicating that the study was adequately powered to detect the observed difference between groups.
Results
Baseline Characteristics
The study analyzed 251 patients with ovarian cancer, consisting of 117 in the observation group and 134 in the control group. Baseline demographic and clinical characteristics were comparable between the two groups. Details were summarized in Table 1.
 |
Table 1 Baseline Characteristics of Included Patients |
Complication Rates
There was a statistically significant difference in the incidence of complications between the groups after intervention. The observation group had a lower rate of patients experiencing complications post-intervention (P = 0.001). Specifically, significant reductions were observed in the rates of nausea and vomiting (P = 0.015) and neuropathy (P = 0.035) compared to the control group. However, there were no significant differences in other complications such as thrombosis, intestinal obstruction, hydronephrosis, and anemia (Table 2). Patients who experienced nausea and vomiting were further evaluated for the severity of symptoms with MASCC antiemesis tool. The results showed that the observation group experienced significantly fewer episodes of vomiting (P=0.005) and lower levels of nausea (P<0.001) compared to the control group after the completion of chemotherapy (Table 3).
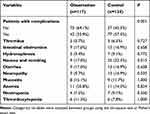 |
Table 2 Post-Intervention Patient Complication Rates |
 |
Table 3 Delayed Nausea and Vomiting After Completion of Chemotherapy |
Quality of Life, Psychological Impact and Patient Satisfaction
Regarding the psychological impact, anxiety and depression scores were significantly improved post-intervention in both observation and control group (P<0.001). However, both SAS (P=0.012) and SDS (P=0.004) scores improved more in the observation group compared to the control group (Table 4). The observation group also had significantly higher SF-36 scores than the control group (P=0.007) (Figure 1). Additionally, patient satisfaction with nursing care was significantly higher in the observation group (P<0.0001) (Figure 2).
 |
Table 4 Differences in SAS and SDS Scores of Patients Before and After Intervention |
 |
Figure 1 Quality of life of two groups after intervention. **indicated P<0.01. |
 |
Figure 2 Patient satisfaction of two groups after intervention. ****indicated P<0.0001. |
Risk Factors for Complication Rates
Univariate logistic regression analysis indicated that the preventive nursing intervention significantly reduced the risk of complications among patients (OR=0.404, 95% CI: 0.233–0.699, P=0.001). Additionally, a BMI ≥30 was significantly related with increased complication risks in patients (OR=2.081, 95% CI: 1.072–4.038, P=0.030). Cancer stage also influenced complications, with Stage II patients experiencing fewer complications than Stage I (OR=0.463, 95% CI: 0.241–0.890, P=0.021). Treatment with carboplatin and paclitaxel showed a trend towards increasing the risk of complications (OR=1.926, 95% CI: 1.045–3.551, P=0.036). After adjusting for the above factors in the multivariate logistic regression model, the preventive nursing intervention remained related to the reduced patient complications (OR=0.391, 95% CI: 0.228–0.670, P =0.001). The influence of BMI and cancer stage was diminished in the multivariate model, indicating that the intervention’s effect holds independently of these factors. The adjusted odds ratios for BMI and cancer stage did not reach statistical significance, highlighting the intervention’s primary role in reducing complications. However, treatment with carboplatin and paclitaxel were still significantly related to increased complication risks in the multivariate model (Table 5 and Table S1).
