Back to Journals » Journal of Inflammation Research » Volume 18
Time to Occurrence of Incontinence-Associated Dermatitis: An Experimental Animal Study
Authors Duan J, Zhang Y, Yuan D, Wang X, Peng J, Wang J, Liang X, Xu C
Received 10 December 2024
Accepted for publication 29 March 2025
Published 14 April 2025 Volume 2025:18 Pages 5077—5086
DOI https://doi.org/10.2147/JIR.S511464
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ning Quan
Junfang Duan,1,* Yan Zhang,2,* Dajiang Yuan,3 Xiaoru Wang,1 Jian Peng,4 Junli Wang,1 Xiaojuan Liang,1 Chenli Xu1
1Department of Critical Care Medicine, The Second Hospital of Shanxi Medical University, Taiyuan, People’s Republic of China; 2General Surgery, The Second Hospital of Shanxi Medical University, Taiyuan, People’s Republic of China; 3Shanxi Cardiovascular Hospital, Taiyuan, 030024, People’s Republic of China; 4Anhui Institute of Pediatric Research, Anhui Provincial Children’s Hospital, Anhui, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chenli Xu, Department of Critical Care Medicine, Second Hospital of Shanxi Medical University, No. 382 of Wuyi Road, Xinghualing District, Taiyuan, 030001, People’s Republic of China, Tel +8619834513692, Email [email protected]
Objective: To establish an animal model of Incontinence-Associated Dermatitis (IAD) and investigate inflammatory factor changes to determine the time frame for IAD onset.
Methods: Twenty-eight male SPF mice were randomly assigned to four groups. Gauze soaked in synthetic fecal solution was applied to the dorsal and ear skin. Based on exposure duration, the groups were designated as the normal, 0.5h, 2h, and 4h groups. At the end of the experiment, IAD severity was assessed, and ear edge thickness was measured. Blood was collected via the eyeball, and IL-1α, IL-6, and TNF-α levels were measured using enzyme-linked immunosorbent assay. Hematoxylin and eosin staining of dorsal skin samples was performed to analyze early pathological changes.
Results: No moderate to severe IAD was observed in any group. However, ear edge thickness increased significantly after 0.5h. Mild inflammatory cell infiltration was noted in the 0.5h group, with more severe infiltration in the 2h and 4h groups. Inflammatory factor levels were higher in the 0.5h, 2h, and 4h groups than in the normal group.
Conclusion: The IAD model established using synthetic fecal exposure effectively facilitates mechanistic research. Skin tissue became loose and edematous, with a significant increase in inflammatory factors within 0.5h. These findings suggest that fecal contamination should be removed within 0.5h to prevent skin damage. Additionally, IL-1α, IL-6, and TNF-α are promising biomarkers for IAD-associated skin injury.
Keywords: animal model, Incontinence-associated dermatitis, synthetic feces, inflammatory cytokines
Introduction
Incontinence-Associated Dermatitis (IAD) is a major concern in hospitals, particularly in intensive care units (ICUs). The incidence of IAD in ICUs is as high as 64%,1–4 with a prevalence of up to 54%.5,6 It commonly affects the buttocks, perineum, perigenital region, groin, and inner thighs.7 IAD is characterized by maceration and erythema, causing discomfort such as itching and pain, which can prolong hospital stays and increase overall healthcare costs.8
IAD is associated with impaired skin barrier function.9 As a protective interface between the body and the external environment, the skin consists of the epidermis, dermis, and subcutis.10 The outermost layer of the epidermis, the stratum corneum (SC), plays a crucial role in barrier function. The SC, composed of corneocytes and a highly organized lipid matrix, forms a nearly impermeable barrier, except to water molecules.11 Skin maceration is the initial step in IAD development.12 Excessive moisture exposure causes overhydration, disrupts SC structure, increases permeability, and heightens sensitivity to irritants.13 Additionally, the role of digestive enzymes has to be considered. Digestive enzymes in feces, including lipases and proteases, penetrate the skin and compromise its barrier function.14 These enzymes also trigger cytokine release, further exacerbating skin damage and leading to erosion and denudation.15
In the current ICD-11 classification, IAD is recognized as a common form of irritant contact dermatitis (ICD) caused by prolonged skin exposure to urine or feces.16–18 However, histopathological findings suggest that IAD may not fully align with the characteristics of irritant dermatitis.12 Among the cytokines involved in inflammation, interleukin-1α (IL-1α),19 interleukin-6 (IL-6),20 and tumor necrosis factor-α (TNF-α)21 have been associated with ICD. Recent studies indicate that the release of IL-1α may be the initial trigger of the inflammatory cascade in ICD.22 IL-1α and TNF-α serve as primary alarm signals, further inducing the release of pro-inflammatory mediators.23,24 Additionally, IL-1α has been reported to upregulate IL-6 expression via MAPK and NF-κB signaling pathways.25–28 IL-6, produced by various immune and non-immune cells such as keratinocytes and fibroblasts, promotes keratinocyte proliferation and migration while enhancing fibroblast proliferation, playing a protective role in ICD development.29 Based on these findings, this study hypothesized that IL-1α, TNF-α, and IL-6 contribute to the pathogenesis of IAD.
