Back to Journals » Journal of Multidisciplinary Healthcare » Volume 18
Association Between Dietary Patterns and All-Cause Mortality in Individuals with Hypertension and Osteoporosis: A Retrospective Cohort Study
Authors Guan J, Ding L, Wang Y, Zhu Z, Pan M, Du L, Yin N
Received 22 January 2025
Accepted for publication 8 June 2025
Published 30 June 2025 Volume 2025:18 Pages 3781—3791
DOI https://doi.org/10.2147/JMDH.S518980
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Pavani Rangachari
Jianhua Guan,* Liang Ding,* Yifei Wang,* Zhongsheng Zhu,* Mingmang Pan, Li Du, Nuo Yin
Department of Orthopedics, Shanghai Jiao Tong University Affiliated Sixth People’s Hospital South Campus (Shanghai Fengxian District Central Hospital), Shanghai, 201599, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Nuo Yin, Department of Orthopedics, South Hospital of the Sixth People’s Hospital Affiliated to Shanghai University of Medicine & Health Sciences (Shanghai Fengxian District Central Hospital), No. 6600 South Fenggong Road Fengxian District, Shanghai, 201599, People’s Republic of China, Tel +86 18916174997, Email [email protected]
Objective: To explore the association of dietary patterns with all-cause mortality in individuals with hypertension and osteoporosis.
Methods: Data on individuals aged ≥ 20 years who completed bone mineral density tests were retrieved from the National Health and Nutrition Examination Survey database. Three dietary patterns were Mediterranean Diet Score (MeDS), Alternative Health Eating Index (AHEI) and Dietary Approaches to Stop Hypertension (DASH). The relationships between osteoporosis (OS), hypertension (HTN) and all-cause mortality were assessed by multivariate and univariate Cox proportional hazard models, with hazard ratios (HRs) and confidence intervals (CIs). Interaction of OS and HTN on overall mortality was evaluated by the attributable proportion (AP), relative excess risk due to interaction (RERI), and synergy index (S). Associations of three dietary patterns with all-cause mortality were explored in different groups, including adults with HTN or OS only, and adults with or without OS and HTN. Subgroups of gender and menopausal state were further evaluated these associations.
Results: Of the total 16,358 participants, 1383 (5.84%) died during the follow-up duration. Participants who had HTN (HR=1.272, 95% CI: 1.083– 1.494) or OS (HR=1.674, 95% CI: 1.262– 2.221) had a higher risk of overall mortality. There was an interaction between HTN and OS on overall mortality (RERI=0.677, 95% CI: 0.070– 1.285; AP=0.293, 95% CI: 0.094– 0.492; SI=2.070, 95% CI: 1.124– 3.813). The AHEI-2010, MeDS, and DASH were related to overall mortality in individuals with OS and HTN. The MeDS and DASH were concerned with all-cause mortality in HTN patients without OS. The MeDS and AHEI-2010 were linked to overall mortality in adults without OS and HTN.
Conclusion: The impacts of different dietary patterns were differences in multi-feature population. It was suggested that reasonable dietary management is beneficial to the prognosis of different populations.
Keywords: hypertension, osteoporosis, all-cause mortality, Mediterranean diet score, alternative health eating index (AHEI-2010), dietary approaches to stop hypertension
Introduction
Osteoporosis (OS), characterized by the deterioration of skeletal microarchitectue and loss of bone mass, can cause fracture.1 Nearly 53.6 million adults over the age of 50 had OS in the United States.2 Previous studies have found that non-gonadal hormone receptors in the osteoblast lineage cells, such as angiotensin II and adiponectin, directly modulate bone turnover and are implied in the etiology of metabolic syndrome, especially hypertension (HTN).3,4 Martinez reported that mortality due to non-communicable diseases increased from 57% of all-cause mortality in 1990 to 72.3% in 2016.5 It is necessary to carry out health management to improve the prognosis of patients with chronic diseases.
The role of other dietary factors in the onset of chronic diseases has been well established. Dietary indices are used to describe the total quality of the diet from current nutritional knowledge and/or dietary guidelines for disease control.6,7 The Mediterranean Diet Score (MeDS), Dietary Approaches to Stop Hypertension (DASH), and Alternative Health Eating Index (AHEI) are indices commonly used, as greater adherence is linked to a lower risk for chronic disease and death.8 Several studies have shown that specific dietary patterns such as Mediterranean Diet Score (MeDS), Alternative Health Eating Index (AHEI-2010) and Dietary Approaches to Stop Hypertension (DASH) can significantly affect health outcomes such as all-cause mortality, Osteoporosis (OS) and Hypertension (HTN).9–11In OS patients with HTN, which dietary pattern is more favorable for prognosis is uncertain.
