Back to Journals » Clinical Ophthalmology » Volume 18
Visual, Refractive, Functional, and Patient Satisfaction Outcomes After Implantation of a New Extended Depth-of-Focus Intraocular Lens
Authors Ferrando Gil J, Churruca Irazola A, Reparaz I, Lauzirika G , Martínez-Soroa I, Mendicute J
Received 21 October 2024
Accepted for publication 6 December 2024
Published 17 December 2024 Volume 2024:18 Pages 3801—3813
DOI https://doi.org/10.2147/OPTH.S499911
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Javier Ferrando Gil,1 Adela Churruca Irazola,1 Iraia Reparaz,1 Gorka Lauzirika,2,3 Itziar Martínez-Soroa,1,2 Javier Mendicute1,2
1Department of Ophthalmology, Donostia University Hospital, Donostia-San Sebastián, Spain; 2Miranza Begitek, Donostia-San Sebastián, Spain; 3R&D Department, Miranza Group, Donostia-San Sebastián, Spain
Correspondence: Gorka Lauzirika, Miranza Begitek, Calcutta Square No. 7, Donostia-San Sebastián, Spain, Email [email protected]
Purpose: To describe the visual, refractive, functional, and patient satisfaction outcomes of the Bi-Flex POB-MA 877PEY (Elon®, Medicontur Medical Engineering Ltd. Zsámbék, Hungary) extended depth-of-focus intraocular lens (EDoF IOL).
Patients and Methods: This was a prospective longitudinal descriptive study. Patients who underwent cataract surgery with the implantation of Bi-Flex POB-MA 877PEY IOL were included. Monocular refractive outcomes and visual acuity at distance, intermediate, and near were evaluated 1- and 3-month post-op. Binocular contrast sensitivity (CSV-1000, VectorVision, USA), binocular defocus curve, and patient satisfaction with the Visual Functioning Questionnaire (VFQ) were assessed at 3-month post-op.
Results: 20 Bi-Flex POB-MA 877PEY IOL were implanted bilaterally in 10 patients. The mean age of the patients was 68.60± 4.45 years. At 1-month post-op the monocular Corrected Distance Visual Acuity (CDVA), intermediate (CIVA) and near (CNVA) was 0.02± 0.03, 0.29± 0.08, and 0.40± 0.05 LogMAR respectively. At 3-month post-op the CDVA decrease to 0.05± 0.06 LogMAR (p=0.042), and CIVA and CNVA remained stable at 3-month post-op (p> 0.05). No statistical differences were found in post-op spherical equivalent at 1 and 3 month (− 0.03± 0.19 D and − 0.03± 0.13 D; p=1.000). 100% of eyes were within ± 0.5 D at 1 month and 3-month post-op. Binocular defocus curve shows a peak of maximum visual acuity (VA) at 0 D (0.00± 0.04 LogMAR), and a constant and progressive decrease at − 1.50 D, and − 2.50 D (0.15± 0.08 LogMAR and 0.33± 0.10 LogMAR, respectively). Contrast sensitivity decreased at high spatial frequencies. In patient satisfaction at 3 months post-op, VFQ reveals that 90% of patients revealed no or minor difficulty with glare/flare and 100% of patients have no or minor difficulty with halos. In overall satisfaction, 80% of patients rate their vision between 8 and 9 from a scale from 0 to 10.
Conclusion: The Bi-Flex POB-MA 877PEY EDoF IOL provides good visual outcomes for distance, and adequate intermediate vision, with low visual disturbances.