Although pancreatin solution has been used to establish IAD animal models,30 limitations include the absence of hematoxylin-eosin staining at experimental sites, prolonged exposure times, and discrepancies between pancreatin solution and actual fecal composition, potentially affecting results. Thus, a feasible and reliable animal model remains lacking, complicating the identification of pathogenic factors and therapeutic targets.
Mice are the most commonly used animal experimental model, especially in studies of physiology, biochemistry31–34 and immunology.35 Moreover, there are the same layers of cells in the epidermis and dermis between human and murine skin.36
In this study, synthetic feces were used to induce IAD in an animal model. By assessing changes in IL-1α, TNF-α, and IL-6 levels, we aimed to determine the time threshold for IAD development.
Materials and Methods
Preparation of Synthetic Feces
To simulate the effects of fecal incontinence, synthetic feces (pH 9.0) were prepared based on previous studies.15,31 The formulation included digestive enzymes such as trypsin, chymotrypsin, lipase, and bile salts in phosphate-buffered saline (PBS). The chemical composition of the synthetic feces is summarized in Table 1.
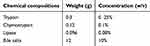 |
Table 1 Chemical Composition and Concentration of the Constituents for Synthetic Feces |
Ethics
All experimental procedures complied with the 8th edition of the US National Research Council’s Guide for the Care and Use of Laboratory Animals and were approved by the Ethics Committee of the Second Hospital of Shanxi Medical University (Approval Number: 2021017).
Animal
A total of 28 male SPF mice, approximately 7 weeks old, were selected and housed individually in the local animal facility for at least 7 days for acclimatization. The dorsal skin of all mice was intact, without erythema or edema. Animals were maintained under standardized 12-hour light-dark cycles at room temperature (23°C ± 2°C, 50% ± 10% humidity) with free access to food and water.
Construction of an IAD Model Animal Treatment
To construct the IAD model, the 28 mice were randomly assigned to one of four groups (n=7 in each) based on the duration of synthetic fecal exposure: (1) Normal group: No exposure to synthetic feces; only hair removal was performed. (2) 0.5h group: Exposed to synthetic feces for 30 minutes. (3) 2h group: Exposed to synthetic feces for 2 hours. (4) 4h group: Exposed to synthetic feces for 4 hours. Mice were anesthetized with an intraperitoneal injection of urethane solution (0.1 mL/10 g). Hair was removed from a 3×3 cm area of the dorsal skin, located 2 cm from the head. The skin was cleansed with sodium chloride solution and allowed to dry. Gauze blocks (3 × 3 cm) soaked with an equal volume of synthetic fecal solution were applied to the back skin. Additionally, a 1×1 cm gauze patch containing the same solution was placed on the ear skin to assess edema severity.
