Back to Journals » Journal of Inflammation Research » Volume 17
The Values of PDK1 and LDH Levels in Patients with Sepsis and Septic Shock: A Prospective Observational Study
Authors Liu J, Zhou G, Tong Z, Wang X, Liu D
Received 7 July 2024
Accepted for publication 10 September 2024
Published 30 September 2024 Volume 2024:17 Pages 6815—6826
DOI https://doi.org/10.2147/JIR.S477495
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Jingjing Liu, Gaosheng Zhou, Zewen Tong, Xiaoting Wang, Dawei Liu
Department of Critical Care Medicine, Peking Union Medical College Hospital, Peking Union Medical College, Chinese Academy of Medical Sciences, Beijing, People’s Republic of China
Correspondence: Dawei Liu, Department of Critical Care Medicine, Peking Union Medical College Hospital, Peking Union Medical College, Chinese Academy of Medical Sciences, 1# Shuai Fu Yuan, Dong Cheng District, Beijing, 100730, People’s Republic of China, Tel +86-10-69152305, Email [email protected]
Background: Metabolic changing is the significant host stress response during sepsis, but there is increasing evidence that uncontrolled metabolic reprogramming is a contributing factor to sepsis. Nevertheless, its association with outcome in patients with sepsis has been poorly investigated. As the key enzyme of metabolic reprogramming, the clinical value of PDK1 and LDH in patients with sepsis will be investigated in this study.
Methods: We collected serum from 167 ICU patients within 24 hours of admission for a single-center prospective observational study. The levels of PDK1 and LDH were detected by enzyme-linked adsorption method. Pearson or Spearman coefficient for correlation analysis between PDK1, LDH and clinical indicators. Areas under the ROC curves for evaluation of mortality prediction. Kaplan–Meier survival curve analysis was performed, and Cox proportional hazards model was performed to determine the risk factors for 28-day mortality.
Results: The PDK1/LDH in the septic shock group was statistically different between both the sepsis group and ICU control group, and had good correlation with ScvO2 and lactate. In predicting 28-day mortality in patients with sepsis, the best AUC was observed for PDK1/LDH, and was higher than the AUC for PDK1, lactate, and SOFA. Additionally, patients with lower PDK1/LDH had markerablely higher 28-day mortality. The multivariate Cox proportional hazards model revealed that PDK1/LDH < 0.1808 were the independent risk factors for 28-day mortality in sepsis.
Conclusion: The level of PDK1/LDH at admission was markedly decreased in patients with septic shock, which can serve as a novel independent prognostic biomarker for predicting mortality.
Keywords: sepsis, septic shock, PDK1/LDH, metabolic reprogramming, mortality
Background
Sepsis is defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection.1 Septic shock is a subtype of sepsis with profound circulatory, and cellular metabolic abnormalities.2 The terms “dysregulated” and “host response” are not explicitly defined, but emphasize the significance of the balance of both immune and non-immune systems in the pathogenesis of sepsis.3 Reprogramming of cellular metabolism from oxidative phosphorylation (OXPHOS) to glycolysis during sepsis is an important positive mechanism for the energy balance and confers new functions on cells (eg immune cells).4–6 As the disease progresses into septic shock, however, the metabolic reprogramming shows a severe imbalance, which causes disruption of cellular metabolism7–9 and functional depression,10,11 ultimately leading to immunosuppression and multiple organ dysfunction syndrome (MODS). During sepsis, metabolic reprogramming occurs in almost every cell, but its association with outcome in sepsis patients has been poorly investigated.
In spite of the fact that lactate is an important metabolite for metabolic reprogramming, it cannot indicate the real balance state of metabolic reprogramming due to its complex source and clearance mechanism in sepsis. Therefore, we need a new indicator capable of depicting the metabolic balance state. The pyruvate dehydrogenase (PDH) is the first crucial point in the cellular mitochondrial OXPHOS, which is regulated by pyruvate dehydrogenase kinase (PDK), linking aerobic oxidation of glucose to the tricarboxylic acid cycle (TCA) and OXPHOS. The inactivity of PDH inhibited TCA, causing pyruvate accumulation, massive lactate production, and even the impairment of MODS.12 The inhibition of PDK can rescue systemic energy imbalance and metabolic dysfunction in sepsis partly through restoration of hepatic fuel metabolism,13 targeting PDK1 is a treatable mitochondrial target for promoting immunometabolic and organ homeostasis during sepsis.14 Lactate dehydrogenase (LDH) is another key enzyme in pyruvate metabolism, which can meet the biosynthetic and energy requirements for against infections by catalyzing the conversion of pyruvate to lactic acid.15,16 As the key enzyme at the bifurcation of mitochondrial oxidation and glycolysis, the PDK and LDH determine the metabolic fate of pyruvate and the extent of metabolic shift. It is meaningful to investigate PDK and LDH as indicators of host metabolic reprogramming balance.