Keywords: cataract surgery, phacoemulsification, EDoF IOL
Introduction
Cataracts are one of the leading causes of vision impairment globally.1 As people age, the prevalence of age-related cataracts steadily increases.2 Cataract surgery, a common procedure involving the implantation of intraocular lenses (IOLs), is highly regarded for its ability to significantly improve visual acuity, thereby enhancing everyday activities, emotional well-being, and social interactions.3
Intraocular lenses come in various optical designs tailored to provide patients with independence from glasses after surgery. Monofocal IOLs primarily improve distance vision but require glasses for near and intermediate distances. On the other hand, multifocal IOLs offer clear vision at multiple distances but can sometimes cause visual disturbances such as halos and glare, which may lead to discomfort or dissatisfaction.4,5
The latest innovation in IOL technology is the extended depth-of-focus (EDoF) lenses. Unlike traditional lenses, EDoF lenses create an extended focal range along the optical axis, enhancing the lens’s depth of focus. These lenses aim to strike a balance between monofocal and multifocal IOLs by improving visual clarity at intermediate distances regarding monofocal IOLs while potentially reducing the incidence and severity of visual disturbances and improving contrast sensitivity if we compare them with most current multifocal IOLs. There are also innovative designs aimed at improving the focal range of monofocal IOLs, such as those that manipulate asphericity. These designs often feature a spherical posterior surface and a higher-order aspheric anterior surface, which create a gradual increase in optical power from the periphery to the center of the lens, thereby enhancing depth of focus without compromising visual comfort.6
EDoF technology can be achieved through various approaches such as diffractive optics, pinhole designs, bioanalogic approaches, and incorporating spherical aberration.7,8 However, recently a new multifocality modality has been developed using Wavefront Linking technology in Bi-Flex POB-MA 877PEY EDoF IOL.9 This is a non-diffractive optical design composed of a series of central concentric refractive zones with varying curvature that are linked by specially designed linking zones, resulting in light energy being distributed continuously along the optical axis. The focal points are linked together, resulting in a single elongated focus that is useful across the entire field of vision.
Although there is evidence in the literature on the results of the different EDoF IOLs, to this date, there is no report showing the results with Bi-Flex POB-MA 877PEY IOL. The aim of this study was to evaluate the visual, refractive and functional outcomes achieved with this new EDoF IOL.
Methods
Study Design
This was a prospective, observational, descriptive study in patients undergoing bilateral cataract surgery with implantation of the Bi-Flex POB-MA 877PEY (Elon®, Medicontur, Medical Engineering Ltd., Zsámbék, Hungary) EDoF IOL. The study was conducted between January 2023 and May 2023 in the Department of Ophthalmology of Hospital Universitario Donostia (HUD) in Donostia-San Sebastián (Spain). Patients were informed in detail about the aim of the study, and informed consent was obtained from all patients. The study was performed in accordance with the Helsinki Declaration, and the research ethics committee approval was obtained from HUD (PS2022040).
Patients
The study population comprised patients over 50 years old with bilateral cataracts. The cataracts were at least level 1 of the Lens Opacities Classification System (LOCS) III classification. Other inclusion criteria were patients with healthy retina and patients who required primary IOL surgery. These criteria ensured the safety and relevance of the study population for evaluating the investigational intraocular lens.
Exclusion criteria were patients with comorbidities or preoperative corneal astigmatism over 0.75 diopters (D) as well as amblyopia, age-related macular degeneration (AMD), congenital ocular anomalies, irregular astigmatism, and non-age-related cataracts. Additionally, patients with retinal or corneal diseases, glaucoma, severe myopia, or requiring iris manipulation were not included. Exclusions also applied to those with systemic diseases, legal restrictions, pregnancy, inability to consent, or inadequate fundus visualization. Patients using systemic medication causing ocular side effects or with a history of ocular trauma were also excluded.
Clinical Protocol
The preoperative examination included a comprehensive assessment to gather pertinent information. It began with a medical history review, encompassing patient background, treatments, and concurrent pathologies. Complete ophthalmic examinations were performed including uncorrected (UDVA) and corrected (CDVA) distance visual acuity, subjective refraction, Pentacam topography (Oculus Optikgeräte GmbH, Wetzlar, Germany), slit-lamp examination, intraocular pressure measurements with Goldman applanation tonometer (GAT), and dilated fundus examinations to guarantee that all inclusion criteria were satisfied and none of the exclusion criteria were met. After patient selection and prior to surgery, IOLMaster500® (Carl Zeiss Meditec, Germany) biometry was performed. IOL power was calculated using the SRK/T formula with an A-constant (manufacturer) of 118.9.
The study protocol included 3-month follow-up visits. All measurements were measured by an experienced optometrist. At the 1-month postoperative review, monocular and binocular uncorrected and corrected visual acuity at three distances (far 6 m, intermediate 66 cm, and near 40 cm) as well as subjective refraction were measured. At the 3-month follow-up, in addition to the same VA and refraction measurements as in the first month post-op, the binocular defocus curve (defocus from +2.00 to −4.50 D) and the binocular contrast sensitivity function (CSF) were measured. The CSV-1000 (Vector Vision, USA) device was used to measure the CSF under photopic (85 cd/m2) and glare conditions at 3-month post-op. The logarithmic values for 3, 6, 12, and 18 cycles per degree (cpd) were analyzed.