Hypertension and osteoporosis are two common age-related diseases. In recent years, more and more evidence has shown that there is a certain biological association between these two diseases. Studies have shown that hypertension not only affects bone mineral density through the increase in sodium on calcium excretion but also affects bone metabolism through the increase in reactive oxygen species in blood vessels, cytokines, renin-angiotensin-aldosterone system and so on.12,13 High sodium diet, oxidative stress and inflammation are the main pathways by which hypertension affects the risk of osteoporosis. The increase in reactive oxygen species in blood vessels will also have a negative impact on bone metabolism, further exacerbating osteoporosis.14
Herein, we explored the interaction of OS and hypertension on the all-mortality, and further assessed the association between different dietary patterns (MeDS, AHEI-2010, and DASH) and all-cause mortality among multi-feature population, including adults with HTN or OS only, and adults with or without OS and HTN. Moreover, the associations were also evaluated based on the gender and menopausal state.
Materials and Methods
Study Design and Population
Data from the cohort study were retrieved retrospectively from the National Health and Nutrition Examination Survey (NHANES) database, an ongoing nationwide survey of the health and nutritional status of the non-institutionalized people in the United States.
A total of 41,209 subjects were collected. Of which, 18,308 subjects aged <20 years, 6,480 without bone mineral density (BMD) data, 23 without HTN information, and 40 without mortality information were excluded. Finally, 16,358 individuals were enrolled. Figure 1 shows the selection process.
 |
Figure 1 Flow chart of participant screening. |
Definition and Follow-up
OS was defined according to the World Health Organization (WHO) diagnostic criteria of BMD values greater than 2.5 standard deviation (SD) below the mean of young adult reference group. Mean femoral BMD of non-Hispanic white female aged 20 to 29 years from NHANES III was selected as the reference.15 OS was assessed separately in femur neck, trochanter, total femur, and intertrochanter. The overall OS was considered as OS in all of the femoral regions of interest.
HTN was defined in the seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure guideline.16 HTN was defined as systolic blood pressure of 140 mmHg (1 mmHg = 0.133 kpa) or diastolic blood pressure of 90 mmHg (1 mmHg = 0.133 kpa) or taking antihypertensive medication. Definitions of DASH, AHEI-2010, and MeDS are provided in Supplementary materials.
The outcome in this study was overall mortality. The average follow-up time was 84 months.
Interaction Measurements
The relative excess risk (RERI), synergy index (S) and attributable proportion (AP) were used to assess the additive and multiplicative interactions of OS and HTN on total mortality.17 RERI is equal to RR11-RR10-RR01+1, where RR is the relative risk, 1 represents the presence of an exposure factor, and 0 is the absence.18 AP equals the ratio of RERI to RR11 and refers to the proportion of disease in the exposure group that is attributable to the exposure. When the CI for RERI or AP did not contain 0, there was an additive effect. S denotes the multiplicative interaction, which is equal to RR11/(RR10×RR01).9 The multiplicative interaction is significant when the CI of S does not contain 1.
Statistical Analysis
Data missing interpolation were performed using a 5-imputation method. The normality of measurement data was evaluated via Shapiro–Wilk test. Of which, the data with normal distribution were assessed using independent samples t-test and described as mean (standard error, SE); the data without normal distribution were evaluated by Mann–Whitney U-test and described as median and quartiles [M(Q1, Q3)]. Enumeration data were assessed by Chi-square or Fisher’s exact probability tests and expressed as the number of cases and composition ratio N(%). The sociodemographic information was analyzed to screen the potential covariates using univariate COX regression analysis. Impacts of OS and HTN on the mortality were assessed using multivariate and univariate Cox proportional hazard models, with hazard ratios (HRs) and confidence intervals (CIs). Model I was a rough model without adjustment for any covariates. Model II had adjustment for age and sex. Model III had adjustment for age BMI, gender, marital status, ethnicity, alcohol consumption, education level, smoking, annual income, health insurance, diabetes history, and physical activity. Interaction of OS and HTN on the all-cause mortality was evaluated by the RERI, AP, and S. Then, the associations between DASH, MeDS, AHEI-2010 scores and all-cause mortality were investigated using COX regression analysis among individuals without OS and HTN, individuals with HTN only, individuals with OS only, and OS patients with HTN. The HR values were calculated after standardized processing. The subgroup analyses for the effects of various dietary scores on overall mortality were conducted for men, women and postmenopausal women. Two-tailed test was used for all statistical analyses. The results of all analyses were weighted except sensitivity test. SAS 9.4 (SAS Institute, Cary, NY, USA), R 4.20 (R Foundation, Vienna, Austria) and GraphPad 6.0 were performed for analyzing and drawing. P <0.05 was considered as statistical differences.
Results
Characteristics of 16,358 Participants
Data on 22,901 participants aged above 20 years were extracted. Participants with no information about HTN, survival status, and BMD were eliminated. Then, 16,358 participants were finally recruited into this cohort study, with an average of 48.67 (0.27) years and an average BMI of 28.04 (0.08) kg/m2. 8,370 (51.17%) were men, 7,788 (47.31%) were smoking, 5,857 had HTN, and 699 suffered from OS. A total of 1,383 adults died during follow-up, with a median follow-up time of 84.03 (64.07, 105.53) months. The characteristics of these participants were shown in Supplementary Table 1. The flow chart of participant screening was displayed in Figure 1.