PDK and LDH have been shown in numerous in vivo and in vitro experiments to be strongly associated with sepsis outcomes. However, to our knowledge, the role of PDK in human sepsis has never been investigated. In this study, we assessed the serum expression of PDK1 and LDH in different patients within 24h of ICU admission and explored the relationship between serum levels of PDK1, LDH and PDK1/LDH and clinical outcomes of patients with sepsis.
Method
Study Design and Patients
This research is a prospective observational clinical study for discussing clinical values of PDK1 and LDH. After approval by the Peking Union Medical College Hospital (PUMCH) institutional review board (approval number JS-3302), we conducted a single-center prospective observational study of critically ill patients admitted to the ICU within 24 hours at PUMCH from January 2022 to December 2022. Inclusion criteria consisted of adult ICU patients (≥18 years old) with sepsis or septic shock according to the latest diagnostic criteria (Sepsis 3.0).1 Patients who have normal infection indicators and no signs of infection were enrolled in the ICU control group. Exclusion criteria consisted of experience of cancer, pregnant, and refusal to be enrolling.
We obtained informed consent from all enrolled patients through the next of kin of each patient. Our study was performed in accordance with the Declaration of Helsinki and was guided by the sepsis 3.0 diagnostic criteria to ensure the safety of human subjects and sample compliance.
Serum Collection and Detection
We collected arterial blood from all patients within 24 hours of admission to the ICU by indwelling arterial catheter. Blood collected in the anticoagulant tube was centrifuged at 3000 r/min for 10 minutes after standing for 10 minutes, then transferred to an EP tube and stored at −80°C.
After defrosting the frozen serum, we used the human PDK1 ELISA kit (LifeSpan Biosciences, Inc., Seattle, America, Catalog # LS-F12294) to detect the concentration of PDK1, and human LDH ELISA kit (Beijing Solarbio Science & Technology Co., Ltd., Beijing, China, Catalog # BC0685) to detect the level of LDH in the serum.
Clinical Data Collection and Endpoint
All the necessary clinical data about patients were collected, including basic information (age, gender, primary disease, infection site), basic vital signs (blood pressure, heart rate, respiratory rate, body temperature), biochemical examination (WBC, hemoglobin, PCT, IL-6, IL-10, hs-CRP). SOFA score, APACHE II, vasoactive drugs, lactate, central venous oxygen saturation (ScvO2), and other information were also collected. The primary endpoint was mortality at 28 days after ICU admission.
Statistical Analysis
Shapiro–Wilk test for normality of clinical data distribution. Normally distributed data are expressed as SEM and compared by one-way Anova or t-test. Non-normally distributed data are shown as M (P25, P75) and analyzed by Kruskal–Wallis test or Mann–Whitney U-test. The counting data were expressed as rates (%) and tested by χ2. A Pearson or Spearman rank correlation coefficient analysis was for normally or non-normally distributed data. The area under the receiver operating characteristic curve (AUC) was calculated to describe the diagnostic accuracy of PDK1/LDH. The Kaplan-Meier analysis for 28-day survival and the Log rank test for differences in survival rates. Cox proportional hazards model was performed to determine the risk factors for 28-day mortality. Statistical significance was set when p value < 0.05.