Assessment of the IAD Model
According to expert consensus, IAD classification is assessed based on the degree and severity of skin damage using the following criteria: Level 0 (No IAD): Intact skin without erythema. Level 1 (Mild IAD): Intact skin with erythema or edema. Level 2 (Moderate to Severe IAD): Skin exhibiting redness, swelling, damage, edema, blisters, erosion, or infection. Photographs of the affected skin were submitted to dermatologists for assessment and classification.
In this study, ear rim thickness was measured using a vernier caliper to evaluate the degree of skin edema in mice. Measurements were taken before and after treatment by laboratory personnel blinded to the experimental conditions. Three repeated measurements were recorded at the same anatomical location.
Enzyme Linked Immunosorbent Assay (ELISA)
Whole blood samples (0.8–1 mL) were collected from each mouse via enucleation of the eyeball. The samples were left to stand at 4°C for 40 minutes, then centrifuged to separate the supernatant, which was stored at −80°C for further analysis. ELISA was performed to quantify the expression of L-1α, IL-6, and TNF-α. Antibody kits were obtained from Boster Biological Technology (USA). Measurements were conducted using a microplate reader at a wavelength of 450 nm, with repeated detection for accuracy.
Histopathology Analysis
Mice were immediately euthanized by cervical dislocation in conjunction following blood collection. The skin tissue of the back of mice was taken for pathological observation at the same time. Tissues was fixed in 4% paraformaldehyde solution (BL539A, Biosharp, China) and maintained for 24 hours. Subsequently, the specimen was dehydrated, underwent paraffin embedding and sectioning. The sections were stained with hematoxylin and eosin (H&E) and sealed with neutral gum. Histomorphological changes were examined under a microscope, and the staining results were reviewed by professional pathologists for diagnosis.
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics 25.0 (IBM Corp). The normality of the data was assessed using the Shapiro–Wilk test. Data were expressed as mean ± standard error of the mean (SE). Paired t-tests were used to compare ear thickness before and after the experiment. One-way analysis of variance (ANOVA) was conducted to compare multiple groups, followed by post hoc multiple comparison tests. A P-value of <0.05 was considered statistically significant.
Results
Visual Observation Results
The study results indicated that in the 0.5h group, the skin at the exposed site remained intact, with no visible erythema, suggesting that IAD did not occur. In contrast, in the 2h and 4h groups, the skin remained intact but exhibited marked redness, indicating the presence of mild IAD. These findings are illustrated in Figure 1.
Pathological Results
Pathological changes in skin tissue were compared across different time points. The results revealed significant differences among the groups. In the 0.5h group, the interstitial tissue appeared noticeably loose and edematous, with scattered infiltration of a small number of inflammatory cells. In the 2h and 4h groups, the inflammatory response was more pronounced in the dermis, and interstitial edema persisted. The predominant inflammatory cells were lymphocytes and plasma cells. These findings are shown in Figure 2.
 |
Figure 2 Representative Images of Hematoxylin-Eosin Stained Histological Sections. (magnification: ×10). |
Comparison of the Degree of Skin Edema
In this study, the degree of edema in the exposed skin was indirectly assessed by measuring changes in the ear margin thickness of the mice. Paired t-test results showed a significant difference in ear margin thickness before and after the experiment, with thickness significantly higher post-experiment. (t left ear=−6.872, P<0.05; t right ear=−6.224, p<0.05). This indicates that the skin of the mice showed significant edema after stimulation.
ANOVA results revealed significant differences among the four groups (P < 0.05). After exposure, ear thickness increased and remained relatively stable after 2 hours, as shown in Table 2. Further analysis indicated a significant difference between baseline and 0.5-hour exposure (P < 0.05), but no significant differences between 0.5-hour and 2-hour exposure (P > 0.05) (Figure 3).