Associations Between HTN, OS and All-Cause Mortality
The covariates screening of overall mortality is presented in Supplementary Table 2. When adjusted for age, gender, BMI, ethnicities, marital status, smoking, alcohol consumption, annual income, medical insurance, history of diabetes and physical activity, participants who had HTN had an increased mortality risk from all causes (HR=1.272, 95% CI: 1.083–1.494, P=0.004). OS was linked to higher mortality risk from all causes (HR=1.674, 95% CI: 1.262–2.221, P<0.001). The associations between HTN, OS and overall mortality are shown in Table 1.
 |
Table 1 Associations Between Hypertension, Osteoporosis and All-Cause Mortality |
The Interaction Between HTN and OS on All-Cause Mortality
Table 2 presents the interaction between HTN and OS on all-cause mortality. Patients with HTN without OS, with OS without HTN, with OS and HTN had 0.224, 0.409, 1.310 folds higher mortality risk from all causes than those without HTN and OS, respectively. The synergistic interaction between HTN and OS on all-cause mortality [RERI: 0.677 (95% CI: 0.070–1.285), AP: 0.293 (95% CI: 0.094–0.492), SI: 2.070 (95% CI: 1.124–3.813)]. Figure 2 shows the interaction of HTN and OS with all-cause mortality.
 |
Table 2 The Interaction Between Hypertension and Osteoporosis on All-Cause Mortality |
 |
Figure 2 The interaction of HTN and OS with all-cause mortality. (A) model 1; (B) model 2; (C) model 3. Abbreviations: HTN, hypertension; OS, osteoporosis. |
Associations Between DASH, MeDS, AHEI-2010 Scores and All-Cause Mortality Among Multi-Feature Populations
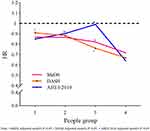
After adjusting the covariates, higher DASH scores were associated with lower mortality risk from all causes in hypertensive individuals with (HR=0.833, 95% CI: 0.796–0.981) or without (HR=0.670, 95% CI: 0.525–0.854) OS. Higher levels of adherence to MeDS were linked to a decreased likelihood of overall mortality in individuals without OS and HTN (HR=0.868, 95% CI: 0.773–0.975), hypertensive patients without OS (HR=0.866, 95% CI: 0.781–0.959), and individuals with OS and HTN (HR=0.717, 95% CI: 0.541–0.950). Elevated AHEI-2010 scores were linked to a decreased overall mortality risk in individuals without OS and HTN (HR=0.850, 95% CI: 0.754–0.959), and patients with OS and HTN (HR=0.641, 95% CI: 0.507–0.810). Table 3 and Figure 3 show the relationships of DASH, MeDS, and AHEI-2010 scores with all-cause mortality.
 |
Table 3 The Associations Between DASH, MeDS, AHEI-2010 Scores and All-Cause Mortality Among Multi-Feature Populations |
The Associations in Subgroups of Males, Females or Post-Menopause Women
The subgroups of males, females or post-menopause women were used to further assess the associations as shown in Table 4. For males, the relationships between DASH (HR=0.358, 95% CI: 0.233–0.550), MeDS (HR=0.462, 95% CI: 0.266–0.803), AHEI-2010 (HR=0.417, 95% CI: 0.277–0.629) scores and all-cause mortality were statistical differences in the Group IV. Similar results were found in the Group I, except that the relation between DASH score and overall mortality was marginal significance (HR=0.865, 95% CI: 0.744–1.006). For females, the DASH score was related to all-cause mortality in the Group II (marginal significance, HR=0.866, 95% CI: 0.748–1.002), III (HR=0.698, 95% CI: 0.512–0.950) and IV (HR=0.714, 95% CI: 0.544–0.936). The MeDS score was associated with overall mortality in the Group IV (HR=0.718, 95% CI: 0.516–0.999). The AHEI-2010 score was in connection with overall mortality in Groups II (HR=0.853, 95% CI: 0.735–0.991) and IV (HR=0.654, 95% CI: 0.504–0.849).
 |
Table 4 Associations Between DASH, MeDS, AHEI-2010 Scores and All-Cause Mortality |
In post-menopause women, the connections between high DASH scores and decreased odds of overall mortality were established in Groups III (HR=0.684, 95% CI: 0.494–0.946) and IV (HR=0.741, 95% CI: 0.555–0.989). The relationships of AHEI-2010 with overall mortality were discovered in Groups II (HR=0.824, 95% CI: 0.714–0.951) and IV (HR=0.673, 95% CI: 0.511–0.885).