 |
Table 5 Logistic Regression Analysis of Factors Affecting Patient Complications |
Discussion
This retrospective study highlights the significant impact of preventive nursing interventions on reducing treatment-related complications in ovarian cancer patients. The findings align with previous research, indicating that preventive nursing interventions can enhance clinical outcomes during complex cancer treatments.39,40 The observed reductions in nausea, vomiting, and neuropathy further support the effectiveness of the nursing strategies applied. These outcomes reinforce the importance of individualized patient education and proactive symptom management in oncology nursing.22,41 These effects may be attributed to early dietary guidance, strict adherence to antiemetic protocols, and timely monitoring of gastrointestinal symptoms. In terms of neuropathy, early recognition of sensory changes and patient education on avoiding exacerbating factors enable nurses to coordinate with the medical team for potential dose adjustments or symptomatic treatments, thereby mitigating the progression of neuropathic symptoms. The absence of significant differences in complications such as thrombosis, obstruction, and hydronephrosis may be due to their close association with underlying disease pathology or their dependence on medical or surgical management beyond nursing scope. Furthermore, the significant improvements in quality of life and nursing satisfaction observed in the preventive nursing group suggest that patient-centered care may play an important role in enhancing the overall treatment experience and perceived outcomes among cancer patients. These results are consistent with previous studies, which document the importance of comprehensive care approaches in improving patient-reported quality of life outcomes in chronic illness.41,42 Such holistic improvements may be particularly meaningful in ovarian cancer care, given the considerable physical and psychological burdens commonly experienced by patients during treatment. In the context of current ovarian cancer nursing care, our findings reinforce the importance of integrating preventive nursing interventions into standard practice. While standard nursing care addresses patient needs reactively, our study suggest that preventive interventions may help reduce the severity and incidence of treatment-related complications, which in turn could be associated with improved patient outcomes and satisfaction.
The potential role of preventive nursing in mitigating psychological distress is supported by the observed improvements in anxiety and depression scores following the intervention. The proactive assessment and management of psychological health, as part of preventive nursing, likely contributed to these outcomes. Mental health support is pivotal, as it can substantially influence patient adherence to treatment and overall well-being. Poor mental health can hinder treatment adherence, highlighting the necessity for robust psychological support systems in oncological care settings.43 Our findings suggested that incorporating psychological assessments and interventions into routine nursing care can significantly benefit patients, confirming the role of nurses in providing psychological support.
Interestingly, our analysis also revealed that while factors such as BMI and cancer stage influenced complication rates, the impact of these factors was diminished in the multivariate model, highlighting the primary role of preventive nursing interventions over these demographic and clinical variables. This emphasizes that, although patient characteristics and disease stage are significant, the quality and scope of nursing care are more decisive in determining patient outcomes. This finding aligns with research indicating that individualized nursing interventions can significantly influence health outcomes, overshadowing some clinical and demographic factors.44 This suggested that high-quality care is effective across diverse patient populations. This insight is valuable for current nursing practices, indicating that allocating resources to preventive care strategies can bring significant benefits regardless of the patient’s demographic data.
However, our study also noted that treatment with carboplatin and paclitaxel was associated with increased complication risk, which remains significant even after adjusting for other factors. This underscores the inherent toxicity of this regimen, which, despite its status as first-line treatment for ovarian cancer, poses substantial challenges due to its side-effect profile. Despite its relative tolerability compared to other regimens, studies demonstrate that carboplatin-paclitaxel treatment can lead to serious hematologic and neuropathic complications, which contribute to dose reductions or delays and consequently affect therapeutic outcomes.45 Supporting this, Machida et al discuss the complications related to neoadjuvant chemotherapy with carboplatin and paclitaxel in ovarian cancer patients, emphasizing the prevalence of adverse events and their impact on therapy continuation.46 The integration of specialized nursing care addressing chemotherapy-related complications is associated with improved adherence and quality of life, and may support more favorable clinical trajectories.
Limitations of our study include its retrospective nature, which inherently restricts the ability to establish causality, the possibility of unmeasured confounding, selection bias, and limited control over data completeness. This bias may arise because patients who receive more comprehensive nursing care might also be those who are generally more engaged in their healthcare. Consequently, the results could reflect differential health outcomes based on levels of patient engagement rather than nursing interventions alone. Besides, some subgroup comparisons were based on relatively small sample sizes. As a result, these findings should be interpreted with caution due to the potential for reduced statistical power and wider confidence intervals. To mitigate these limitations and enhance the validity of our findings, future studies could benefit from a prospective design and a larger sample size. Such studies would enable a more controlled examination of the effects of preventive nursing interventions on patient outcomes, ensuring that findings are robust and generalizable. In addition, this study was conducted in a single institution, which may limit the generalizability of the findings. Although similar nursing interventions have shown beneficial effects in cancer patient populations in other hospitals in China and elsewhere internationally, differences in institutional practices and patient characteristics may affect the results.32,47,48 Therefore, multicenter studies in different healthcare settings are necessary to more broadly validate the effectiveness and adaptability of this intervention.