Besides clinical outcomes, vision-related quality of vision using the Visual Functioning Questionnaire (VFQ) test was used pre- and post-operatively. The questionnaire is divided into four sections. In the first section, the patients must respond about the difficulty performing the visual task through the question
How much difficulty have you got with glare, night vision, color perception, glare, depth perception, distorted near vision, distorted distance vision, blurred near vision, blurred far vision, and double vision?
being the answers 1-Not difficulty, 2-Minor difficulty, 3-Moderate difficulty, 4-Major difficulty, 5-Cannot accomplish, and 6-Not applicable. In the second section, the patients must respond about visual lifestyle through the question
How much difficulties have you got with (Watching TV or movies; Playing or working outdoors; Caring for / playing with children; Reading the time on an alarm clock; Seeing clearly when waking up; Reading the time on a wall clock; Performing your jobs / hobbies; Participating in sports / recreation; Participating in social events; Reading and near work activities; Driving at night; Driving when it is raining; Using a computer; Cooking; Shopping; Using a cell phone; Shaving or putting on make-up) due to your vision (without glasses or contact lenses)?
being the answers 1-Not difficulty, 2-Minor difficulty, 3-Moderate difficulty, 4-Major difficulty, 5-Cannot accomplish, and 6-Not applicable. In the third section, the patients must respond about If they use or not glasses through the question “How often do you use glasses or contact lenses?” being the answers 1- Always, 2-Almost always, 3-Time to time, 4-Very Rare, and 5-Never. Finally, in the fourth section, the patients must respond about overall satisfaction through the question “How much satisfied are you with your vision on a scale from 1 to 10?” being 1-At least, and 10- Maximum satisfaction.
Surgical Procedure
All surgeries were performed by a single experienced surgeon (JM). All patients underwent Femtosecond Laser-Assisted Cataract Surgery (FLACS) with VICTUSTM Femtosecond Laser Platform (Technolas, Bausch&Lomb Surgical, Munich, Germany) under topical anesthesia. 2.2 mm clear corneal temporal incisions were used since astigmatism was lower than 0.75 mm on all subjects. No sutures were used for incision sealing. The 5 mm capsulorhexis was centered in relation to the pupil in surgical mydriasis. After completion of phacoemulsification and polishing of the posterior capsule, the IOL was injected into the capsular bag. The viscoelastic material from behind the IOL was removed. The orientation of the haptics was vertical in all cases. At the end of the surgery, each patient was given intracameral cefuroxime. The second eye was operated between 2 days and 1 month after surgery on the first eye. Any potential adverse events were reviewed to ensure patient safety and assess the success of the surgical intervention.
Intraocular Lens
The Bi-Flex POB-MA 877PEY is a single piece, foldable aspheric hydrophobic acrylic IOL with UV blocker and blue light filter. This EDoF IOL incorporates Wavefront Linking technology and a series of central concentric refractive zones with varying curvatures connected by specially designed linking zones that provide +2.4 D of depth of focus extension. The outer diameter of the refractive zone has 2 mm diameter, and the inner diameter has 1.6 mm (Figure 1). This design is intended to improve vision at intermediate and near distances, featuring a patented 360° square edge (10 μm), posterior vaulting fenestrated C-loops with 0° angulation as haptic design, and a neutral aspheric optical design. The IOL has an overall diameter of 13 mm and an optic zone of 6 mm. The non-toric version of this IOL is available in spherical powers from +8.00 to +30.00 D in 0.50 D steps and from +31.00 to +35.00 D in 1 D steps. The IOL is available as part of a preloaded injector system.
 |
Figure 1 Optic design of the Bi-Flex POB-MA 877PEY IOL using Wavefront Linking technology. |
Statistical Analysis
The data was collected using a Microsoft Excel spreadsheet. Descriptive summaries of all relevant data were provided. The quantitative outcome measures were expressed in mean, standard deviation (SD), and range (max and min). The qualitative outcome measures were presented as the percentage of each category, with percentages generally based on the number of observation units with available data. The statistical analysis was done using SPSS software (version 22.0, SPSS Inc., Chicago, IL, USA). Normality was assessed using the Shapiro–Wilk test. When the quantitative variables were parametric, the t-student test was used; in non-parametric cases, the Wilcoxon test was used. Friedman exact test was used to evaluate the mean difference in VFQ test. A p-value of <0.05 was considered statistically significant.
