Back to Journals » Clinical Ophthalmology » Volume 18
Validation of Clinical Protocol of Astigmatism Induction in Pseudophakic Patients
Authors De Melo Jnr IR, Hida WT , Moscovici BK , Vilar C, Motta AFP, de Medeiros AL, Chaves MAPD , Lake JC, Nose W, Carricondo PC
Received 8 April 2024
Accepted for publication 16 October 2024
Published 21 November 2024 Volume 2024:18 Pages 3375—3387
DOI https://doi.org/10.2147/OPTH.S472752
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Irineu Ribeiro De Melo Jnr,1 Wilson Takashi Hida,1– 3 Bernardo Kaplan Moscovici,4,5 Cesar Vilar,1,2 Antonio Francisco Pimenta Motta,1 Andre Lins de Medeiros,1 Mario Augusto Pereira Dias Chaves,1 Jonathan Clive Lake,1 Walton Nose,4 Pedro Carlos Carricondo3
1Department of Ophthalmology, Hospital Oftalmológico De Brasília, Brasília, DF, Brazil; 2Department of Ophthalmology, Renato Ambrosio Eye Research Center, Brasília, DF, Brazil; 3Department of Ophthalmology, University of Sao Paulo, São Paulo, SP, Brazil; 4Department of Ophthalmology, Federal University of Sao Paulo UNIFESP, São Paulo, SP, Brazil; 5Department of Ophthalmology, Hospital Visão Laser, Santos, SP, Brazil
Correspondence: Bernardo Kaplan Moscovici, Email [email protected]
Purpose: Validate a novel approach for assessing residual astigmatism’s impact on visual acuity in pseudophakic patients using defocus curves and spherical equivalent compensation.
Materials and Methods: Thirteen patients over 40 with cataracts and normal ophthalmological examinations were enrolled in a prospective, non-randomized cohort study. The defocus curve method was employed, wherein visual acuity was measured with spherical lenses ranging from − 2.50 to +2.50 diopters in 0.5 diopter increments based on subjective refraction. Cylindrical lenses (+1, +2, and +3 diopters) were introduced at each spherical diopter’s 90° and 180° axes. Curves’ results were compared at each defocus point to assess the impact of astigmatism. The Kruskal–Wallis test was used to determine if astigmatism significantly affected visual acuity post-phacoemulsification surgery with intraocular lens implantation.
Results: Significant p-values were observed only for defocus curve points of − 0.5, 0, +0.5, and +1, indicating rejection of the hypothesis of no difference between the 90° and 180° groups at these points. Although statistical significance was not achieved, the against-the-rule (ATR) group was inclined toward improved near and intermediate visual acuity. In contrast, the with-the-rule (WTR) group tended to enhance distance visual acuity and myopic tolerance.
Conclusion: This novel methodology is both reproducible and valuable. It offers potential insight into residual astigmatism tolerance in pseudophakic patients. Its application may aid in surgical planning and intraocular lens decision-making.
Keywords: cataract, astigmatism, visual acuity, treatment result
Introduction
Astigmatism assessment and treatment at the time of cataract surgery can impact both objective and subjective outcomes. Toric intraocular lenses are the most common technology used in this manner. However, even with modern corneal pre-operative analysis (eg Placido topography, Scheimpflug tomography, multi-spot central reflectometry), residual refractive astigmatism still poses a challenge in many patients. A recent meta-analysis showed that residual astigmatism of 0.50 diopters or less varied from 45% to 85% of cases. This range of outcomes is likely influenced by factors such as tear film abnormalities, corneal high-order aberrations and IOL tilt — elements that are not entirely within the surgeon’s control. Therefore, IOLs that ensure optimal visual quality, even with some remaining astigmatism, are desirable.1–13
Residual astigmatism poses a significant challenge in achieving optimal visual outcomes with intraocular lenses (IOLs). Defocus curves have become an invaluable tool for assessing the performance of presbyopia-correcting IOLs across multiple focal points, providing insights into how astigmatism impacts visual acuity at various distances. This methodology is particularly beneficial for evaluating cases where residual astigmatism persists after surgery, allowing for informed decisions regarding the need for further correction.