Results
Baseline Characteristics of Patients
Data and serum samples from 167 patients were available for analysis. Baseline clinical characteristics according to diagnosis are shown in Table 1. There were 90 patients in the sepsis group (61.96 ±18.53 years, 60% male), 37 in the septic shock group (63.00 ±16.37, 70.3% male), and 40 in the ICU control group (62.38 ±17.77, 32.5% male). The site of infection of patients in the sepsis group and septic shock group was counted: lung (31.1% vs 27.03%), abdomen (45.56% vs 43.24%), central nervous system (12.2% vs 5.4%) bloodstream infection (10% vs 13.51%), or other (13.33% vs 10.81%). The history of previous diseases was also counted in all groups, including hypertension, diabetes, hyperlipidemia, cardiovascular disease, cerebral hemorrhage. No statistically significant difference in infection site and diseases history between the three groups. Inflammatory indicators (TNF-α, IL-10, IL-6), PCT, norepinephrine, oxygenation index (OI), SOFA, RASS, APACHE II, lactate, length of ICU stay, and length of hospital stay were statistically significant between the three groups. No difference in 28-day mortality between the sepsis and septic shock groups (Table 1).
 |
Table 1 Baseline Characteristics of All Patients |
The Serum Levels of PDK1, LDH and PDK1/LDH in Different Patients with ICU
The serum PDK1 level was highest in the sepsis patients and lowest in the ICU control group, but the difference in PDK1 levels only existed between the ICU control and sepsis group (109.0 ± 71.61 vs 149.4 ± 99.54, p=0.036, Figure 1A). LDH levels were significantly higher in septic shock patients than in ICU controls (765.0 ± 4308 vs 515.8 ± 399.5, p=0.010, Figure 1B), but not statistically different from the sepsis group. We analyzed the ratio of PDK1 to LDH among the three groups. The results showed that PDK1/LDH in the septic shock group was statistically different between both the sepsis group (0.197 ± 0.136 vs 0.326± 0.302, p=0.044, Figure 1C) and ICU control group (0.197 ± 0.136 vs 0.289 ± 0.202, p=0.011, Figure 1C).
Correlation with Clinical Indicators in ICU Patients
We assessed correlations between PDK1, LDH and PDK1/LDH and metabolic indicators in clinical patients. PDK1 and LDH correlated with metabolic indicators (ScvO2, lactate) in septic shock group, where PDK1 negatively correlated with lactate (Spearman: r2 =−0.379, p=0.021. Figure 2A) and LDH negatively correlated with ScvO2 (Spearman: r2 =−0.325, p=0.050. Figure 2B). PDK1/LDH showed a positive correlation with ScvO2 (Spearman: r2 = 0.333, p=0.006. Figure 2C) but not with lactate in the sepsis group (Spearman: r2 =−0.142, p=0.118. Figure 2C). In the septic shock group, a significant positive correlation was shown with both ScvO2 (Spearman: r2=0.424, p=0.009. Figure 2D) and lactate (Spearman: r2 =−0.431, p=0.008. Figure 2D). PDK1/LDH showed a better correlation with metabolic indicators in patients with septic shock than other groups.
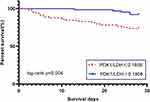
Predictive Value for 28-Day Mortality in Patients with Sepsis
A total of 22 patients died during the 28-day follow-up period. Patients that died had significantly higher levels of PDK1/LDH (p = 0.002) and PDK1 (p = 0.038) compared to those that survived, except the level of LDH (p=0.460, Figure 3A–C). To investigate whether PDK1/LDH is useful in predicting 28-day mortality in patients with sepsis who are critically ill, ROC analysis was conducted for prediction of 28-day mortality using clinical and laboratory markers. Among the six prognostic factors studied (Table 2), the best AUC was observed for PDK1/LDH (AUC, 0.713; 95% CI, 0.589–0.836, p=0.002), and was higher than the AUC for PDK1 (AUC, 0.641; 95% CI, 0.531–0.750, p=0.384), lactate (AUC, 0.619; 95% CI, 0.480–0.758, p=0.079), and SOFA (AUC, 0.603; 95% CI, 0.474–0.732, p=0.129) (Figure 4 and Table 2). With a cutoff value of 0.1407 determined on the ROC curve, Kaplan -Meier survival curves were established. Patients with lower PDK1/LDH had lower survival than patients with higher PDK1/LDH(log-rank P < 0.001, Figure 5).