Discussion
In this cohort study with a large population (16,358 participants), we explored the interaction of OS and hypertension on the all-mortality, and further assessed the association between different dietary patterns (MeDS, AHEI-2010, and DASH) and all-cause mortality among multi-feature population, including adults with HTN or OS only, and adults with or without OS and HTN. Participants who had HTN or OS had higher overall mortality risk. We found that HTN and OS interacted to affect overall mortality. The AHEI-2010, MeDS, and DASH were linked to overall mortality in individuals with HTN complicated with OS.
Higher adherence to MeDS was linked to reduced overall mortality risk in the whole cohort who had OS and HTN. This finding was consistent across the groups of males and females, different from post-menopause women. Previous studies have shown that higher MeDS adherence is linked to a better survival.19,20 Whether the survival edge is maintained in people with different characteristics is not yet clear. Regarding the components of MeDS, increased intakes of nuts, fruits, whole grains, or vegetables were concerned with a decline in overall mortality risk.
Studies have shown that lipid metabolism may be involved in the development of osteoporosis,21,22 this may be a potential mechanism for the interaction between hypertension and osteoporosis. In addition, studies have shown that the activation of the local renin–angiotensin system in bone tissue can lead to increased bone resorption, leading to osteoporosis, which is also a possible way for osteoporosis and hypertension to interact.23,24 Previous studies have shown that hormone levels, histone modifications, dairy intake, diabetes, calcium and phosphorus metabolism in the body are closely related to hypertension and osteoporosis.25–31 There are also some studies that provide different results: Amirkhanlou et al found that osteoporosis has a lower incidence in patients with hypertension, and Laure Rouch et al and Michael et al have similar results.32–34
The DASH diet has played a role in blood pressure reduction, which was originally introduced for the HTN treatment in the 1990s.35,36 Strict DASH diet adherence may contribute to survival improval.37 High DASH scores were linked to reduced odds of overall mortality in hypertensive adults.38 However, no relationship was found between the DASH score and the risk of death from all causes in the general public.39 DASH adherence was low among the general public,39 even among hypertensive patients.40 Similar results were discovered in our study. It was indicated that high DASH maintenance might be beneficial to the health management of chronic diseases.37 For the DASH components, elevated fiber, magnesium, or potassium intakes were linked to a reduction overall mortality risk.
The AHEI was based on large epidemiological studies for the prevention of noncommunicable diseases.41 Though the HEI and AHEI diet scores had slightly different aims, they both emphasize high consumption of fruits, vegetables, monounsaturated fat, legumes, whole grains, with recommendations to reduce consumption of saturated fatty acids, added sugars, refined grains, and sodium associated with increased HTN risk.42 A diet rich in fiber, low energy density, and low glycemic load protects against HTN.43 The beneficial effects of vegetables/fruits on HTN could be attributed to phytochemicals,44 vitamins,45 Mg, and K46 and antioxidants,47 which are independently linked to blood pressure reduction. Eating nuts and soya, and drinking alcohol in moderation, appeared to be the most independently powerful contributors to decrease mortality.48 What makes the MED diet unique and distinctive is the relatively high use of nuts, olive oil and moderate use of red wine at mealtimes.49 High compliance with the MeDS diet has also been reported to reduce blood pressure.50,51
Dietary studies have shown that specific dietary patterns have a significant effect on reducing the risk of death, mainly by regulating inflammation, improving blood lipid and blood glucose management, controlling blood pressure and bone health. Specific dietary patterns, such as the Mediterranean diet and the DASH diet, have been extensively studied and shown to reduce all-cause mortality and the risk of death from specific diseases (such as cardiovascular disease). The Mediterranean diet and DASH diet, which are rich in antioxidants and anti-inflammatory foods, help to reduce the inflammatory response in the body.52–55 By inhibiting oxidative stress and inflammatory responses, these dietary patterns help reduce the risk of chronic diseases such as diabetes and cardiovascular disease. The DASH diet is specifically designed to reduce high blood pressure by reducing sodium intake and increasing potassium, magnesium and calcium intake.56–58 Mediterranean diet rich in monounsaturated fatty acids helps reduce low-density lipoprotein (LDL) levels and increase high-density lipoprotein (HDL) levels.59–62 In addition, these dietary patterns are also rich in dietary fiber, which helps to control blood glucose levels, reduce insulin resistance, and reduce the risk of metabolic syndrome and type 2 diabetes. The Mediterranean diet and the DASH diet are rich in nutrients needed for bone health to help maintain bone mineral density and prevent osteoporosis.63–69
Although adjustment was made for socio-economic variables and chronic diseases, disease condition and treatment during follow-up were hard to adjust for. Dietary information was collected by a continuous 24-hour dietary recall using questionnaires. Long-term adherence to the dietary patterns was not addressed. The single components of dietary scores were not further assessed in this study, which may be beneficial for making dietary decisions. Our findings may give some hints for dietary recommendations for multi-feature individuals. Considering that diet data mainly relying on self-reporting can introduce recall bias, and the impact of treatment on HTN and OS during follow-up may confuse the results; future well-designed studies with long-term observation are essential.