Modern cataract surgery aims to both restore vision by replacing the opaque lens and achieve precise refractive outcomes. With the introduction of toric lenses and arcuate incisions, it is crucial to have a method to assess tolerance to residual astigmatism. This evaluation helps guide decisions on whether to perform additional procedures or leave small amounts of residual against-the-rule (ATR) or with-the-rule (WTR) astigmatism, depending on the patient’s specific needs.
This study aims to validate a new methodology for evaluating the impact of residual astigmatism in pseudophakic patients. It employs the astigmatic defocus curve with spherical equivalent compensation.
Materials and Methods
This prospective and non-randomized cohort study included thirteen patients older than 40 with a normal ophthalmological examination besides senile cataracts. Although the study was non-randomized, all procedures were standardized and performed under identical conditions to minimize bias, and the defocus curve was performed by the same surgeon for all patients. It was conducted within the Department of Cataract at the Hospital Oftalmológico de Brasilia (HOB). Before surgery, written informed consent was secured from all patients, and the study received approval from ethics committee of HOB – Hospital Oftalmologico de Brasilia (approval code: 42915320.3.0000.5667).
All procedures adhered rigorously to the ethical standards the responsible human experimentation committee set forth and followed the principles outlined in the Helsinki Declaration.
Preoperative Evaluation and Patient Selection
Patients were recruited for this study from only one site between September 2018 and December 2018.
We allowed a two-minute interval between each lens measurement to avoid carryover effects and ensure that responses were independent of previous lens trials.
Inclusion Criteria
Patients who underwent bilateral phacoemulsification surgery with a monofocal lens implant (Sensar AR40, Johnson & Johnson, News Brunswick, USA) with residual refractive astigmatism of less than 0.50D in both eyes.
Exclusion Criteria
Patients with a history of ocular surgery, central endothelial cell count <2000 cells/mm2, glaucoma with intraocular pressure >21 mmHg, amblyopia, retinal abnormalities, ongoing steroid or immunosuppressive treatment, connective tissue diseases, or those who had experienced complicated cataract surgery, such as posterior capsule rupture, vitreous loss, or incorrect positioning of the IOL within the capsular bag, as well as individuals with irregular astigmatism or keratoconus, were excluded. Residual refractive astigmatism of more than 0.50D after PHACO.
Study Lens
(Sensar AR40, Johnson & Johnson, News Brunswick, USA).
Preoperative Evaluation
All patients underwent a comprehensive ophthalmological examination, including auxiliary examinations such as IOL Master 700 (Zeiss, Germany), OPD Scan (NIDEK, Japan), and Pentacam (Oculus, Germany).
Surgical Procedures
All surgeries were consistently performed by the same skilled surgeon following established protocols. Phacoemulsification surgery was performed via a temporal clear corneal incision, and a foldable posterior chamber IOL was inserted into the capsular bag. The surgeries used the Centurion phacoemulsification device (Alcon, Texas, USA).
Defocus Curve
Only one eye per patient was included. Eye dominance was tested using the Dolman method, and the dominant eye was selected. Astigmatic defocus was induced over the manifest distance refraction with negative refractive cylinders (CYL) from −0.50 to −1.50 D in 0.50 D steps at two orientations of the axis (0 and 90 degrees) to induce against the rule astigmatism (ATR) and with the rule astigmatism (WTR) simple hyperopic astigmatism, respectively. The defocus curves were obtained in corrected distance visual acuity with the Early Treatment Diabetic Retinopathy Study (ETDRS) reading charts, at intervals of 0.50 spherical diopters from −3.00D to +2.00D associated with astigmatism induced (astigmatic defocus).