Conclusion
In conclusion, our study provides observational evidence that integrating preventive nursing interventions into the treatment regimen of ovarian cancer patients may effectively reduce treatment-related complications. These interventions were associated with a lower incidence of treatment-related complications, as well as improvements in the overall quality of life, satisfaction, and psychological well-being. This multifaceted impact highlights the relevance of a comprehensive, patient-centered approach in oncology nursing. Nonetheless, further confirmation through large-scale, multi-center prospective studies is warranted to validate these findings and assess their generalizability.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Air Force Medical University Tangdu Hospital in accordance with the Declaration of Helsinki. Due to its retrospective nature, the requirement for informed consent was waived by the Ethics Committee of the Second Affiliated Hospital of Air Force Medical University Tangdu Hospital. All patient data were kept confidential.
Patient and Public Involvement
It was not appropriate or possible to involve patients or the public in the design, or conduct, or reporting, or dissemination plans of our research.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
1. Gaona-Luviano P, Medina-Gaona LA, Magana-Perez K. Epidemiology of ovarian cancer. Chin Clin Oncol. 2020;9(4):47. doi:10.21037/cco-20-34
2. Tonti N, Golia D’Auge T, Cuccu I, et al. The Role of Tumor Biomarkers in Tailoring the Approach to Advanced Ovarian Cancer. Int J Mol Sci. 2024;26(1):25. doi:10.3390/ijms26010025
3. Perrone C, Angioli R, Luvero D, et al. Targeting BRAF pathway in low-grade serous ovarian cancer. J Gynecol Oncol. 2024;35(4):e104. doi:10.3802/jgo.2024.35.e104
4. Xu Z, Becerra AZ, Justiniano CF, et al. Complications and Survivorship Trends After Primary Debulking Surgery for Ovarian Cancer. J Surg Res. 2020;246:34–41. doi:10.1016/j.jss.2019.08.027
5. Woopen H, Richter R, Chekerov R, et al. Prognostic role of chemotherapy-induced nausea and vomiting in recurrent ovarian cancer patients: results of an individual participant data meta-analysis in 1213. Support Care Cancer. 2020;28(1):73–78. doi:10.1007/s00520-019-04778-1
6. Liu A, Li M, Liu Z, et al. Application of comprehensive unit-based safety program model to improve chemotherapy-induced nausea and vomiting in patients with ovarian cancer: a retrospective study. J Ovarian Res. 2023;16(1):143. doi:10.1186/s13048-023-01230-1
7. Thomsen M, Vitetta L. Adjunctive Treatments for the Prevention of Chemotherapy- and Radiotherapy-Induced Mucositis. Integr Cancer Ther. 2018;17(4):1027–1047. doi:10.1177/1534735418794885
8. Cao A, Cartmel B, Li FY, et al. Effect of Exercise on Chemotherapy-Induced Peripheral Neuropathy Among Patients Treated for Ovarian Cancer: a Secondary Analysis of a Randomized Clinical Trial. JAMA Network Open. 2023;6(8):e2326463. doi:10.1001/jamanetworkopen.2023.26463
9. Bonhof CS, Mols F, Vos MC, et al. Course of chemotherapy-induced peripheral neuropathy and its impact on health-related quality of life among ovarian cancer patients: a longitudinal study. Gynecol Oncol. 2018;149(3):455–463. doi:10.1016/j.ygyno.2018.03.052
10. Tatsumi K. The pathogenesis of cancer-associated thrombosis. Int J Hematol. 2024;119(5):495–504. doi:10.1007/s12185-024-03735-x
11. Randall TC, Rubin SC. Management of intestinal obstruction in the patient with ovarian cancer. Oncology. 2000;14(8):1159–1163.