Conclusion
This study explored the associations of different dietary patterns with all-cause mortality among multi-feature population. The MeDS, AHEI-2010 and DASH were all associated with overall mortality in individuals with OS and HTN. The MeDS and DASH were concerned with all-cause mortality in HTN patients without OS. The MeDS and AHEI-2010 were linked to overall mortality for adults without OS and HTN. The impacts of different dietary patterns were differences in multi-feature population. It was suggested that reasonable dietary management is beneficial to the prognosis of different populations.
Data Sharing Statement
The datasets used and/or analysed during the current study were publicly available from the NHANES database.
Ethics Approval and Consent to Participate
Not applicable, because NHANES belongs to public databases, the patients involved in the database have obtained ethical approval, users can download relevant data for free for research and publish relevant articles, and our study is based on open-source data, and the South Hospital of the Sixth People’s Hospital Affiliated to Shanghai University of Medicine & Health Sciences (Shanghai Fengxian District Central Hospital) do not require research using publicly available data to be submitted for review to their ethics committee, so there are no ethical issues and other conflicts of interest.
Consent for Publication
Not applicable, because this paper did not reveal any personal information of patients.
Acknowledgments
Jianhua Guan, Liang Ding, Yifei Wang and Zhongsheng Zhu are co-first authors for this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Key Project of the Diagnosis and Treatment Center of Shanghai Fengxian District (No. fxlczlzx-a-201704).
Disclosure
All authors declare that they have no conflicts of interest for this work.
References
1. Liu Z, Lee HL, Suh JS, et al. The ERα/KDM6B regulatory axis modulates osteogenic differentiation in human mesenchymal stem cells. Bone Res. 2022;10(1):3. doi:10.1038/s41413-021-00171-z
2. Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393(10169):364–376. doi:10.1016/s0140-6736(18)32112-3
3. Hollenberg NK. Hypertension, small arteries, and pathways for angiotensin II generation: “The proper study of mankind is man”. Circulation. 2000;101(14):1641–1642. doi:10.1161/01.cir.101.14.1641
4. Ohashi K, Ouchi N, Matsuzawa Y. Adiponectin and hypertension. Am J Hypertens. 2011;24(3):263–269. doi:10.1038/ajh.2010.216
5. Martinez R, Lloyd-Sherlock P, Soliz P, et al. Trends in premature avertable mortality from non-communicable diseases for 195 countries and territories, 1990-2017: a population-based study. Lancet Glob Health. 2020;8(4):e511–e523. doi:10.1016/s2214-109x(20)30035-8
6. Chen H, Dhana K, Huang Y, et al. Association of the Mediterranean dietary approaches to stop hypertension intervention for neurodegenerative delay (MIND) diet with the risk of dementia. JAMA psychiatry. 2023;80(6):630–638. doi:10.1001/jamapsychiatry.2023.0800
7. Morze J, Danielewicz A, Hoffmann G, Schwingshackl L. Diet quality as assessed by the healthy eating index, alternate healthy eating index, dietary approaches to stop hypertension score, and health outcomes: a second update of a systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2020;120(12):1998–2031.e1915. doi:10.1016/j.jand.2020.08.076
8. Shan Z, Wang F, Li Y, et al. healthy eating patterns and risk of total and cause-specific mortality. JAMA Intern Med. 2023;183(2):142–153. doi:10.1001/jamainternmed.2022.6117
9. Soltani S, Arablou T, Jayedi A, Salehi-Abargouei, A. Adherence to the dietary approaches to stop hypertension (DASH) diet in relation to all-cause and cause-specific mortality: a systematic review and dose-response meta-analysis of prospective cohort studies.Nutrition. Journal. 2020;19(1):37. doi:10.1186/s12937-020-00554-8
10. Luong R, Ribeiro R, Naganathan V, Blyth F, Waite LM, Handelsman DJ, Le Couteur DG, Seibel MJ, Hirani VEmpirically derived dietary patterns are associated with major adverse cardiovascular events, all-cause mortality, and congestive cardiac failure in older men: the concord health and ageing in men project. Journal of nutrition, health and aging. J Nutr, Health & Aging. 2024;28(2):100020. doi:10.1016/j.jnha.2023.100020