The spherical equivalent of the original refraction was respected for the defocus curve with cylindrical lenses. So, for each −0.50 added in cylindrical diopters, +0.25 was added in the spherical component.
No control group was included in this preliminary study. However, the defocus curve measurements were repeated twice for each patient, showing consistent results across repetitions and confirming the repeatability of our procedures.
Although this was a non-randomized study, all measurements were standardized and performed under identical conditions to minimize bias.
Statistical Analysis
Statistical analysis was performed using SPSS (Version 24.0 for Windows; IBM, Armonk, NY). The normality of the data distribution was assessed using the Kolmogorov–Smirnov test. Parametric analysis was conducted when applicable, utilizing Fisher’s exact test. The Kruskal–Wallis test assessed whether astigmatism significantly affected the quality of the patient’s visual acuity following phacoemulsification surgery with intraocular lens implantation. Subsequently, the Nemenyi test, a multiple comparison test for non-parametric data, was utilized to identify group differences.
The sample size of 13 patients was deemed adequate to detect a medium-to-large effect size (DZ = 0.66) with a significance level of 5% for a one-tailed test and a statistical power of 0.8 (type II error <20%). A sensitivity analysis was conducted using GPower 3.1VR software.
Results
The p-value results were statistically significant solely for the defocus curve points of −0.5, 0, +0.5, and +1. Therefore, at these particular points, we can reject the null hypothesis, suggesting no difference between the WTR and ATR groups (Table 1 and Figure 1).
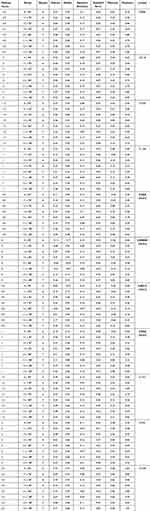 |
Table 1 Descriptive Statistics for Induced Astigmatism and Defocus Curves in WTR and ATR Astigmatism |
 |
Figure 1 Defocus Curves. |
Comparison of +1 × 90° and +1 × 180° (Table 2 and Figure 2)
At a −1.0 D vergence, a tendency toward better visual acuity was noted with +1 D ATR astigmatism induction compared to +1 D WTR astigmatism (p = 0.92).
 |
Table 2 Comparative Analysis of Defocus Curves in Relation to Induced ATR and WTR Astigmatism |
 |
Figure 2 Defocus Curves. |
At 0 D (p = 0.9608), +0.50 D (p = 0.8193), +1.00 D (p = 0.9197), −2.50 D (p = 0.98), and −2.00 D (p = 0.95) vergences, there was an inclination toward improved visual acuity for the WTR astigmatism group.
Comparison of +2 × 90° and +2 × 180° (Table 2 and Figure 2)
A tendency toward improved visual acuity was observed at −1.5 D (p = 0.98) and −1.0 D (p = 0.99) vergences with ATR astigmatism induction.
At 0 D (p = 0.9648), +0.50 D (p = 0.9502), +1.00 D (p = 0.9338), +1.50 D (p = 0.96), and +2.50 D (p = 0.95) vergences, there was a trend toward enhanced visual acuity for the WTR astigmatism group.
Comparison of +3 × 90° and +3 × 180° (Table 2 and Figure 2)
A trend toward improved visual acuity was observed at −2.50 D (p = 0.92) and −2.0 D (p = 0.93) vergences with ATR astigmatism induction.
At −0.50 D (p = 0.996), 0 D (p = 0.9972), +0.50 D (p = 0.9945), +1.00 D (p = 0.7831), and +1.50 D (p = 0.93) vergences, there was a trend toward enhanced visual acuity for the WTR astigmatism group.
No statistical significance was observed in any of these three comparisons. From the defocus graphs, it is evident that all groups reach a peak at point 0 of the defocus curve.