Results
Demographics
20 Bi-Flex POB-MA 877PEY were implanted bilaterally in 10 patients. The mean age was 68.60 ± 4.45 years (range 77–63). Table 1 shows the preoperative biometric values. All the surgeries were uneventful, and we did not record any adverse events (glistening, posterior capsular opacification, early IOL-capsular bag complex dislocation, dysphotopyc phenomena, Irvine-Gass syndrome or endophthalmitis) in any patient along study visits.
 |
Table 1 Preoperative Biometric Values of Right Eye |
Visual and Refractive Outcomes
Ten right eyes of 10 patients were employed for visual and refractive analysis. Thus, in terms of monocular VA outcomes, the mean monocular Uncorrected Distance Visual Acuity (UCDVA) at 1-month (0.05 ± 0.09 LogMAR) and at 3-month (0.08 ± 0.10 LogMAR) was similar (p=0.115). Also, the monocular Best-Corrected Distance Visual Acuity (CDVA) at 1-month (0.02 ± 0.03 LogMAR) and at 3-month (0.05 ± 0.06 LogMAR) was similar (p=0.042) (Table 2).
 |
Table 2 Visual Acuity (LogMAR) During 3 Months of Follow-Up |
Regarding efficacy, the histogram of postoperative cumulative distribution of visual acuity reveal that 9 eyes (90%) achieved a monocular UDVA and CDVA equal to or greater than 20/25 LogMAR at 1-month post-op. The remaining cumulative distribution of VA at 1-month is presented in Figure 2 graphs. 3 eyes (30%) gained 1 line or more and the rest obtained the same difference in UDVA and CDVA (Figure 2, Graph B).
The predictability, in terms of intended post-op SE, the percentage of eyes in ± 0.50 D and ± 1.00 D were 100% (10 eyes) and 100% (10 eyes, respectively, at 1 month and 3-month post-op (Graph C of Figures 2 and 3). About 80% of eyes had a post-operative refractive cylinder ≤ −0.50 D at 1 month and 3 months. The remaining post-op refractive cylinder outcomes are presented in graph D and H in Figure 3. Thus, the stability of postoperative subjective refraction (sphere, cylinder and SE) remains stable (p=1.000) at 1 month and 3 months (Table 3).
 |
Table 3 Refractive results During 3 Months of Follow-Up |
Defocus Curve and Contrast Sensitivity Function
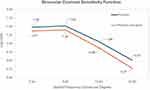
Figure 4 illustrates the binocular defocus curves (DF) at 3-month post-op. The binocular DF shows a peak of maximum VA at 0 D (0.00 ± 0.04 LogMAR) that corresponds to distance vision (6 m) and a constant and progressive decrease in VA at the intermediate (66 cm or −1.50 D) and near (40 cm or −2.50 D) distance (0.15 ± 0.08 LogMAR and 0.33 ± 0.10 LogMAR respectively).
 |
Figure 4 Binocular defocus curve given in LogMAR after implantation of a nondiffractive EDoF IOL (Bi-Flex POB-MA 877PEY) at 3 months postoperatively (n = 10 patients). |
Figure 5 shows the binocular contrast sensitivity function measured with CSV-1000 at 3-month. Regarding photopic conditions, at short spatial frequencies (3 and 6 cpg) a high and expected performance is evident (1.48 ± 0.26 Log Units and 1.52 ± 0.27 Log Units, respectively); however, at high spatial frequencies (12 and 18 cpg) a decrease (1.06 ± 0.24 Log Units and 0.51 ± 0.29 Log Units, respectively) were observed. In conditions with glare (Figure 5), the CSF decreases statistically in all spatial frequencies (A: 7.42%, p=0.040; B: 7.89%, p=0.022; C: 16.98%, p=0.000, and D: 47.06% p=0.014, respectively) compared with photopic conditions. The binocular contrast sensitivity in mesopic conditions (1.55 Log Units) at 1.5 cpg also decreased (1.37 Log Units) statistically significantly (p=0.100) when glare was applied.