 |
Table 2 Change Trend of Ear Rim Thickness After the Experiment (Mm) |
Change Trend of Inflammatory Factors
To investigate the involvement of inflammatory factors in the process of IAD and their changing trends, IL-1α, IL-6, and TNF-α levels were measured in both normal and synthetic feces-irritated mice. Analysis of variance revealed significant differences in the levels of IL-1α, IL-6, and TNF-α between groups (Table 3). Inflammatory factor levels were compared at each time point. IL-1α, IL-6, and TNF-α levels significantly increased at both the half-hour and baseline time points (p<0.05). The trends of IL-1α, IL-6, and TNF-α over time differed after half an hour of intervention. IL-1α levels began to decrease after half an hour and remained significantly higher than baseline after 2 hours (P<0.05). IL-6 levels showed a downward trend after half an hour, while TNF-α levels began to decline after two hours. No statistically significant difference was observed in TNF-α and IL-6 levels between the four-hour and baseline time points (Figure 4).
 |
Table 3 Change Trend of IL-1α,IL-6 and TNF-α (pg/Ml) |
Discussion
In this study, synthetic feces were used to stimulate the back skin of mice, resulting in skin redness, edema, inflammatory cell infiltration, and the release of inflammatory factors, which are pathophysiological characteristics of IAD.32
The “Incontinence-Associated Dermatitis: Moving Prevention Forward” report, formed by the global IAD expert panel, clearly highlights the need for further research into the pathophysiological mechanisms of IAD.33 Therefore, constructing a suitable IAD animal model is essential for exploring skin damage and the inflammatory response, as well as determining the onset of IAD, which will provide a basis for understanding its pathogenesis and prevention.34
Building on previous studies,15,30,37–39 this research determined that trypsin, lipase, chymotrypsin, and bile salts were the main stimulants used to construct the IAD animal model after several pre-experiments. It has been reported that trypsin and lipase are risk factors for skin erythema and barrier damage.35 Notably, trypsin facilitates the dissolution of the stratum corneum and enhances the transdermal penetration of macromolecules, leading to internal tissue damage.36,37 On the other hand, lipids are crucial for maintaining skin barrier function.40 However, lipids can be digested by lipase, resulting in skin barrier impairment and exacerbating skin maceration.14,31 Additionally, bile salts further promote protease-induced skin irritation.31 Simultaneously, the pH of the solution was adjusted to 9. The alkaline nature of this irritant can disrupt the skin’s natural acidity, impairing barrier homeostasis and making the skin more susceptible to injury from external substances and mechanical forces.41,42 Likewise, digestive enzymes can damage the skin’s acid mantle, further compromising its integrity.12,38 Thus, the skin barrier is severely disrupted by the combined effects of alkaline enzyme solutions.31
Disruption of the skin barrier function may lead to increased penetration of other chemicals exposed to the skin, which can further cause skin edema.39 Therefore, edema is a common manifestation of IAD. The study evaluated the degree of skin edema in mice by measuring ear thickness. Increased skin thickness is typically indicative of edema formation and swelling within the dermis, often serving as the first hallmark of local inflammation.43 The results showed that the skin of mice stimulated by synthetic feces exhibited edema, with the degree of edema worsening as the stimulation time increased.
Although mild IAD was observed at two hours, inflammatory cell infiltration and tissue edema occurred after just half an hour. Based on these findings, it is recommended that nursing staff initiate treatment promptly to prevent further progression of IAD. This interpretation also provides a foundation for future research into the pathophysiological mechanisms of IAD.
Studies have shown that the pathological mechanism of IAD is related to the release of cytokines.30 However, changes in inflammatory factor levels over time have not been fully accounted for. Traditionally, IL-1 family cytokines mediate inflammation.44 IL-1α and TNF-α act synergistically,23 and their release triggers further proinflammatory cytokine production.24 It has also been reported that IL-1α regulates the release of IL-6.25–28 Cytokines, in turn, activate resident skin cells, which recruit neutrophils and lymphocytes to aggregate at the site of tissue damage,45,46 leading to inflammation, including redness, edema, and infiltration of inflammatory cells. Neutrophils also release proinflammatory cytokines IL-1α, IL-6, and TNF-α, which perpetuate this cycle and exacerbate the occurrence of IAD. Results from blood samples showed a significant increase in inflammatory factor levels compared to baseline values after exposure to synthetic feces for half an hour. However, a downward trend was observed after this time. This supports the time correlation between the onset of IAD and inflammatory factor levels. At 4 hours, mean levels of IL-1αand TNF-αremained above baseline levels, indicating that these inflammatory factors persisted for 4 hours. This finding is of clinical importance and highlights that interventions minimizing prolonged skin exposure to incontinence are critical for preventing IAD. In contrast, the mean levels of IL-6 continued to decrease after 2 hours of exposure and were not statistically different from baseline levels at 4 hours. The study by Sofoklis Koudounas15 showed that IL-6 levels began to decrease after 90 minutes, which is consistent with our findings.