Discussion
Achieving spectacle independence is critical for patients undergoing premium intraocular lens (IOL) implantation. Post-implantation of presbyopia-correcting IOLs, refractive residual errors can compromise visual acuity, potentially leading to decreased patient satisfaction.14,15
In cases where corneal toricity is 0.75D or more, toric IOLs may be deemed necessary, given that 40% of cataract patients exhibit such levels of astigmatism. Understanding the astigmatic tolerance of IOLs is pivotal for surgical planning, as it plays a significant role in surgical outcomes. While the astigmatic tolerance limits for multifocal IOLs typically hover around 0.75D, recent research indicates that an extended depth of focus (EDOF) IOL exhibits a slightly higher tolerance of 1.00D compared to bifocal IOLs (0.75D) and trifocal IOLs (0.50D). Surgeons can leverage this information to tailor IOL selection based on the patient’s astigmatism levels, thereby minimizing the need for secondary interventions and enhancing overall patient satisfaction.16–28
A study by Sawusch and Guyton et al demonstrated that a small amount of myopic astigmatism can enhance the depth of focus in pseudophakic eyes, providing at least 20/30 visual acuity for both near and distant vision. The study concluded that the optimal amount of astigmatism to achieve maximum depth of focus is approximately 0.75D of the positive cylinder for each negative spherical component minus ATR 0.25 D, which is beneficial for near vision and the WTR favoring distance vision.29
In our current study, we validated a novel methodology using defocus curves to assess the impact of residual astigmatism on visual acuity in pseudophakic patients. The results showed that, although not achieving full statistical significance, there was a tendency towards improved near and intermediate visual acuity in the ATR group. In contrast, the WTR group exhibited better distance visual acuity and higher myopic tolerance. Therefore, our findings align with Sawusch and Guyton’s results, indicating that inducing residual astigmatism could improve the depth of focus.29
Residual astigmatism challenges the functional benefits of simultaneous focal points in multifocal IOLs, contributing to a higher retreatment rate in eyes implanted with such lenses. Even residual astigmatism as low as 0.50–0.75D has been demonstrated to negatively impact visual contrast and quality, emphasizing the importance of addressing astigmatism to enhance patient satisfaction.17–21
Alpins et al introduced a comprehensive vector analysis to quantify the effects of astigmatism correction, highlighting that off-axis astigmatic treatments result in reduced flattening and increased torque effects. Alpins demonstrated that as the deviation from the intended treatment axis increases, the efficacy of the astigmatic correction diminishes, a finding critical for understanding and predicting surgical outcomes. Both studies underscore the importance of precise alignment in astigmatic corrections. In our research, the defocus curve methodology provided insights into how specific astigmatism orientations affect visual acuity at different vergences, paralleling Alpins’ emphasis on the significant impact of off-axis treatments on the overall effectiveness of astigmatism correction. Integrating these insights into clinical practice can improve surgical planning and IOL selection, ultimately enhancing patient satisfaction by reducing residual astigmatism and optimizing visual outcomes.30–32
Our study observed that residual astigmatism impacts visual acuity in pseudophakic patients, with ATR astigmatism improving near and intermediate vision, while WTR astigmatism enhances distance vision. These findings align with Tognetto et al, who demonstrated the importance of accurate toric IOL alignment for optimal visual outcomes. Their study illustrated how misalignment of toric IOLs from the intended axis results in a progressive decline in image quality, as shown by the visual information fidelity (VIF) metric. A 5-degree rotation caused a 7.03% decay in VIF, while a 30-degree rotation led to a 45.85% reduction, indicating significant image quality deterioration with increased misalignment.30–32
Furthermore, Tognetto et al confirmed Alpins’ mathematical prediction that the loss of astigmatic correction is not linear but follows a sinusoidal relationship, with significant quality loss at higher degrees of misalignment. This matches our observations, particularly with Figure 2 in our study, which shows similar trends in visual acuity degradation when comparing ATR and WTR astigmatism at different defocus points. Thus, integrating these insights highlights the critical need for precise toric IOL placement to minimize residual astigmatism and enhance postoperative visual quality.30,31
This research introduces a novel methodology employing a defocus curve and distance visual acuity to assess the tolerance to optically induced astigmatism (compensated with spherical equivalent) in pseudophakic eyes. The validation of this approach serves as an additional tool for surgeons in evaluating the need for toric IOLs during pre-phacoemulsification assessments. Furthermore, it provides valuable insights for selecting the appropriate IOL, especially when corneal astigmatism measurements vary between diagnostic devices. The study findings offer significant information to both patients and surgeons regarding the outcomes associated with toric IOL implantation.20–22
Furthermore, utilizing an ATR cylindrical lens may alleviate the effects of WTR astigmatism induced by the eyelid, thereby improving visual performance. However, it is essential to acknowledge that this theoretical possibility necessitates further research and clinical trials to validate its efficacy.