Patient Satisfaction
Patient satisfaction was assessed with the VFQ test. The results for each question are expressed in % in four sub-tables (Supplemental Table 1) and in mean values in Figure 6. As it can be seen in Supplemental Table 1.1, regarding “How much difficulty have you got with each of the visual disturbances?” at 3-month post-op, 90% of the patients answered that they have no difficulty or minor difficulty with “glare”, “night vision”, “depth perception”, distorted near vision” and “blurred near vision”, and 100% of the patients had no difficulty or minor difficulty with “color perception” or “distorted far vision”. Regarding “How often do you use glasses or contact lenses?” (Supplemental Table 1.3), 70% of patients have answered that “never or very rarely need glasses or contact lenses” in far distance at 3-month post-op. In Figure 6C, for far distance, the difference in 1-month and 3-month post-op was statistically significant (3.10 ± 0.74 and 4.10 ± 0.88; p=0.016). However, no statistical differences were found in intermediate (2.80 ± 0.92 and 3.20 ± 1.03; p=0.313) and near (2.50 ± 0.97 and 3.00 ± 1.15; p=0.250) distance at 1- and 3-month post-op. In overall satisfaction (Supplemental Table 1.4), to the question “How much satisfied are you with your vision on a scale from 1 to 10?”, after the surgery at 3 months, 80% of patients rate their vision in a scale between 8 and 10, being 10 maximum satisfaction. The mean overall satisfaction (Figure 6D) at 1-month post-op was 6.00 ± 1.33 and at 3-month post-op was 7.90 ± 0.57, the difference being statistically significant (p=0.008).
 |
Figure 6 Mean values at 3-month post-op for the four sections (from A to D) of Visual Functioning Questionnaire (VFQ) test. |
Discussion
To the best of our knowledge, this is the first study to highlight the visual, refractive, and functional outcomes of Bi-Flex POB-MA 877PEY EDoF IOL in healthy eyes over a three-month period post-surgery.
In terms of visual acuity outcomes, at 3-month post-op we achieved values of monocular UDVA, UIVA, and UNVA of 0.08 ± 0.10, 0.26 ± 0.05, and 0.36 ± 0.07 LogMAR, respectively. These results are consistent with those reported by previous authors evaluating other refractive EDoF IOLs.10,11 Thus, Campos et al achieved a mean 3-month postoperative monocular UDVA, UIVA, and UNVA values of 0.10 ± 0.11 LogMAR, 0.21 ± 0.08 LogMAR, and 0.38 ± 0.14 LogMAR, respectively, with the LuxSmart refractive EDoF IOL. The same thing happened with Rabinovich's study where they found a UDVA at 3-month post-op of 0.07 ± 0.08 LogMAR with Lucidis refractive EDoF IOL. However, slight differences were found in UDVA and UNVA in the Iradier study with the implantation of Synthesis PLUS refractive EDoF IOL, being UDVA and UNVA of 0.11 ± 0.17 LogMAR and 0.14 ± 0.22 LogMAR, respectively.12 Therefore, the refractive EDoF IOL compared provided good distance and intermediate monocular and binocular (Table 4) visual outcomes.
 |
Table 4 Binocular UDVA, UIVA, UNVA and Spherical Equivalent at 3 Months Post-op on Patients Implanted with Comparable EDOF Lenses in the Literature |
As is known, other methods of expanding the depth-of-focus have been released, including the use of the pinhole effect, diffractive elements, and even wavefront-shaping designs.22 Our study evaluates the Bi-Flex POB-MA 877PEY EDoF IOL that has been designed by wavefront-linking technology. This has allowed us to achieve binocular distance-corrected visual acuities at 3-month post-op mean values of −0.01 ± 0.04 LogMAR, 0.19 ± 0.05 LogMAR, and 0.29 ± 0.05 LogMAR for CDVA, CIVA, and CNVA, respectively. Considering other wavefront-shaping design as Vivity IOL, Pantanelli et al found similar binocular CDVA −0.01 ± 0.10 LogMAR with Vivity EDoF IOL as in our study.13 However, Pantanelli et al found that DCIVA (−0.02 ± 0.13 LogMAR) and DCNVA (0.03 ± 0.12 LogMAR) values are even better than in the US registration trial.14 These results in intermediate and near distances are higher than could be expected for an EDoF IOL, but the fact that the Pantanelli study achieved better results than the US registration trial could be the difference in how the near testing was completed. However, T. Kohnen et al found the same binocular corrected VA results at three distances (−0.02 ± 0.068 LogMAR, 0.10 ± 0.08 LogMAR, and 0.29 ± 0.10 LogMAR for CDVA, DCIVA at 66cm and DCNVA at 40 cm, respectively) as in our study at 3-month post-op with Vivity EDoF IOL.15 Moreover, MA, Scheepers et al found that binocular DCVA and DCNVA at 40 cm were similar as in our results with Vivity (−0.03 ± 0.05 LogMAR and 0.22 ± 0.12 LogMAR respectively) and diffractive Symfony IOL (−0.03 ± 0.05 LogMAR and 0.26 ± 0.11 LogMAR respectively) EDoF IOL.16 Although we achieved similar results compared with other IOLs at 3-month post-op, our outcomes are also comparable with those achieved by de Medeiros et al with the diffractive Symfony IOL during long-term follow-up.17 In addition, our results indicate that both uncorrected and corrected distance visual acuity (UCDVA and CDVA) remained stable from the one-month to the three-month follow-up visits (p>0.05). These findings are consistent with other studies on EDoF lenses15,16 which have demonstrated that these lenses can provide a stable visual outcome without significant fluctuations over time.