Interestingly, the levels of IL-1α, IL-6, and TNF-α were significantly higher, yet pathological images showed only a small amount of inflammatory cell infiltration in the tissue after half an hour of fecal stimulation. This suggests that the body may inevitably experience immune dysregulation when skin tissue encounters feces. Activation of the immune system, including the epidermal barrier, immune cells, and cytokines, is thought to occur primarily. The innate immune system serves as the first line of defense against tissue injury.47 Immune factors and cells are rapidly activated and released upon encountering a stimulus.48,49 Additionally, the skin, as an immune organ, contains a complex network of immune cells within its tissue.50 The skin’s function is to initiate an inflammatory response following injury by utilizing epidermal and dermal components. This response includes the release of inflammatory cytokines and the recruitment of inflammatory cells.19,51 This raises an important clinical question: IL-1α, IL-6, and TNF-α may be predictors of IAD development.
Based on the above results, inflammatory cell infiltration and a significant increase in inflammatory factor release occurred at half an hour. However, mild IAD was observed on the skin only after 2 hours.
Limitations and Perspectives for Future Research
This study did not observe severe IAD in the skin of mice, but only noticeable redness and edema. Moreover, the picture was not clear enough. Inflammatory factors in the skin tissue of mice were not verified. Future experimental designs should focus on exploring cellular pathways involved in IAD, using cells as a breakthrough point. This approach may provide more accurate and scientific references for the clinical development of IAD prevention measures.
Conclusion
In summary, we developed a reproducible animal model for IAD induced by synthetic feces. This model can be used to study the pathogenesis of IAD and guide the development of novel interventions and nursing products. The study suggests that feces should be cleaned within half an hour to prevent IAD. Delayed cleaning beyond half an hour increases the risk of IAD, highlighting the importance of early detection by clinical nursing staff to reduce inflammatory responses and IAD incidence. Additionally, the study indicates that the occurrence of IAD is associated with the release of IL-1α, IL-6, and TNF-α, which may serve as promising biomarkers for identifying skin damage and understanding the pathogenesis of IAD, warranting further investigation. Furthermore, the destruction of the skin barrier is implicated in the development of IAD, providing new insights for its prevention.
Ethics Approval
This study was conducted with approval from the Ethics Committee of Second Hospital of Shanxi Medical University (No.: 2021017).
Funding
This study was awarded the Second Hospital of Shanxi Medical University Hospital Fund (No.:202204-5), Science and Technology Innovation Project of college in Shanxi Province (No.:2023L067).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Campbell J, Cook J-L, Doubrovsky A, Vann A, McNamara G, Coyer F. Exploring incontinence-associated dermatitis in a single center intensive care unit: a longitudinal point prevalence survey. J Wound Ostomy Continence Nurs. 2019;46(5):401–407. doi:10.1097/WON.0000000000000571
2. Wei L, Bao Y, Chai Q, Zheng J, Xu W. Determining risk factors to develop a predictive model of incontinence-associated dermatitis among critically Ill patients with fecal incontinence: a prospective, quantitative study. Wound Management & Prevention. 2019;65(4):24–33.