A potential hypothesis for why WTR astigmatism might influence visual acuity differently from ATR astigmatism involves the natural changes in corneal curvature and the influence of eyelid pressure on the cornea. As people age, the cornea tends to flatten in the horizontal meridian and steepen in the vertical meridian, leading to a natural shift toward ATR astigmatism. Consequently, WTR astigmatism, aligning with the steeper vertical meridian, might focus light more effectively for distance vision, whereas ATR astigmatism could improve near and intermediate vision.
Hayashi et al’s research underscored the impact of residual astigmatism on both monofocal and multifocal IOLs, revealing that astigmatism exceeding 1D exacerbated vision impairment in bifocal IOLs and 0.75D in trifocal IOLs. Before implantation, prior comprehension of each IOL’s response to residual astigmatism is pivotal.1–3,24–28
Pérez-Sanz et al studied astigmatism tolerance, comparing monofocal and EDOF IOLs through in vitro measurements. Their findings highlighted superior visual acuity outcomes with ATR astigmatism in both types of lenses, emphasizing the significance of considering astigmatism type in IOL selection.1–3
While near and intermediate acuities were not directly measured, the trends were inferred from the defocus curve, which allowed us to assess visual performance across various focal points.
Despite the study’s contributions, limitations, such as a small sample size, underscore the need for further research to validate and expand upon these findings. Although this study involved only 13 eyes, which limits the statistical power, the results indicate trends that warrant further exploration. Future studies with larger sample sizes and more information will be essential to confirm these trends and enhance the generalizability of the findings. In conclusion, the proposed methodology proves reproducible and valuable, offering insights into predicting residual astigmatism tolerance in pseudophakic patients. This information can aid surgery planning and facilitate informed decision-making regarding IOL selection.
Although not statistically significant, the ATR group also tended to enhance near and intermediate visual acuity. In contrast, the WTR group trended toward improved distance visual acuity and myopic tolerance.
Overall, this new methodology proves reproducible and beneficial and may assist in predicting residual astigmatism tolerance in pseudophakic patients, thereby aiding in surgery planning and IOL decision-making.
Abbreviations
ATR, Against-the-rule; IOL, Intraocular lenses; OMS, Organizacion Mundial de la Salud; WTR, With-the-rule.
Ethics Approval and Informed Consent
Prior to surgical procedures, written consent was obtained from all patients, and ethical approval was granted by the local ethics committee (approval code: 93694918.0.0000.5667). The study strictly adhered to the ethical guidelines established by the responsible human experimentation committee and followed the principles outlined in the Helsinki Declaration.
Acknowledgments
This paper’s abstract was orally presented at the 2019 American Society of Cataract and Refractive Surgery (ASCRS) ASOA annual meeting.
Disclosure
Prof. Dr. Jonathan Lake reports grants from Johnson & Johnson, during the conduct of the study. The authors declare no other conflict of interests in this work.