One of the primary benefits observed with the Bi-Flex POB-MA 877PEY EDoF IOL was the high percentage of eyes achieving refractive stability in sphere, cylinder and SE through the period of follow-up (p > 1.000), with an accuracy of 100% of the cases within ±0.50 D and ±1.00 D of SE at both one and three months postoperatively. It seems to be a good approach to use the SRK/T formula targeting emmetropia and a Constant-A provided by the manufacturer when the AXL is in the normal range between 21.25 and 24.57mm as in our study. In terms of stability, there was not a trend to a more myopic residual refractive error over time as it has shown in other studies with other EDoF IOL.18,23 However, our refractive stability may be attributed to a stable IOL position within the capsular bag due to round and centered capsulorhexis facilitated by femtosecond laser. Thus, this degree of refractive accuracy and predictability is critical for ensuring patient satisfaction and reducing the need for additional corrective procedures, while other studies (Table 4) with nontoric version of EDoF IOLs achieved an accuracy of SE within ±0.50 D between 85–95%13,15,16 and 92–93% within ±1.00 D.19,20 These differences could be attributed to our study’s sample size, which results in a small amount of residual cylinder that has no effect on the SE mean. It is reasonable to expect that with a larger sample size, the percentage of patients within ±0.50D will decrease slightly.
The defocus curve analysis further supported the lens’s performance, showing optimal visual acuity at 0 D (0.00 ± 0.04 LogMAR) and a continuous range of vision between +0.50 D and −1.00 D with 0.10 LogMAR or better of visual acuity. This pattern is characteristic of EDoF lenses, which are designed to extend the range of clear vision while avoiding the sharp decline in acuity seen with traditional multifocal lenses. Also, it can see a gradual and smooth decline of visual acuity along intermediate (−1.50 D or 66 cm) and near (−2.50 D or 40 cm) distances that provide good functional vision. T. Khonen et al achieved 0.38 LogMAR of binocular visual acuity in −2.50 D defocus with Vivity IOL, very close to our results (0.33 ± 0.10 LogMAR) with Bi-Flex POB-MA 877PEY IOL.15
Concerning contrast sensitivity function measured with CSV-1000, performed under various conditions including glare, revealed satisfactory outcomes. Although there was a decrease in contrast sensitivity at higher spatial frequencies (12 and 18 cpg) under glare conditions, the overall performance is good. Theoretically, when positive spherical aberration of the cornea is compensated by negative spherical aberration of the IOL, the CSF could increase. In this sense, the Tecnis Symfony IOL has a negative spherical aberration value of −0.20 µm and is expected to reduce corneal positive spherical aberrations to almost zero. Thus, MO Sevik et al found in photopic conditions a mean value of CSF at 3, 6, and 12 cpg of 1.49 ± 0.15, 1.67 ± 0.13, and 1.38 ± 0.13 Log Units, respectively.21 At 3 cpg, the results were similar, but at 6 and 12 cpg they achieved better results. These differences could be due to negative spherical aberration of the Symfony IOL. Although it is not comparable, they also measured the CSF at 15 cpg, and they found 0.92 ± 0.17 Log Units compared with our study that we measured up to 18 cpg achieving 0.51 ± 0.29 Log Units. In glare conditions, their results were even better than in its non-glare conditions. This could be explained by achromatic technology to reduce chromatic aberrations. Even though the Bi-Flex POB-MA 877PEY IOL being neutral in spherical aberration, we believe that the results achieved in our study were comparable to M.O. Sevik, suggesting that the Bi-Flex POB-MA 877PEY IOL provides good visual quality even in challenging lighting situations due to its lack of spherical aberration, which is also less sensitive to decentration.