12. Celano T. Severe Hydronephrosis Secondary to Ovarian Serous Carcinoma. J Diagnost Med Sonography. 2022;38:347–352.
13. Wu Y, Aravind S, Ranganathan G, Martin A, Nalysnyk L. Anemia and thrombocytopenia in patients undergoing chemotherapy for solid tumors: a descriptive study of a large outpatient oncology practice database, 2000- 2007. Clin Ther. 2009;31(2):2416–2432. doi:10.1016/j.clinthera.2009.11.020
14. da Silva RLM, da Silva TTM, Pessoa RL, et al. Use of ginger to control nausea and vomiting caused by chemotherapy in patients with cervical cancer undergoing treatment: an experiment. Medicine. 2022;101(24):e29403. doi:10.1097/MD.0000000000029403
15. Griffiths EA, Roy V, Alwan L, et al. NCCN Guidelines(R) Insights: hematopoietic Growth Factors, Version 1.2022. J Natl Compr Canc Netw. 2022;20(5):436–442. doi:10.6004/jnccn.2022.0026
16. Gordon LG, Scuffham PA, Beesley VL, et al. Medical costs and outcomes for Australian women with ovarian cancer: a patient-level analysis over 2.5 years. Int J Gynecol Cancer. 2010;20(5):757–765. doi:10.1111/IGC.0b013e3181dbd13f
17. Zhao M, Li H, Li X, Wang J, Wang P, Zhao M. Effects of preventive nursing based on quantitative evaluation on psychological state and maternal-infant outcome in patients with gestational diabetes mellitus. J Matern Fetal Neonatal Med. 2023;36(1):2183473. doi:10.1080/14767058.2023.2183473
18. Liu H, Li P, Yu D, et al. Analysis of the Nursing Effect of Anesthesia Care Integration Combined with Preventive Nursing on Older Patients with Lumbar Disc Herniation During the Perioperative Period. Risk Manag Healthc Policy. 2023;16:1001–1009. doi:10.2147/RMHP.S411885
19. Yao D, Tao Z. Preventive nursing reduces the incidence of adverse reactions in patients with ovarian cancer after the use of poly(adenosine diphosphate ribose) polymerase inhibitors. J Cl Pathol Res. 2023;43:394–399.
20. Wittenberg-Lyles E, Goldsmith J, Ferrell B. Oncology nurse communication barriers to patient-centered care. Clin J Oncol Nurs. 2013;17(2):152–158. doi:10.1188/13.CJON.152-158
21. Richmond JP, Kelly MG, Johnston A, Murphy PJ, Murphy AW. Current management of adults receiving oral anti-cancer medications: a scoping review. Eur J Oncol Nurs. 2021;54:102015. doi:10.1016/j.ejon.2021.102015
22. McCorkle R, Ercolano E, Lazenby M, et al. Self-management: enabling and empowering patients living with cancer as a chronic illness. CA Cancer J Clin. 2011;61(1):50–62. doi:10.3322/caac.20093
23. Arends J, Bachmann P, Baracos V, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36(1):11–48. doi:10.1016/j.clnu.2016.07.015
24. Courneya KS, Friedenreich CM. Physical activity and cancer control. Semin Oncol Nurs. 2007;23(4):242–252. doi:10.1016/j.soncn.2007.08.002
25. Baumann FT, Zopf EM, Bloch W. Clinical exercise interventions in prostate cancer patients--a systematic review of randomized controlled trials. Support Care Cancer. 2012;20(2):221–233. doi:10.1007/s00520-011-1271-0
26. Pinto BM, Maruyama NC. Exercise in the rehabilitation of breast cancer survivors. Psychooncology. 1999;8(3):191–206. doi:10.1002/(SICI)1099-1611(199905/06)8:3<191::AID-PON355>3.0.CO;2-T
27. Cordeiro Rde A, Silva KR, Brilhante RS, et al. Coccidioides posadasii infection in bats, Brazil. Emerg Infect Dis. 2012;18(4):668–670. doi:10.3201/eid1804.111641
28. Jacobsen PB, DeRosa AP, Henderson TO, et al. Systematic Review of the Impact of Cancer Survivorship Care Plans on Health Outcomes and Health Care Delivery. J Clin Oncol. 2018;36(20):2088–2100. doi:10.1200/JCO.2018.77.7482
29. Fei M. Influence of predictive nursing on coagulation index and deep vein thrombosis in patients with ovarian cancer after operation. EIec J Pract Gynecol Endocrinol. 2021;8:114–116.
30. Su L, Chen L. Observation of the application effect of predictive nursing in preventing postoperative urinary tract infections of ovarian cancer patients. World Latest Med Inform. 2019;19:360–362.