 |
Table 2 AUC and Optimal Cutoff Points with Their Corresponding Validity Indexes for SOFA and Biomarkers in Relation to 28-Day Mortality of Patients with Sepsis |
 |
Figure 4 The ROC curves of indicators in relation to 28-day mortality of patients with sepsis. AUC was 0.713 (95% CI, 0.589–0.836, p=0.002) for serum PDK1/LDH levels at admission in the patients with sepsis. AUC: area under the curve, ROC curve: Receiver operating characteristic curve. P<0.05 were considered statistically significant. See Table 2 legend for AUC and the corresponding validity indexes of other indicators. |
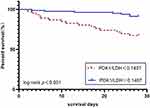 |
Figure 5 Kaplan-Meier survival curves of patients with sepsis based on the PDK1/LDH cutoff value (0.1407). Significant difference was measured between the two curves (P <0.001, Log rank test). |
Prognostic Value of PDK1/LDH in Patients with Sepsis
We verified the prognostic value using a Cox proportional hazard model. In the univariate analysis, we converted PDK1/LDH, PDK1, age, SOFA, and lactate into binary variables using the median and lactate >2mmol in the cohort. With P < 0.1, PDK1/LDH < 0.1808 and lactate <2 mmol/L were screened as key factors influencing 28-day mortality (Table 3). After multivariate analysis, the result showed that PDK1/LDH < 0.1808 independently associated with 28-day mortality (HR=3.478, 95% CI 1.263–9.573, p = 0.016) (Table 3). PDK1/LDH is an independent influence on 28-day mortality in patients with sepsis.
 |
Table 3 Hazard Ratios for Risk Factors Associated with 28-Day Mortality |
When using the Kaplan–Meier estimator again to plot the survival curve with a cut-off value of 0.1808 and assessed survival differences using the Log Rank test again, we also found patients with PDK1/LDH < 0.1808 had a lower 28-day survival rate (log-rank p=0.004, Figure 6) than those with PDK1/LDH ≥0.1808.
Discussion
This is the first study investigating an indicator of metabolic reprogramming in septic patients and assessing the prognostic role of PDK1/LDH in human sepsis. In this study, we found that: (1) The serum levels of PDK1 and LDH have poor clinical value as separate biomarkers, (2) PDK1/LDH levels were significantly lower in patients with septic shock than in patients with sepsis and non-infectious patients, and only correlated well with lactate and Scvo2 in patients with septic shock, (3) PDK1/LDH performed better than other parameters (PDK1, lactate, and SOFA) in predicting 28-day mortality on the day of ICU admission, and patients with lower PDK1/LDH have higher 28-day mortality, and (4) PDK1/LDH was an independent factor influencing 28-day mortality in patients with sepsis. We suggest that PDK1/LDH is an important predictor and prognostic factor for 28-day mortality during sepsis. In addition, PDK1/LDH may provide an indication of the balance of metabolic reprogramming during sepsis, although further research is needed to confirm this.
Reduced OXPHOS and enhanced glycolysis are important features of metabolic reprogramming, predominantly occurring in tumor cells,17,18 which reflect the flexibility of cell metabolism and ensure resistance and tolerance of the cells within certain damage.5,10,19 Rapid energy supply and the large amounts of intermediate metabolites produced by glycolysis also support the immune response.6,20 Low OXPHOS-related ROS may prevent vulnerable cells and mitochondria to be further damaged10,21,22 and reducing OXPHOS may be a protective measure. At some extent, metabolic reprogramming is beneficial for cells during sepsis. Active PDH is a key component of the metabolic reprogramming mechanism in sepsis, and inactivity of PDH phosphorylated by PDK leads to TCA inhibition and reduction in mitochondrial oxygenation capacity.23 We found that sepsis causes PDK1 serum levels to increase compared with ICU controls. This result not only supported the idea that sepsis causes a decrease in PDH activity, it also comes with a new perspective: PDK1 elevation may serve as a protective mechanism in cells during sepsis. Nevertheless, PDH generally regarded as an energy sensing and signaling homeostat that restores metabolic and energy fitness during acute inflammation.24 Zhu et.al25 show that DCA-induced activation of PDH restored anabolic energetics in inflammatory monocytes while increasing TCA cycle intermediates and reversing inflammatory monocyte injury. Active PDH reverses LPS-induced glycolysis, thereby preventing lactate production and monolayer barrier dysfunction in HUVECs,26 improving disrupted metabolic regulation in animals27 and even affecting survival.28 However, no clinical efficacy of serum levels of PDK1 was found in our clinical study within 24 hours of admission to the ICU. We found the serum levels of PDK1 were higher in survivors than in non-survivors, which is contrary to previous findings that suggest inhibition of PDK1 activity contributes to survival. Ferreira et al29 also found PDK1 is differentially expressed in leukocytes from survivors and non-survivors during clinical sepsis. This result reveals the huge gap between in vivo or in vitro experiments and clinical studies again, especially in the metabolism system that supports all cellular functions and responds to environmental factors.