Patient-reported outcomes were measured with Visual Functioning Questionnaire (VFQ) test. Overall satisfaction increases from 1-month post-op to 3-month post-op, whereas the spectacle used in far, intermediate, and near distances as well as halos, glare, and night vision difficulties decreases. This is similar to the findings achieved with other EDoF IOL in earlier studies, which reported excellent levels of patient satisfaction.10,18,24 We speculate that our good refractive predictability with the Bi-Flex POB-MA 877PEY EDoF IOL might be the cause of this good patient satisfaction values. To support this explanation, it is known that patients with greater residual refractive error have more tendency to report dysphotopsia and be less satisfied with their overall visual quality.25,26 Although the questions related to near activities received the lowest scores, this pattern compared with trifocal IOLs is as could be expected.27
Regarding adverse events after surgery, no adverse events were reported throughout the study, underscoring the safety profile of Bi-Flex POB-MA 877PEY IOL. The absence of complications like posterior capsule opacification (PCO) or cystoid macular edema (CME) during the follow-up period reinforces the suitability of this lens for widespread clinical use.
This study has some limitations that should be noted. The first is the sample size; future studies with larger sample sizes, including patients with different anatomical characteristics, such as axial lengths and others, should be conducted to achieve more robust conclusions. Second, this is a non-comparative study, and therefore, an analysis of the possible superiority of this IOL compared with other EDoF IOLs should be performed. Third, several clinical measurements were not acquired, such as an investigation of the association between pupil size and possible corneal astigmatism changes after the surgery.
Conclusions
All in all, the Bi-Flex POB-MA 877PEY EDoF IOL demonstrates promising results in terms of visual acuity, refractive stability, and patient satisfaction. Its ability to provide good vision at multiple distances with minimal side effects makes it a valuable option for patients undergoing cataract surgery. Future studies should aim to evaluate long-term outcomes, and further comparative studies with other types of EDoF IOLs should be conducted to maximize the benefits of this advanced IOL technology.
Acknowledgments
The authors would like to thank all the staff of the ophthalmology department at HUD for their assistance in measuring and collecting the variables for this study.
Funding
This study was partially supported by a Medicontur grant (code: MEN-LIE-2022-01). The results of the study and the revision of the manuscript were conducted independently of any influence from Medicontur. Moreover, none of the authors have received payments from Medicontur for this study.
Disclosure
Javier Mendicute is a consultant for Alcon, and an external researcher for Bausch and Lomb, Santem, Hoya, and Medicontur. The remaining authors have nothing to declare.
The authors have no financial or proprietary interests in the medical field or products involved in this manuscript.
References
1. Flaxman SR, Bourne RRA, Resnikoff S, et al. Vision Loss Expert Group of the Global Burden of Disease Study. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(12):e1221–e1234. doi:10.1016/S2214-109X(17)30393-5
2. Hashemi H, Pakzad R, Yekta A, et al. Global and regional prevalence of age-related cataract: a comprehensive systematic review and meta-analysis. Eye. 2020;34(8):1357–1370. doi:10.1038/s41433-020-0806-3
3. Hecht I, Kanclerz P, Tuuminen R. Secondary outcomes of lens and cataract surgery: more than just “best-corrected visual acuity”. Prog Retin Eye Res. 2023;95:101150. doi:10.1016/j.preteyeres.2022.101150
4. Micheletti JM, Duncan NB, Hall B. Head-to-head comparison of intermediate vision of two monofocal intraocular lenses. Clin Ophthalmol. 2023;17:3983–3990. doi:10.2147/OPTH.S444696
5. Han KE, Lee JE. Comparative evaluation of visual performance and patient satisfaction following cataract surgery: a retrospective analysis of an extended depth-of-focus intraocular lens and a diffractive multifocal lens with extended depth of focus. J Clin Med. 2023;12(23):7368. doi:10.3390/jcm12237368
6. Goslings O, Veraart H, van de Laar-Muskens J, Piñero DP. Clinical outcomes with an aspheric monofocal and a new enhanced monofocal intraocular lens with modified optical profile. Graefes Arch Clin Exp Ophthalmol. 2023;261(8):2315–2326. doi:10.1007/s00417-023-06128-8
7. Ribeiro F, Dick HB, Kohnen T, et al. Evidence-based functional classification of simultaneous vision intraocular lenses: seeking a global consensus by the ESCRS Functional Vision Working Group. J Cataract Refract Surg. 2024;50(8):794–798. doi:10.1097/j.jcrs.0000000000001502
8. Kohnen T. Current and future nomenclature and categorization of intraocular lenses. J Cataract Refract Surg. 2024;50(8):787–788. doi:10.1097/j.jcrs.0000000000001510