3. Johansen E, Lind R, Sjøbø B, Petosic A. Moisture associated skin damage (MASD) in intensive care patients: a Norwegian point-prevalence study. Intensive and Critical Care Nursing. 2020;60:102889. doi:10.1016/j.iccn.2020.102889
4. Del Cotillo-Fuente M, Valls-Matarín J, Sandalinas-Mulero I. Efficacy of a comprehensive strategy to reduce moisture-associated skin damage in an intensive care unit: a quasi-experimental study. Intensive and Critical Care Nursing. 2021;63:102964. doi:10.1016/j.iccn.2020.102964
5. Gray M, Giuliano KK. Incontinence-associated dermatitis, characteristics and relationship to pressure injury: a multisite epidemiologic analysis. Journal of Wound, Ostomy & Continence Nursing. 2018;45(1):63–67. doi:10.1097/WON.0000000000000390
6. Yüceler Kaçmaz H, Kaplan Ö, Kaplan A, Şahin MG, Cetinkaya A, Avci A. Incontinence-associated dermatitis: prevalence in intensive care units and knowledge, attitudes, and practices of nurses. J Nurs Care Qual. 2023;38(4):354–360. doi:10.1097/NCQ.0000000000000707
7. Campbell JL, Coyer FM, Osborne SR. Incontinence-associated dermatitis: a cross-sectional prevalence study in the Australian acute care hospital setting. Int Wound J. 2016;13(3):403–411. doi:10.1111/iwj.12322
8. Kayser SA, Koloms K, Murray A, Khawar W, Gray M. Incontinence and incontinence-associated dermatitis in acute care: a retrospective analysis of total cost of care and patient outcomes from the premier healthcare database. J Wound Ostomy Continence Nurs. 2021;48(6):545–552. doi:10.1097/WON.0000000000000818
9. Beele H, Smet S, Van Damme N, Beeckman D. Incontinence-associated dermatitis: pathogenesis, contributing factors, prevention and management options. Drugs & Aging. 2018;35(1):1–10. doi:10.1007/s40266-017-0507-1
10. Elias PM, Friend DS. The permeability barrier in mammalian epidermis. The Journal of Cell Biology. 1975;65(1):180–191. doi:10.1083/jcb.65.1.180
11. Volksdorf T, Heilmann J, Eming SA, et al. Tight junction proteins claudin-1 and occludin are important for cutaneous wound healing. The American Journal of Pathology. 2017;187(6):1301–1312. doi:10.1016/j.ajpath.2017.02.006
12. Mugita Y, Minematsu T, Huang L, et al. Histopathology of incontinence-associated skin lesions: inner tissue damage due to invasion of proteolytic enzymes and bacteria in macerated rat skin. PLoS One. 2015;10(9):e0138117. doi:10.1371/journal.pone.0138117
13. Pather P, Doubrovsky A, Jack L, Coyer F. Incontinence-associated dermatitis: who is affected? J Wound Care. 2021;30(4):261–267. doi:10.12968/jowc.2021.30.4.261
14. Mugita Y, Minematsu T, Nakagami G, Sanada H. Influence of digestive enzymes on development of incontinence-associated dermatitis: inner tissue damage and skin barrier impairment caused by lipidolytic enzymes and proteases in rat macerated skin. Int Wound J. 2018;15(4):623–632. doi:10.1111/iwj.12906
15. Koudounas S, Bader DL, Voegeli D. Investigating the release of inflammatory cytokines in a human model of incontinence-associated dermatitis. J Tissue Viability. 2021;30(3):427–433. doi:10.1016/j.jtv.2021.06.005
16. Acton C, Ivins N, Bainbridge P, Browning P. Management of incontinence-associated dermatitis patients using a skin protectant in acute care: a case series. J Wound Care. 2020;29(1):18–26. doi:10.12968/jowc.2020.29.1.18
17. Deprez J, Ohde N, Eilegård Wallin A, et al. Prognostic factors for the development of incontinence-associated dermatitis (IAD): a systematic review. Int Wound J. 2024;21(7):e14962. doi:10.1111/iwj.14962
18. International classification of diseases for mortality and morbidity statistic. 2018. Available from: https://icd.who.int/browse11/l-m/en.