11. Steinberg FM, Batchelor-Murphy MK, Heather M. Young.Eating for Healthy Aging.The. supporting family caregivers: no longer home alone: eating for healthy aging. Am J Nurs. 2019;119(11):43–51. doi:10.1097/01.NAJ.0000605360.22194.1f
12. Huang Y, Ye J. Association between hypertension and osteoporosis: a population-based cross-sectional study. BMC Musculoskelet Disord. 2024;25(1):434. doi:10.1186/s12891-024-07553-4
13. Cho H-W, Jin H-S, Eom Y-B. FGFRL1 and FGF genes are associated with height, hypertension, and osteoporosis. PLoS One. 2022;17(8):e0273237. doi:10.1371/journal.pone.0273237
14. Canoy D, Harvey NC, Prieto-Alhambra D, et al. Rahimi.Elevated blood pressure, antihypertensive medications and bone health in the population: revisiting old hypotheses and exploring future research directions.Osteoporosis International. 2022;33(2):315–326. doi:10.1007/s00198-021-06190-0
15. Guo J, Huang Y, Bian S, et al. Associations of urinary polycyclic aromatic hydrocarbons with bone mass density and osteoporosis in U.S. In: Adults, NHANES 2005-2010. Environmental Pollution. Vol. 240;2018:209–218. doi:10.1016/j.envpol.2018.04.108
16. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi:10.1001/jama.289.19.2560
17. Knol MJ, VanderWeele TJ, Groenwold RH, Klungel OH, Rovers MM, Grobbee DE. Estimating measures of interaction on an additive scale for preventive exposures. Eur j epidemiol. 2011;26(6):433–438. doi:10.1007/s10654-011-9554-9
18. Chu H, Nie L, Cole SR. Estimating the relative excess risk due to interaction: a Bayesian approach. Epidemiology. 2011;22(2):242–248. doi:10.1097/EDE.0b013e318208750e
19. Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. New Engl J Med. 2003;348(26):2599–2608. doi:10.1056/NEJMoa025039
20. Trichopoulou A, Bamia C, Trichopoulos D. Anatomy of health effects of Mediterranean diet: Greek EPIC prospective cohort study. BMJ. 2009;338:b2337. doi:10.1136/bmj.b2337
21. Sun J, Pan Y, Li X, et al. Quercetin attenuates osteoporosis in orchiectomy mice by regulating glucose and lipid metabolism via the gprc6a/AMPK/mtor signaling pathway. Front Endocrinol. 2022;13:849544. doi:10.3389/fendo.2022.849544
22. Kan B, Zhao Q, Wang L, Xue S, Cai H, Yang S. Association between lipid biomarkers and osteoporosis: a cross-sectional study. BMC Musculoskelet Disord. 2021;22(1):759. doi:10.1186/s12891-021-04643-5
23. Zhao J, Yang H, Chen B, Zhang R. The skeletal renin-angiotensin system: a potential therapeutic target for the treatment of osteoarticular diseases. Int Immunopharmacol. 2019;72:258–263. doi:10.1016/j.intimp.2019.04.023
24. Kim KM, Hwang EJ, Lee S, Yoon J-H. The impact of renin-angiotensin system inhibitors on bone fracture risk: a nationwide nested case-control study. BMC Musculoskelet Disord. 2024;25(1):10.1186/s12891–023–07102–5. doi:10.1186/s12891-023-07102-5
25. Veronese N, Stubbs B, Crepaldi G, et al. Relationship between low bone mineral density and fractures with incident cardiovascular disease: a systematic review and meta-analysis. J Bone Miner Res. 2017;32(5):1126–1135. doi:10.1002/jbmr.3089
26. Varenna M, Manara M, Galli L, Binelli L, Zucchi F, Sinigaglia L. The association between osteoporosis and hypertension: the role of a low dairy intake. Calcif Tissue Int. 2013;93(1):86–92. doi:10.1007/s00223-013-9731-9
27. Tan YQ, Ng DX, Gunasekaran K, Lim WL, Tan NC. Clinical characteristics and risk factors of osteoporosis among older Asian men with type-2 diabetes mellitus, hypertension, or hyperlipidaemia. Arch Osteoporos. 2024;19(1):10.1007/s11657–024–01442–y.
28. Sun P, Huang T, Huang C, Wang Y, Tang D. Role of histone modification in the occurrence and development of osteoporosis. Front Endocrinol. 2022;13:964103. doi:10.3389/fendo.2022.964103
29. Hu R, Chen L, Chen X, Xie Z, Xia C, Chen Y. Aloperine improves osteoporosis in ovariectomized mice by inhibiting RANKL-induced NF-κB, ERK and JNK approaches. Int Immunopharmacol. 2021;97:107720. doi:10.1016/j.intimp.2021.107720
30. Do Carmo L, Harrison DG. Hypertension and osteoporosis: common pathophysiological mechanisms. Med Nov Technol Devices. 2020;8:100047. doi:10.1016/j.medntd.2020.100047
31. Chai H, Ge J, Li L, Li J, Ye Y. Hypertension is associated with osteoporosis: a case-control study in Chinese postmenopausal women. BMC Musculoskelet Disord. 2021;22(1):10.1186/s12891–021–04124–9.