References
1. Hayashi K, Yoshida M, Igarashi C, Hirata A. Effect of refractive astigmatism on all-distance visual acuity in eyes with a trifocal intraocular lens. Am J Ophthalmol. 2021;221:279–286. doi:10.1016/j.ajo.2020.07.051
2. Wan KH, Au ACK, Kua WN, et al. Enhanced monofocal versus conventional monofocal intraocular lens in cataract surgery: a meta-analysis. J Refract Surg. 2022;38(8):538–546. doi:10.3928/1081597X-20220707-01
3. Pérez-Sanz L, Vega F, Azor-Morón JA, Cuellar F, Millán MS, Garzón N. Tolerance to residual astigmatism of an isofocal intraocular lens. Graefes Arch Clin Exp Ophthalmol. 2023. doi:10.1007/s00417-023-06305-9
4. Bourne RR, Dineen BP, Ali SM, Noorul Huq DM, Johnson GJ. Prevalence of refractive error in Bangladeshi adults: results of the national blindness and low vision survey of Bangladesh. Ophthalmology. 2004;111(6):1150–1160. doi:10.1016/j.ophtha.2003.09.046
5. Ventura LO, Barros EA, Arruda Junior JR. Sinais e sintomas das ametropias. In: Schor P, Uras R, Óptica VS, editors. Refração e Visão Subnormal. Rio de Janeiro: Cultura Médica; 2008:205–217.
6. Alves MR, Polati M, de Sousa F. Refratometria Ocular e a Arte da Prescrição Médica. Rio de Janeiro: Cultura Médica; 2009.
7. Rayes TR, Rayes GR, Eing F, Guimarães Neto HP, Marquardt FA, Rayes A. Prevalência do astigmatismo e distribuição de seu eixo em pacientes de um serviço oftalmológico privado [Prevalence of astigmatism and distribution of its axis in patients of a private ophthalmological service]. Rev Bras Oftalmol. 2007;66(6):369–375. Portuguese. doi:10.1590/S0034-72802007000600002
8. Gills JP. Treating astigmatism at the time of cataract surgery. Curr Opin Ophthalmol. 2002;13(1):2–6. doi:10.1097/00055735-200202000-00002
9. Rocha Rde C, Oechsler RA, Garcia de Carvalho R, Moreira H. Influence of corneal astigmatism in final visual acuity after implantation of AcrySof ReSTOR: case report. Arq Bras Oftalmol. 2007;70(6):1040–1042. doi:10.1590/S0004-27492007000600031
10. Silva EFE, Trindade FC. Correção do astigmatismo na cirurgia da catarata [Correction of astigmatism in cataract surgery]. Arq Bras Oftalmol. 2007;70(4):609–614. Portuguese. doi:10.1590/S0004-27492007000400010
11. Sanders DR, Schneider D, Martin R, et al. Toric implantable collamer lens for moderate to high myopic astigmatism. Ophthalmology. 2007;114(1):54–61. doi:10.1016/j.ophtha.2006.08.049
12. Correia RJB, Moreira H, Netto SUL, Pantaleão GR. Performance visual após implante de LIO tórica em pacientes com astigmatismo corneano [Visual performance after toric IOL implantation in patients with corneal astigmatism]. Arq Bras Oftalmol. 2009;72(5):636–640. Portuguese. doi:10.1590/S0004-27492009000500007
13. Dick HB, Alió J, Bianchetti M, et al. Toric phakic intraocular lens: European multicenter study. Ophthalmology. 2003;110(1):150–162. doi:10.1016/S0161-6420(02)01447-1
14. Nichamin LD. Astigmatism management for modern phaco surgery. Int Ophthalmol Clin. 2003;43(3):53–63. doi:10.1097/00004397-200343030-00006
15. Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, González-Méijome JM, Cerviño A. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35(1):70–75. doi:10.1016/j.jcrs.2008.09.027
16. Braga-Mele R, Chang D, Dewey S, et al. Multifocal intraocular lenses: relative indications and contraindications for implantation. J Cataract Refract Surg. 2014;40(2):313–322. doi:10.1016/j.jcrs.2013.12.011