Excessive glycolysis has a potent immunosuppressive effect on immune cells20,30 and induces the release of inflammatory factors,31,32 as well as energy exhaustion can also occur when glycolysis is continuously relied upon for energy. Balancing high energy-consuming danger resistance and low energy supply of disease tolerance is a universal survival principle that often fails during sepsis.5,33 Brealey et al34 showed sepsis non-survivors are characterized by subnormal levels of muscle ATP. As failed organs show minimal to no evidence of cell death, Singer and Giacomo11,35–37 et al have consistently claimed that MODS is a functional shutdown of the organism in the face of energy deficiency during sepsis. This state, akin to hibernation, may even represent an adaptive mechanism, allowing restoration of organ function once the inflammatory process resolves.11 We observed that PDK1 levels did not increase but decreased in patients with septic shock compared to patients with sepsis, which may imply a recovery of PDH activity. The recovery of active PDH can be considered a restoration of mitochondrial oxidative capacity, even though there are other factors (electron transport chain, membrane potential, and so on) that disturb mitochondrial oxidative capacity.34,38–40 Lower PDK1 is necessary to restore mitochondrial oxidative metabolism at this stage. Ferreira et al.29 Ferreira’s study supported this speculation: PDK1 was less expressed in leukocytes from survivors and non-survivors during clinical sepsis at day 7. PDK1 seems to have diametrically opposed effects at early and late stages of sepsis.
In our study, PDK1/LDH showed a significant correlation with lactate and ScvO2 only in the septic shock group, which is not surprising since the lactate and ScvO2 are controlled by both PDK1 and LDH, at the same time, PDK1 or LDH have no independent ability to indicate the metabolic imbalance induced by septic shock. This finding also provided favorable evidence for PDK1/LDH using as a balance indicator of metabolic switch. Although the increased awareness and early effective management of patients with sepsis, the mortality of sepsis remains unacceptably high. Early prediction of mortality has important implications for clinical treatment and intervention. PDK1/LDH in the study showed excellent mortality prediction, even beyond that of lactate. ATP is the basis of cellular life and functional activity. Metabolic pathway affects the production of ATP and is also the most important factor contributing to the life activities of cells. It is reasonable to conclude that PDK1/LDH has a higher predictive capacity as a gatekeeper of the OXPHOS and glycolytic pathways than lactate, considering lactate’s complex physiological cycle. In this research, PDK1/LDH < 0.1808 is an independently associated with 28-day mortality. Metabolic reprogramming is an important manifestation of host response. There is a large of animal and cellular research supporting the non-negligible role of metabolic reprogramming in the immune response to sepsis41,42 and in the development of MODS,10,43 but no relevant clinical studies. Our study firstly demonstrated the clinical value of PDK1/LDH in sepsis and also highlights the important role of metabolic disorders in the prognosis of sepsis.
Some points need to be further clarified and acknowledged. Firstly, although we have clearly demonstrated the clinical value of PDK1/LDH, the study only detected PDK1 and did not determine its clinical value as a separate indicator. Considering that PDK2-4 can also inhibit PDH activity, further assessment of the clinical value of PDK2-4 is necessary for demonstrating the clinical significance of PDKs as a single indicator. Secondly, our study was a single-centre study, and the inadequate sample size may also be an important reason for not obtaining the clinical value of LDH and PDK1, a larger sample size, multi-center studies will be necessary in the future. Thirdly, based on the natural physiological functions of PDK1 and LDH, combined with our findings that PDK1/LDH is an important prognostic factor in patients with sepsis, we hypothesized that PDK1/LDH may be a key indicator of metabolic homeostasis during human sepsis. This is the first study that attempts to find metabolic reprogramming markers in sepsis patients, and we hope that more studies will find better markers in the future than PDK1/LDH.
Conclusion
We found that serum PDK1/LDH measured within 24 hours of ICU admission was both a predictor and an independent factor on 28-day mortality in septic patients, but PDK1 and LDH individually have no significant clinical value, which suggests that PDK1/LDH is a novel indicator for identifying a group of patients with sepsis at high risk of death. It is also possible that PDK1/LDH may indicate the imbalance of metabolic reprogramming during sepsis, a theory that needs more evidence to support it. Further efforts aimed at exploring the clinical value of metabolic reprogramming in sepsis are necessary in the future.