19. Calhoun KN, Luckett-Chastain LR, Frempah B, Gallucci RM. Associations between immune phenotype and inflammation in murine models of irritant contact dermatitis. Toxicological Sciences: an Official Journal of the Society of Toxicology. 2019;168(1):179–189. doi:10.1093/toxsci/kfy289
20. Luckett-Chastain LR, Gipson JR, Gillaspy AF, Gallucci RM. Transcriptional profiling of irritant contact dermatitis (ICD) in a mouse model identifies specific patterns of gene expression and immune-regulation. Toxicology. 2018;410:1–9. doi:10.1016/j.tox.2018.08.014
21. Carreras-Badosa G, Maslovskaja J, Periyasamy K, et al. NickFect type of cell-penetrating peptides present enhanced efficiency for microRNA-146a delivery into dendritic cells and during skin inflammation. Biomaterials. 2020;262:120316. doi:10.1016/j.biomaterials.2020.120316
22. Lee HY, Stieger M, Yawalkar N, Kakeda M. Cytokines and chemokines in irritant contact dermatitis. Mediators Inflamm. 2013;2013:916497. doi:10.1155/2013/916497
23. Spiekstra SW, Toebak MJ, Sampat‐Sardjoepersad S, et al. Induction of cytokine (interleukin-1α and tumor necrosis factor-α) and chemokine (CCL20, CCL27, and CXCL8) alarm signals after allergen and irritant exposure. Exp Dermatol. 2005;14(2):109–116. doi:10.1111/j.0906-6705.2005.00226.x
24. Hertiš Petek T, Petek M, Petek T, Marčun Varda N. Emerging links between microbiome composition and skin immunology in diaper dermatitis: a narrative review. Children (Basel). 2022;9(1). doi:10.3390/children9010112
25. Dinarello CA. Immunological and inflammatory functions of the interleukin-1 family. Annu Rev Immunol. 2009;27(1):519–550. doi:10.1146/annurev.immunol.021908.132612
26. Sims JE, Smith DE. The IL-1 family: regulators of immunity. Nat Rev Immunol. 2010;10(2):89–102. doi:10.1038/nri2691
27. Joosten LAB, Netea MG, Dinarello CA. Interleukin-1β in innate inflammation, autophagy and immunity. Semin Immunol. 2013;25(6):416–424. doi:10.1016/j.smim.2013.10.018
28. Yang M, Wang X, Wang L, Wang X, Li J, Yang Z. IL-1α up-regulates IL-6 expression in bovine granulosa cells via MAPKs and NF-κB signaling pathways. Cell Physiol Biochem. 2017;41(1):265–273. doi:10.1159/000456091
29. Frempah B, Luckett-Chastain LR, Gallucci RM. IL-6 negatively regulates IL-22R α expression on epidermal keratinocytes: implications for irritant contact dermatitis. J Immunol Res. 2019;2019:6276254. doi:10.1155/2019/6276254
30. Wen Z, Zhu W, Liu Q, Zhang H, Mei B, Shen M. Development of an animal model for inducing various degrees of severity of incontinence-associated dermatitis. Journal of Wound, Ostomy & Continence Nursing. 2017;44(6):578–582. doi:10.1097/WON.0000000000000370
31. Andersen PH, Bucher AP, Saeed I, Lee PC, Davis JA, Maibach HI. Faecal enzymes: in vivo human skin irritation. Contact Dermatitis. 1994;30(3):152–158. doi:10.1111/j.1600-0536.1994.tb00696.x
32. Dissemond J, Assenheimer B, Gerber V, et al. Moisture-associated skin damage (MASD): a best practice recommendation from Wund-D.A.CH. J Dtsch Dermatol Ges. 2021;19(6):815–825.