17. Ang RE. Comparison of tolerance to induced astigmatism in pseudophakic eyes implanted with small aperture, trifocal, or monofocal intraocular lenses. Clin Ophthalmol. 2019;13:905–911. doi:10.2147/OPTH.S208651
18. de Vries NE, Webers CAB, Touwslager WRH, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859–865. doi:10.1016/j.jcrs.2010.11.032
19. Ravalico G, Parentin F, Baccara F. Effect of astigmatism on multifocal intraocular lenses. J Cataract Refract Surg. 1999;25(6):804–807. doi:10.1016/S0886-3350(99)00029-2
20. Gundersen KG, Makari S, Ostenstad S, Potvin R. Retreatments after multifocal intraocular lens implantation: an analysis. Clin Ophthalmol. 2016;10:365–371. doi:10.2147/OPTH.S100840
21. Richdale K, Berntsen DA, Mack CJ, Merchea MM, Barr JT. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optom Vis Sci. 2007;84(10):969–975. doi:10.1097/OPX.0b013e318157c6dc
22. Lehmann RP, Houtman DM. Visual performance in cataract patients with low levels of postoperative astigmatism: full correction versus spherical equivalent correction. Clin Ophthalmol. 2012;6:333–338. doi:10.2147/OPTH.S28241
23. Rhim JW, Eom Y, Park SY, Kang SY, Song JS, Kim HM. Eyelid squinting improves near vision in against-the-rule and distance vision in with-the-rule astigmatism in pseudophakic eyes: an eye model experimental study. BMC Ophthalmol. 2020;20(1):4. doi:10.1186/s12886-019-1297-5
24. Hayashi K, Manabe S, Yoshida M, Hayashi H. Effect of astigmatism on visual acuity in eyes with a diffractive multifocal intraocular lens. J Cataract Refract Surg. 2010;36(8):1323–1329. doi:10.1016/j.jcrs.2010.02.016
25. Breyer DRH, Beckers L, Ax T, Kaymak H, Klabe K, Kretz FTA. Aktuelle übersicht: multifokale linsen und extended-depth-of-focus-intraokularlinsen [Current review: multifocal intraocular lenses and extended depth of focus intraocular lenses. Klin Monbl Augenheilkd. 2020; Vol. 2378:943–957. German
26. Niazi S, Gatzioufas Z, Dhubhghaill SN, et al. Association of patient satisfaction with cataract grading in five types of multifocal IOLs. Adv Ther. 2024;41(1):231–245. doi:10.1007/s12325-023-02698-5
27. Galvis V, Escaf LC, Escaf LJ, et al. Visual and satisfaction results with implantation of the trifocal Panoptix® intraocular lens in cataract surgery. J Optom. 2022;15(3):219–227. doi:10.1016/j.optom.2021.05.002
28. Karam M, Alkhowaiter N, Alkhabbaz A, et al. Extended depth of Focus versus trifocal for intraocular lens implantation: an updated systematic review and meta-analysis. Am J Ophthalmol. 2023;251:52–70. doi:10.1016/j.ajo.2023.01.024
29. Sawusch MR, Guyton DL. Optimal astigmatism to enhance depth of focus after cataract surgery. Ophthalmology. 1991;98(7):1025–1029. doi:10.1016/S0161-6420(91)32182-1
30. Tognetto D, Perrotta AA, Bauci F, et al. Quality of images with toric intraocular lenses. J Cataract Refract Surg. 2018;44(3):376–381. doi:10.1016/j.jcrs.2017.10.053
31. Alpins NA. Vector analysis of astigmatism changes by flattening, steepening, and torque. J Cataract Refract Surg. 1997;23(10):1503–1514. doi:10.1016/S0886-3350(97)80021-1
32. Villegas EA, Alcón E, Artal P. Minimum amount of astigmatism that should be corrected. J Cataract Refract Surg. 2014;40(1):13–19. doi:10.1016/j.jcrs.2013.09.010
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