Abbreviations
OXPHOS, Oxidative phosphorylation; MODS, Multiple organ dysfunction syndrome; PDH, Pyruvate dehydrogenase; PDK, Pyruvate dehydrogenase kinase; TAC, Tricarboxylic acid cycle; LDH, Lactate dehydrogenase; MAP, Mean arterial pressure, HR, Heart rate, CVP, Central venous pressure; RASS, Richmond Agitation-Sedation Scale; SOFA, Sequential Organ Failure Assessment; APACHE II score, Acute Physiology and Chronic Health Evaluation II score, NE, Norepinephrine, P(V-A)CO2, Central venous-to-arterial carbon dioxide difference; ScvO2, Central venous oxygen saturation; OI, Oxygenation index; HB, Hemoglobin; PCT, Procalcitonin; WBC, White blood cell; TNF-α, Tumor Necrosis Factor α; IL-10, Interleukin-10; IL-6, Interleukin-6; ROC curve, Receiver operating characteristic curve; AUC, The area under receiver operating characteristic curve; ICU, The intensive care unit; PUMCH, Peking Union Medical College Hospital.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article. The datasets generated or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
All procedures performed in the present study were in accordance with the Declaration of Helsinki and the study was reviewed and approved by Peking Union Medical College Hospital (PUMCH) institutional review board (approval number JS-3302). Informed consent to participate in the study was obtained from the next of kin of each patient.
Acknowledgments
We thank all patients for their understanding and cooperation during this study and their contributions to sepsis research. We thank Rongping Chen, Department of Critical Care Medicine, Peking Union Medical College Hospital, Peking Union Medical College, Chinese Academy of Medical Sciences, for assistance with data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Beijing Municipal Science & Technology Commission (No. Z201100005520038), Beijing natural Science Foundation (7232126) and National High Level Hospital Clinical Research Funding [2022-PUMCH-A-218]for the financial support.
Disclosure
The authors declared that they have no competing interests.
References
1. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
2. Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):775–787. doi:10.1001/jama.2016.0289
3. Van Der Poll T, Shankar-Hari M, Wiersinga WJ. The immunology of sepsis. Immunity. 2021;54(11):2450–2464. doi:10.1016/j.immuni.2021.10.012
4. Lan R, Geng H, Singha PK, et al. Mitochondrial pathology and glycolytic shift during proximal tubule atrophy after ischemic AKI. J Am Soc Nephrol. 2016;27(11):3356–3367. doi:10.1681/asn.2015020177
5. Liu J, Zhou G, Wang X, et al. Metabolic reprogramming consequences of sepsis: adaptations and contradictions. Cell Mol Life Sci. 2022;79(8):456. doi:10.1007/s00018-022-04490-0
6. Batista-Gonzalez A, Vidal R, Criollo A, et al. New insights on the role of lipid metabolism in the metabolic reprogramming of macrophages. Front Immunol. 2020:10. doi:10.3389/fimmu.2019.02993
7. Zhang W, Wang G, Xu ZG, et al. Lactate Is a natural suppressor of rlr signaling by targeting MAVS. Cell. 2019;178(1):176–189.e15. doi:10.1016/j.cell.2019.05.003
8. Zuo H, Wan Y. Metabolic reprogramming in mitochondria of myeloid cells. Cells. 2019;9(1). doi:10.3390/cells9010005
9. Zhang Y, Zhai Z, Duan J, et al. Lactate: the Mediator of Metabolism and Immunosuppression. Front Endocrinol. 2022:13. doi:10.3389/fendo.2022.901495
10. Gómez H, Kellum JA, Ronco C. Metabolic reprogramming and tolerance during sepsis-induced AKI. Nat Rev Nephrol. 2017;13(3):143–151. doi:10.1038/nrneph.2016.186
11. Stanzani G, Tidswell R, Singer M. Do critical care patients hibernate? Theoretical support for less is more. Intensive Care Med. 2020;46(3):495–497. doi:10.1007/s00134-019-05813-9