9. ESCRS EuroTimes. 2022.
10. Campos N, Loureiro T, Rodrigues-Barros S, et al. Preliminary clinical outcomes of a new enhanced depth of focus intraocular lens. Clin Ophthalmol. 2021;15:4801–4807. doi:10.2147/OPTH.S344379
11. Rabinovich M, Ceresara G, Aramburu Del Boz A, Al Khatib D, Crespe M, Bovet J. Visual outcomes after implantation of lucidis EDOF IOL. J Ophthalmol. 2022;2022:5100861. doi:10.1155/2022/5100861
12. Iradier MT, Cruz V, Gentile N, Cedano P, Piñero DP. Clinical outcomes with a novel extended depth of focus presbyopia-correcting intraocular lens: pilot study. Clin Ophthalmol. 2021;15:1215–1221. doi:10.2147/OPTH.S297985
13. Pantanelli SM, O’Rourke T, Bolognia O, Scruggs K, Longenecker A, Lehman E. Vision and patient-reported outcomes with nondiffractive EDOF or neutral aspheric monofocal intraocular lenses. J Cataract Refract Surg. 2023;49(4):360–366. doi:10.1097/j.jcrs.0000000000001123
14. PMA P930014/S126: FDA summary of safety and effectiveness data. 2020.
15. Kohnen T, Petermann K, Böhm M, et al. Nondiffractive wavefront-shaping extended depth-of-focus intraocular lens: visual performance and patient-reported outcomes. J Cataract Refract Surg. 2022;48(2):144–150. doi:10.1097/j.jcrs.0000000000000826
16. Scheepers MA, Hall B. Randomized and double-blind comparison of clinical visual outcomes of 2 EDOF intraocular lenses. J Cataract Refract Surg. 2023;49(4):354–359. doi:10.1097/j.jcrs.0000000000001113
17. de Medeiros AL, Jones Saraiva F, Iguma CI, et al. Comparison of visual outcomes after bilateral implantation of two intraocular lenses with distinct diffractive optics. Clin Ophthalmol. 2019;13:1657–1663. doi:10.2147/OPTH.S202895
18. Campos N. Clinical outcomes and patient satisfaction of an enhanced depth of focus intraocular lens targeted for mini-monovision. Clin Ophthalmol. 2024;18:1607–1613. doi:10.2147/OPTH.S459868
19. Ruiz-Mesa R, Blanch-Ruiz J, Ruiz-Santos M, Montés-Micó R. Optical and visual quality assessment of an extended depth-of-focus intraocular lens based on spherical aberration of different sign. Int Ophthalmol. 2021;41(3):1019–1032. doi:10.1007/s10792-020-01659-z
20. Auffarth GU, Moraru O, Munteanu M, et al. European, multicenter, prospective, non-comparative clinical evaluation of an extended depth of focus intraocular lens. J Refract Surg. 2020;36(7):426–434. doi:10.3928/1081597X-20200603-01
21. Sevik MO, Akkaya Turhan S, Toker E. Clinical outcomes with a low add multifocal and an extended depth of focus intraocular lenses both implanted with mini-monovision. Eye. 2022;36(6):1168–1177. doi:10.1038/s41433-021-01600-3
22. Megiddo-Barnir E, Alió JL. Latest development in extended depth-of-focus intraocular lenses: an update. Asia Pac J Ophthalmol. 2023;12:58–79. doi:10.1097/APO.0000000000000590
23. Gawęcki M, Prądzyńska N, Kiciński K, Ratajczak A, Karska-Basta I, Grzybowski A. Patient reported outcomes after implementation of an enhanced depth of focus intraocular lens with low postoperative myopia. Adv Ophthalmol Pract Res. 2023;3:86–92. doi:10.1016/j.aopr.2023.02.003
24. Nowrouzi A, Del Barrio JL A, D’Oria F, Kamel NR, Alió JL. Visual performance after unilateral implantation of an extended depth-of-focus intraocular lens in patients with unilateral cataract. J Refract Surg. 2023;39:518–523. doi:10.3928/1081597X-20230710-01
25. de Vries NE, Webers CA, Touwslager WR, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;5:859–865. doi:10.1016/j.jcrs.2010.11.032
26. Woodward MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg. 2009;6:992–997. doi:10.1016/j.jcrs.2009.01.031
27. Tavassoli S, Ziaei H, Yadegarfar ME, et al. Trifocal versus extended depth of focus (EDOF) intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2024;7(7):CD014891. doi:10.1002/14651858.CD014891.pub2
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.