33. Proceedings of the Global IAD Expert Panel. Incontinence-associated dermatitis: moving prevention forward.
34. Glass GF Jr, Goh CCK, Cheong RQ, Ong ZL, Khong PCB, Chan E-Y. Effectiveness of skin cleanser and protectant regimen on incontinence-associated dermatitis outcomes in acute care patients: a cluster randomised trial. Int Wound J. 2021;18(6):862–873. doi:10.1111/iwj.13588
35. Berg RW, Buckingham KW, Stewart RL. Etiologic factors in diaper dermatitis: the role of urine. Pediatr Dermatol. 1986;3(2):102–106. doi:10.1111/j.1525-1470.1986.tb00498.x
36. Li Y-Z, Quan Y-S, Zang L, et al. Transdermal delivery of insulin using trypsin as a biochemical enhancer. Biol Pharm Bull. 2008;31(8):1574–1579. doi:10.1248/bpb.31.1574
37. Li Y-Z, Quan Y-S, Zang L, et al. Trypsin as a novel potential absorption enhancer for improving the transdermal delivery of macromolecules. J Pharm Pharmacol. 2009;61(8):1005–1012. doi:10.1211/jpp.61.08.0003
38. Basketter DA, English JS, Wakelin SH, White IR. Enzymes, detergents and skin: facts and fantasies. The British Journal of Dermatology. 2008;158(6):1177–1181. doi:10.1111/j.1365-2133.2008.08561.x
39. Kanikkannan N, Burton S, Patel R, Jackson T, Shaik MS, Singh M. Percutaneous permeation and skin irritation of JP-8+100 jet fuel in a porcine model. Toxicol Lett. 2001;119(2):133–142. doi:10.1016/S0378-4274(00)00311-8
40. Jost PC, Griffith OH, Capaldi RA, Vanderkooi G. Evidence for boundary lipid in membranes. Proc Natl Acad Sci U S A. 1973;70(2):480–484. doi:10.1073/pnas.70.2.480
41. Koudounas S, Bader DL, Voegeli D. Elevated skin pH is associated with an increased permeability to synthetic urine. Journal of Wound, Ostomy & Continence Nursing. 2021;48(1):61–67. doi:10.1097/WON.0000000000000716
42. Baker P, Huang C, Radi R, Moll SB, Jules E, Arbiser JL. Skin Barrier Function: the Interplay of Physical, Chemical, and Immunologic Properties. Cells. 2023;12(23):2745. doi:10.3390/cells12232745
43. Camponogara C, Casoti R, Brusco I, et al. Tabernaemontana catharinensis leaves effectively reduce the irritant contact dermatitis by glucocorticoid receptor-dependent pathway in mice. Biomedicine & Pharmacotherapy = Biomedecine & Pharmacotherapie. 2019;109:646–657. doi:10.1016/j.biopha.2018.10.132
44. Berger A. Science commentary: th1 and Th2 responses: what are they? BMJ (Clinical Research Ed). 2000;321(7258):424. doi:10.1136/bmj.321.7258.424
45. Gittler JK, Krueger JG, Guttman-Yassky E. Atopic dermatitis results in intrinsic barrier and immune abnormalities: implications for contact dermatitis. The Journal of Allergy and Clinical Immunology. 2013;131(2):300–313. doi:10.1016/j.jaci.2012.06.048
46. Tian H, Matsuo Y, Fukunaga A, Ono R, Nishigori C, Yodoi J. Thioredoxin ameliorates cutaneous inflammation by regulating the epithelial production and release of pro-inflammatory cytokines. Frontiers in Immunology. 2013;4:269. doi:10.3389/fimmu.2013.00269
47. Hillion S, Arleevskaya MI, Blanco P, et al. The innate part of the adaptive immune system. Clinical Reviews in Allergy & Immunology. 2020;58(2):151–154. doi:10.1007/s12016-019-08740-1
48. Yatim KM, Lakkis FG. A brief journey through the immune system. Clinical Journal of the American Society of Nephrology: CJASN. 2015;10(7):1274–1281. doi:10.2215/CJN.10031014
49. Hato T, Dagher PC. How the innate immune system senses trouble and causes trouble. Clinical Journal of the American Society of Nephrology: CJASN. 2015;10(8):1459–1469. doi:10.2215/CJN.04680514
50. Nguyen AV, Soulika AM. The dynamics of the skin’s immune system. International Journal of Molecular Sciences. 2019;20(8). doi:10.3390/ijms20081811
51. Sierawska O, Małkowska P, Taskin C, et al. Innate immune system response to burn damage-focus on cytokine alteration. International Journal of Molecular Sciences. 2022;23(2):716. doi:10.3390/ijms23020716
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