32. Amirkhanlou S, Roshandel G, Aghaei M, et al. Assessment of bone mineral density in patients undergoing hemodialysis; an Iranian population-based study. Arch Iran Med. 2021;24(8):599–606. doi:10.34172/aim.2021.85
33. Rouch L, Rolland Y, Hanon O, et al. Blood pressure, antihypertensive drugs, and incident frailty: the multidomain Alzheimer preventive trial (MAPT). Maturitas. 2022;162:
34. Mussolino ME, Gillum RF. Bone mineral density and hypertension prevalence in postmenopausal women: results from the third national health and nutrition examination survey. Ann Epidemiol. 2006;16(5):395–399. doi:10.1016/j.annepidem.2005.06.051
35. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Res Group New Eng J Med. 1997;336(16):1117–1124. doi:10.1056/nejm199704173361601
36. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. New Engl J Med. 2001;344(1):3–10. doi:10.1056/nejm200101043440101
37. Folsom AR, Parker ED, Harnack LJ. Degree of concordance with DASH diet guidelines and incidence of hypertension and fatal cardiovascular disease. Am J Hypertens. 2007;20(3):225–232. doi:10.1016/j.amjhyper.2006.09.003
38. Parikh A, Lipsitz SR, Natarajan S. Association between a DASH-like diet and mortality in adults with hypertension: findings from a population-based follow-up study. Am J Hypertens. 2009;22(4):409–416. doi:10.1038/ajh.2009.10
39. Beydoun HA, Huang S, Beydoun MA, Hossain S, Zonderman AB. Mediating-moderating effect of allostatic load on the association between dietary approaches to stop hypertension diet and all-cause and cause-specific mortality: 2001-2010 national health and nutrition examination surveys. Nutrients. 2019;11(10):2311. doi:10.3390/nu11102311
40. Mellen PB, Gao SK, Vitolins MZ, Goff DC. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Archives of Internal Medicine. 2008;168(3):308–314. doi:10.1001/archinternmed.2007.119
41. Hlaing-Hlaing H, Dolja-Gore X, Tavener M, James EL, Hure AJ. alternative healthy eating index-2010 and incident non-communicable diseases: findings from a 15-year follow up of women from the 1973-78 cohort of the Australian longitudinal study on women’s health. Nutrients. 2022;14(20):4403. doi:10.3390/nu14204403
42. Xu Z, Steffen LM, Selvin E, Rebholz CM. Diet quality, change in diet quality and risk of incident CVD and diabetes. Public Health Nutrition. 2020;23(2):329–338. doi:10.1017/s136898001900212x
43. Alissa EM, Ferns GA. Dietary fruits and vegetables and cardiovascular diseases risk. Critical reviews in food science and nutrition. Critical Rev Food Sci Nutr. 2017;57(9):1950–1962. doi:10.1080/10408398.2015.1040487
44. Tain YL, Hsu CN. Novel insights on dietary polyphenols for prevention in early-life origins of hypertension: a review focusing on preclinical animal models. Int J Mol Sci. 2022;23(12):6620. doi:10.3390/ijms23126620
45. Lee Y, Park S. Serum folate levels and hypertension. Sci Rep. 2022;12(1):10071. doi:10.1038/s41598-022-13978-5
46. Cheteu Wabo TM, Wu X, Sun C, et al. Association of dietary calcium, magnesium, sodium, and potassium intake and hypertension: a study on an 8-year dietary intake data from the national health and nutrition examination survey. Nutr Res Pract. 2022;16(1):74–93. doi:10.4162/nrp.2022.16.1.74
47. Colon Hidalgo D, Elajaili H, Suliman H, George MP, Delaney C, Metabolism NE. Mitochondrial dysfunction, and redox homeostasis in pulmonary hypertension. Antioxidants. 2022;11(2):428. doi:10.3390/antiox11020428
48. Akbaraly TN, Ferrie JE, Berr C, et al. Alternative healthy eating index and mortality over 18 y of follow-up: results from the Whitehall II cohort. Am J Clin Nutr. 2011;94(1):247–253. doi:10.3945/ajcn.111.013128
49. Guasch-Ferré M, Willett WC. The Mediterranean diet and health: a comprehensive overview. J Internal Med. 2021;290(3):549–566. doi:10.1111/joim.13333
50. Toledo E, Hu FB, Estruch R, et al. Effect of the Mediterranean diet on blood pressure in the PREDIMED trial: results from a randomized controlled trial. BMC Med. 2013;11(207). doi:10.1186/1741-7015-11-207
51. Davis CR, Hodgson JM, Woodman R, Bryan J, Wilson C, Murphy KJ. A Mediterranean diet lowers blood pressure and improves endothelial function: results from the MedLey randomized intervention trial. Am J Clin Nutr. 2017;105(6):1305–1313. doi:10.3945/ajcn.116.146803
52. Cheng E, Um CY, Prizment A, Lazovich D, Bostick RM. Associations of evolutionary-concordance diet, Mediterranean diet and evolutionary-concordance lifestyle pattern scores with all-cause and cause-specific mortality. Br J Nutr. 2018;1–10. doi:10.1017/S0007114518003483