31. Ravasco P. Nutrition in Cancer Patients. J Clin Med. 2019;8(8):1211. doi:10.3390/jcm8081211
32. Tuominen L, Stolt M, Meretoja R, Leino-Kilpi H. Effectiveness of nursing interventions among patients with cancer: an overview of systematic reviews. J Clin Nurs. 2019;28(13–14):2401–2419. doi:10.1111/jocn.14762
33. Wang J, Liu Y, Zong J, Sun L, Wang C, Fang M. The Effects of WeChat-Based Teach-Back Health Education on Patients With Advanced Cancer Pain. Clin J Oncol Nurs. 2024;28(3):287–296. doi:10.1188/24.CJON.287-296
34. Maguire R, McCann L, Kotronoulas G, et al. Real time remote symptom monitoring during chemotherapy for cancer: European multicentre randomised controlled trial (eSMART). BMJ. 2021;374:n1647. doi:10.1136/bmj.n1647
35. Molassiotis A, Coventry PA, Stricker CT, et al. Validation and psychometric assessment of a short clinical scale to measure chemotherapy-induced nausea and vomiting: the MASCC antiemesis tool. J Pain Symptom Manage. 2007;34(2):148–159. doi:10.1016/j.jpainsymman.2006.10.018
36. Ware JE, Kosinski M. SF-36 physical & mental health summary scales: a manual for users of version 1. Quality Metric. 2001;2001:5.
37. Dunstan DA, Scott N. Norms for Zung’s Self-rating Anxiety Scale. BMC Psychiatry. 2020;20(1):90. doi:10.1186/s12888-019-2427-6
38. Zung WW. A Self-Rating Depression Scale. Arch Gen Psychiatry. 1965;12(1):63–70. doi:10.1001/archpsyc.1965.01720310065008
39. Zhang Q, Li F, Zhang H, Yu X, Cong Y. Effects of nurse-led home-based exercise & cognitive behavioral therapy on reducing cancer-related fatigue in patients with ovarian cancer during and after chemotherapy: a randomized controlled trial. Int J Nurs Stud. 2018;78:52–60. doi:10.1016/j.ijnurstu.2017.08.010
40. Edwards SJ. Prevention and treatment of adverse effects related to chemotherapy for recurrent ovarian cancer. Semin Oncol Nurs. 2003;19:19–39. doi:10.1016/S0749-2081(03)00059-7
41. Hoffman AJ. Enhancing self-efficacy for optimized patient outcomes through the theory of symptom self-management. Cancer Nurs. 2013;36(1):E16–26. doi:10.1097/NCC.0b013e31824a730a
42. Flanagan S, Damery S, Combes G. The effectiveness of integrated care interventions in improving patient quality of life (QoL) for patients with chronic conditions. An overview of the systematic review evidence. Health Qual Life Outcomes. 2017;15(1):188. doi:10.1186/s12955-017-0765-y
43. Shoshani A, Kanat-Maymon Y. Involvement in care in pediatric cancer patients: implications for treatment compliance, mental health and health-related quality of life. Qual Life Res. 2018;27(2):567–575. doi:10.1007/s11136-017-1744-9
44. Suhonen R, Valimaki M, Leino-Kilpi H. A review of outcomes of individualised nursing interventions on adult patients. J Clin Nurs. 2008;17(7):843–860. doi:10.1111/j.1365-2702.2007.01979.x
45. Ozols RF, Bundy BN, Greer BE, et al. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J Clin Oncol. 2003;21(17):3194–3200. doi:10.1200/JCO.2003.02.153
46. Machida H, Tokunaga H, Matsuo K, et al. Survival outcome and perioperative complication related to neoadjuvant chemotherapy with carboplatin and paclitaxel for advanced ovarian cancer: a systematic review and meta-analysis. Eur J Surg Oncol. 2020;46(5):868–875. doi:10.1016/j.ejso.2019.11.520
47. Zhang T, Lu J, Fan Y, Wang L. Evidence-based nursing intervention can improve the treatment compliance, quality of life and self-efficacy of patients with lung cancer undergoing radiotherapy and chemotherapy. Am J Transl Res. 2022;14(1):396–405.
48. Rodrigues C, Gomes B, Albuquerque C. The rehabilitation of cancer patients and the role of nurses: a scoping review. Oncol Clin Pract. 2022;18:147–165.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