12. Mainali R, Zabalawi M, Long D, et al. Dichloroacetate reverses sepsis-induced hepatic metabolic dysfunction. Elife. 2021:10. doi:10.7554/eLife.64611
13. S OT, Zabalawi M, Jain S, et al. Dichloroacetate improves systemic energy balance and feeding behavior during sepsis. JCI Insight. 2022;7(12). doi:10.1172/jci.insight.153944
14. Mccall CE, Zabalawi M, Liu T, et al. Pyruvate dehydrogenase complex stimulation promotes immunometabolic homeostasis and sepsis survival. JCI Insight. 2018;3(15). doi:10.1172/jci.insight.99292
15. Krejčová G, Danielová A, Nedbalová P, et al. Drosophila macrophages switch to aerobic glycolysis to mount effective antibacterial defense. Elife. 2019:8. doi:10.7554/eLife.50414
16. Daifuku M, Nishi K, Okamoto T, et al. Activation of J774.1 murine macrophages by lactate dehydrogenase. Cytotechnology. 2014;66(6):937–943. doi:10.1007/s10616-013-9646-3
17. Faubert B, Solmonson A, Deberardinis RJ. Metabolic reprogramming and cancer progression. Science. 2020;368(6487). doi:10.1126/science.aaw5473
18. Biswas SK. Metabolic reprogramming of immune cells in cancer progression. Immunity. 2015;43(3):435–449. doi:10.1016/j.immuni.2015.09.001
19. Toro J, Manrique-Caballero CL, Gómez H. Metabolic reprogramming and host tolerance: a novel concept to understand sepsis-associated AKI. J Clin Med. 2021;10(18). doi:10.3390/jcm10184184
20. Cheng SC, Scicluna BP, Arts RJ, et al. Broad defects in the energy metabolism of leukocytes underlie immunoparalysis in sepsis. Nat Immunol. 2016;17(4):406–413. doi:10.1038/ni.3398
21. Zullo A, Guida R, Sciarrillo R, et al. Redox homeostasis in cardiovascular disease: the role of mitochondrial sirtuins. Front Endocrinol (Lausanne). 2022;13:858330. doi:10.3389/fendo.2022.858330
22. Li AE, Ito H, Rovira II, et al. A role for reactive oxygen species in endothelial cell anoikis. Circ Res. 1999;85(4):304–310. doi:10.1161/01.res.85.4.304
23. Nuzzo E, Berg KM, Andersen LW, et al. Pyruvate dehydrogenase activity is decreased in the peripheral blood mononuclear cells of patients with sepsis. a prospective observational trial. Ann Am Thorac Soc. 2015;12(11):1662–1666. doi:10.1513/AnnalsATS.201505-267BC
24. Zeng Z, Huang Q, Mao L, et al. The Pyruvate Dehydrogenase Complex in Sepsis: metabolic Regulation and Targeted Therapy. Front Nutr. 2021;8:783164. doi:10.3389/fnut.2021.783164
25. Zhu X, Long D, Zabalawi M, et al. Stimulating pyruvate dehydrogenase complex reduces itaconate levels and enhances TCA cycle anabolic bioenergetics in acutely inflamed monocytes. J Leukoc Biol. 2020;107(3):467–484. doi:10.1002/jlb.3a1119-236r
26. Mao L, Sun M, Chen Z, et al. The pyruvate dehydrogenase complex mitigates LPS-induced endothelial barrier dysfunction by metabolic regulation. Shock. 2022;57(6):308–317. doi:10.1097/shk.0000000000001931
27. L’her E, Sebert P. Effects of dichloroacetate and ubiquinone infusions on glycolysis activity and thermal sensitivity during sepsis. J Lab Clin Med. 2004;143(6):352–357. doi:10.1016/j.lab.2004.03.004
28. Bakalov V, Reyes-Uribe L, Deshpande R, et al. Dichloroacetate-induced metabolic reprogramming improves lifespan in a Drosophila model of surviving sepsis. PLoS One. 2020;15(11):e0241122. doi:10.1371/journal.pone.0241122
29. Ferreira BL, Leite GGF, Brunialti MKC, et al. HIF-1α and hypoxia responsive genes are differentially expressed in leukocytes from survivors and non-survivors patients during clinical sepsis. Shock. 2021;56(1):80–91. doi:10.1097/shk.0000000000001694
30. Liberti MV, Locasale JW. Histone lactylation: a new role for glucose metabolism. Trends Biochem Sci. 2020;45(3):179–182. doi:10.1016/j.tibs.2019.12.004