53. Mostafa MA, Skipina T, Anees MA, Soliman EZ, Ahmad MI. Association of empirical dietary inflammatory potential with mortality: results from the third national nutrition examination survey. J Res Health Sci. 2023;23(2):e00578. doi:10.34172/jrhs.2023.113
54. Norde MM, Collese TS, Giovannucci E, Rogero MM. A posteriori dietary patterns and their association with systemic low-grade inflammation in adults: a systematic review and meta-analysis. Nutr Rev. 2021;79(3):331–350. doi:10.1093/nutrit/nuaa010
55. Lyu L, Yu J, Liu Y, et al. Dietary patterns, oxidative stress, inflammation and biological variation in hemoglobin a1c: association and mediation analysis in a rural community in north China. Diabetes Res Clin Pract1. 2022;194:110154. doi:10.1016/j.diabres.2022.110154
56. Morton KF, Scheinuk JE, Bowman S, et al. Association between dietary patterns and incident hypertension in REGARDS (REasons for geographic and regional differences in stroke) participants. Am J Hypertens. 2025. doi:10.1093/ajh/hpaf063
57. Lu X, Wang J, Chen S, Lv L, Yu J. Analysis of ADHERENCE STATUS AND INFLUENCING FACTORS AMONG MIDDLE-AGED AND ELDERLY HYPERTENSION PATIEnts in Rural Areas of Northeast China. Int J Hypertens. 2025;2025:9954099. doi:10.1155/ijhy/9954099
58. Hasan F, Singh A, Garcia A, et al. Evaluating the impact of the Dietary Approaches to Stop Hypertension diet versus a calorie-restricted diet on metabolic dysfunction-associated steatotic liver disease: a meta-analysis of randomized controlled trials. Hepatol Res. 2025;55(4):515–526. doi:10.1111/hepr.14155
59. Tosti V, Bertozzi B, Fontana L. Health benefits of the Mediterranean diet: metabolic and molecular mechanisms. J Gerontol a Biol Sci Med Sci. 2018;73(3):318–326. doi:10.1093/gerona/glx227
60. Sjögren P, Becker W, Warensjö E, et al. Mediterranean and carbohydrate-restricted diets and mortality among elderly men: a cohort study in Sweden. Am J Clin Nutr. 2010;92(4):967–974. doi:10.3945/ajcn.2010.29345
61. Perrone P, D’Angelo S. Gut microbiota modulation through Mediterranean diet foods: implications for human health. Nutrients. 2025;17(6):948. doi:10.3390/nu17060948
62. Cheng F-Y, Chen C, Wang F-Y, Zhao B-H. Combining nutraceuticals and a Mediterranean diet for managing metabolic dysfunction associated with steatotic liver disease. World J Hepatol. 2025;17(4):104622. doi:10.4254/wjh.v17.i4.104622
63. Biver E, Herrou J, Larid G, et al. Dietary recommendations in the prevention and treatment of osteoporosis. Joint Bone Spine. 2023;90(3):105521. doi:10.1016/j.jbspin.2022.105521
64. Andreo-López MC, Contreras-Bolívar V, García-Fontana B, García-Fontana C, Muñoz-Torres M. The influence of the Mediterranean dietary pattern on osteoporosis and sarcopenia. Nutrients. 2023;15(14):3224. doi:10.3390/nu15143224
65. Quattrini S, Pampaloni B, Gronchi G, Giusti F, Brandi ML. The Mediterranean diet in osteoporosis prevention: an insight in a peri- and post-menopausal population. Nutrients. 2021;13(2):531. doi:10.3390/nu13020531
66. Shahriarpour Z, Nasrabadi B, Shariati-Bafghi S-E, Karamati M, Rashidkhani B. Adherence to the dietary approaches to stop hypertension (DASH) dietary pattern and osteoporosis risk in postmenopausal Iranian women. Osteoporos Int. 2020;31(11):2179–2188. doi:10.1007/s00198-020-05450-9
67. Qiu H, Yu IT, Wang XR, Fu ZM, Tse SL. [Study on the interaction under logistic regression modeling]. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi. 2008;29(9):934–937.
68. Noel SE, Mangano KM, Mattei J, et al. Dietary approaches to stop hypertension, Mediterranean, and alternative healthy eating indices are associated with bone health among Puerto Rican adults from the Boston Puerto Rican osteoporosis study. Am J Clin Nutr. 2020;111(6):1267–1277. doi:10.1093/ajcn/nqaa090
69. Ozemek C, Laddu DR, Arena R, Lavie CJ. The role of diet for prevention and management of hypertension. Current Opinion Cardiol. 2018;33(4):388–393. doi:10.1097/hco.0000000000000532
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Age-Dependent Association Between Body Mass Index and All-Cause Mortality Among Patients with Hypertension: A Longitudinal Population-Based Cohort Study in China
Huang Y, Peng J, Wang W, Zheng X, Qin G, Xu H
Clinical Epidemiology 2023, 15:1159-1170
Published Date: 7 December 2023
Relationship Between Body Composition and Hypertension in Postmenopausal Women with Osteoporosis—A Single-Center Cross-Sectional Study
Jiang S, Fu Y, Chen L, Qiu Y
Diabetes, Metabolic Syndrome and Obesity 2025, 18:1587-1598
Published Date: 14 May 2025