31. Samuvel DJ, Sundararaj KP, Nareika A, et al. Lactate boosts TLR4 signaling and NF-kappaB pathway-mediated gene transcription in macrophages via monocarboxylate transporters and MD-2 up-regulation. J Immunol. 2009;182(4):2476–2484. doi:10.4049/jimmunol.0802059
32. Feng T, Zhao X, Gu P, et al. Adipocyte-derived lactate is a signalling metabolite that potentiates adipose macrophage inflammation via targeting PHD2. Nat Commun. 2022;13(1):5208. doi:10.1038/s41467-022-32871-3
33. Schneider DS, Ayres JS. Two ways to survive infection: what resistance and tolerance can teach us about treating infectious diseases. Nat Rev Immunol. 2008;8(11):889–895. doi:10.1038/nri2432
34. Brealey D, Brand M, Hargreaves I, et al. Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet. 2002;360(9328):219–223. doi:10.1016/s0140-6736(02)09459-x
35. Abraham E, Singer M. Mechanisms of sepsis-induced organ dysfunction. Crit Care Med. 2007;35(10):2408–2416. doi:10.1097/01.ccm.0000282072.56245.91
36. Fullerton JN, Singer M. Organ failure in the ICU: cellular alterations. Semin Respir Crit Care Med. 2011;32(5):581–586. doi:10.1055/s-0031-1287866
37. Singer M. The role of mitochondrial dysfunction in sepsis-induced multi-organ failure. Virulence. 2014;5(1):66–72. doi:10.4161/viru.26907
38. Japiassú AM, Santiago AP, D’avila JC, et al. Bioenergetic failure of human peripheral blood monocytes in patients with septic shock is mediated by reduced F1Fo adenosine-5’-triphosphate synthase activity. Crit Care Med. 2011;39(5):1056–1063. doi:10.1097/CCM.0b013e31820eda5c
39. Eyenga P, Rey B, Eyenga L, et al. Regulation of oxidative phosphorylation of liver mitochondria in sepsis. Cells. 2022;11(10). doi:10.3390/cells11101598
40. Cimolai MC, Alvarez S, Bode C, et al. Mitochondrial mechanisms in septic cardiomyopathy. Int J Mol Sci. 2015;16(8):17763–17778. doi:10.3390/ijms160817763
41. Biswas SK, Mantovani A. Orchestration of metabolism by macrophages. Cell Metab. 2012;15(4):432–437. doi:10.1016/j.cmet.2011.11.013
42. Yang L, Xie M, Yang M, et al. PKM2 regulates the Warburg effect and promotes HMGB1 release in sepsis. Nat Commun. 2014;5:4436. doi:10.1038/ncomms5436
43. Pool R, Gomez H, Kellum JA. Mechanisms of Organ Dysfunction in Sepsis. Crit Care Clin. 2018;34(1):63–80. doi:10.1016/j.ccc.2017.08.003
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Correlation and Prognostic Assessment of Low T3 Syndrome and Norepinephrine Dosage for Patients with Sepsis: A Retrospective Single-Center (Cohort) Study
Zhang J, Fu S, Liu F, Wan J, Wu S, Jiang G, Tao W, Zhou W, Qian K
International Journal of General Medicine 2022, 15:4837-4847
Published Date: 10 May 2022
Role of Procalcitonin in Predicting Mortality and Organ Dysfunction at Intensive Care Admission
Suranadi IW, Sinardja CD, Suryadi IA
International Journal of General Medicine 2022, 15:4917-4923
Published Date: 12 May 2022
Intravenous Fluid Bolus Rates Associated with Outcomes in Pediatric Sepsis: A Multi-Center Analysis
Mullan PC, Pruitt CM, Levasseur KA, Macias CG, Paul R, Depinet H, Nguyen ATH, Melendez E
Open Access Emergency Medicine 2022, 14:375-384
Published Date: 28 July 2022
Impaired Circulating Antibody-Secreting Cells Generation Predicts the Dismal Outcome in the Elderly Septic Shock Patients
Xu H, Li T, Zhang X, Li H, Lv D, Wang Y, Huo F, Bai J, Wang C
Journal of Inflammation Research 2022, 15:5293-5308
Published Date: 13 September 2022
Albumin Level is Associated with Short-Term and Long-Term Outcomes in Sepsis Patients Admitted in the ICU: A Large Public Database Retrospective Research
Cao Y, Su Y, Guo C, He L, Ding N
Clinical Epidemiology 2023, 15:263-273
Published Date: 3 March 2023